In patients with single hepatocellular carcinoma (HCC) >5cm and preserved liver function, surgery is the treatment option that offers the greatest benefit in terms of survival, although it is associated with very high recurrence figures (70% at 5 years).1 Sometimes, tumour size and its vascular relationships compromise the surgical margin, and the prior use of local regional treatments facilities resectability. Nevertheless, the possibility of a subsequent relapse continues to be high. At this moment in time, a great deal of research is being conducted in the field of adjuvant treatment to surgery with systemic treatments, with a view to reducing these recurrences; nevertheless, the use of a neoadjuvant strategy is also very attractive, and its role has yet to be elucidated.
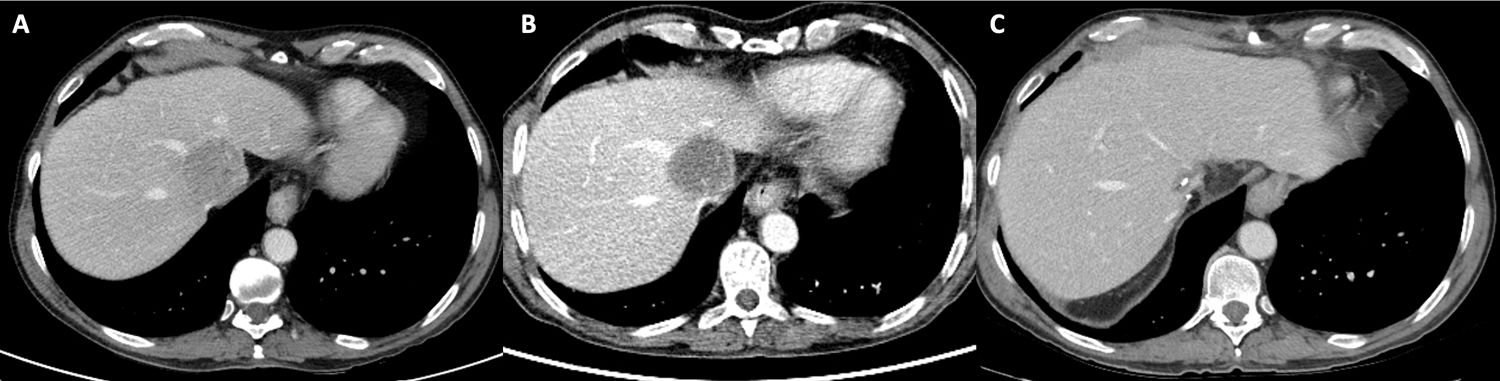
We present the case of a 65-year-old patient with treated HCV infection, diagnosed with a 64-mm HCC(BCLC stage A) in segment I in contact with the vena cava, left portal vein and middle and left suprahepatic veins (Fig. 1A). The patient had elevated α-fetoprotein (AFP) (620μg/l) with preserved liver function (Child A 5 points). The patient was initially regarded as an ideal candidate for surgery with a hepatic venous pressure gradient of 3mm Hg and favourable indocyanine green clearance (PDR: 21 and R15: 0.9). The complexity of the vascular relationships that compromised the possibility of R0 resection, together with extremely elevated AFP levels, led us to first consider a neoadjuvant strategy with transarterial radioembolisation (TARE), intended to improve the vascular resection margin. However, technical difficulties emerged in the planning with regard to addressing the tumour’s arterial afferents, leading the TARE to be replaced by DCBeads transarterial chemoembolisation (TACE), after which the patient developed a prolonged post-embolisation syndrome with transient liver function impairment. The CT scan performed one month after TACE showed a partial radiological response according to the modified RECIST criteria, with a significant reduction in the lesion's uptake of contrast (Fig. 1B), together with a marked reduction in AFP (33μg/l), albeit without a reduction in size or improvement of the margin. Following assessment by the multidisciplinary committee, TACE was regarded as the best procedure, which could not be bettered and had a high risk of new complications. The decision was taken to switch to systemic treatment, and lenvatinib at a dose of 8mg/24h was initiated for two months and maintained up until 10 days prior to the surgery, thereby normalising AFP levels. After five months of neoadjuvant strategy, parenchyma-'sparing' anatomical surgery was performed, segment I segmentectomy, permitting adequate cutting on the wall of the suprahepatic veins and the left portal vein without the need for major hepatectomy. Pathology was reported as a moderately differentiated HCC with extensive tumour necrosis (<10% of residual activity), with no microscopic vascular invasion and free margins. The postoperative period was uneventful, and the patient was discharged on the third day. The follow-up CT scan one and half months later showed vascular permeability without the presence of residual tumour (Fig. 1C). After 10 months of follow-up, the patient is tumour relapse-free.
(A) Pre-treatment index CT scan. HCC closely related to the middle and left suprahepatic veins. (B) Post-TACE PET-CT scan. Absence of metabolic uptake in the HCC with slightly hypermetabolic margins. (C) Post-surgical follow-up CT after one and a half months. Vascular permeability in the suprahepatic veins, with no residual tumour.
In large HCC associated with other data indicating a poor prognosis, post-surgical relapses are common. In these circumstances, although adjuvant treatment strategies are being evaluated, the concept of performing neoadjuvant treatment is also interesting, although the scenarios in which it would be most suitable have yet to be defined. In our case, besides the size, the tumour’s vascular relationships led us to perform prior local regional treatment in an attempt to improve the cancer margin. Our first option was to use TARE, which was ruled out on account of technical problems, whereupon the procedure was changed to TACE. The pre-surgical TACE strategy is well-known, and there are studies demonstrating that the subsequent radiological response, as was the case in our patient, is the main prognostic factor associated with survival.2 Despite the favourable response to TACE, we felt that we needed more time to evaluate the tumour's biological behaviour. The onset of post-embolisation syndrome with impaired liver function led us to consider, rather than repeating TACE, systemic lenvatinib treatment for a further two months instead of sorafenib due to its greater antiangiogenic effect, since in post-TACE recurrence, stimulating neovascularisation in the peripheral area of the treated tumour plays a major role. Several phase 3 trials are currently assessing adjuvant treatment to surgery in HCC with an intermediate-high risk of relapse, although none of them as a neoadjuvant option. This dual strategy may improve the resectability rate and makes it possible to select the HCC subgroup with the most favourable biological behaviour over time, associated with better survival and fewer relapses. In our case, the combination of TACE and lenvatinib proved to be safe, did not increase perioperative morbidity and allowed us to test the tumour’s biology, facilitating resection with adequate cancer margins. Recently, similar neoadjuvant treatment strategies with lenvatinib with downstaging intent that permit subsequent salvage with surgery have been reported.3–5
While we await clinical trials that clarify the impact on overall survival and recurrence, the use of a combined neoadjuvant treatment strategy may be an attractive, feasible and safe option in HCC with complex intrahepatic vascular relationships and data suggesting poor prognosis at diagnosis
FundingNo funding was received for this study.
Conflicts of interestArturo Colón: consultant with Sirtex.
Ana Matilla: conferences with Boston, EISAI/MSD and SIRTeX, consultant with Sirtex and EISAI/MSD.
Please cite this article as: Colón Rodríguez A, Velasco Sánchez E, Rodríguez-Bachiller L, Díaz-Zorita B, López Baena JÁ, Álvarez Luque A, et al. Estrategia combinada de neoadyuvancia a cirugía con quimioembolizació n y lenvatinib en carcinoma hepatocelular. Gastroenterol Hepatol. 2022;96:490–491.