Jejunal diverticulitis is a very uncommon acquired pathology, with an incidence of 0.3%–1%.1 The diverticula are located on the mesenteric face of the proximal jejunum in 75% of cases, the distal jejunum in 20% and the ileum in 5%.1
We present a case of perforated jejunal diverticulitis as a rare cause of acute abdominal pain and highlight the importance in this condition of having high clinical suspicion in order to diagnose and treat it early.
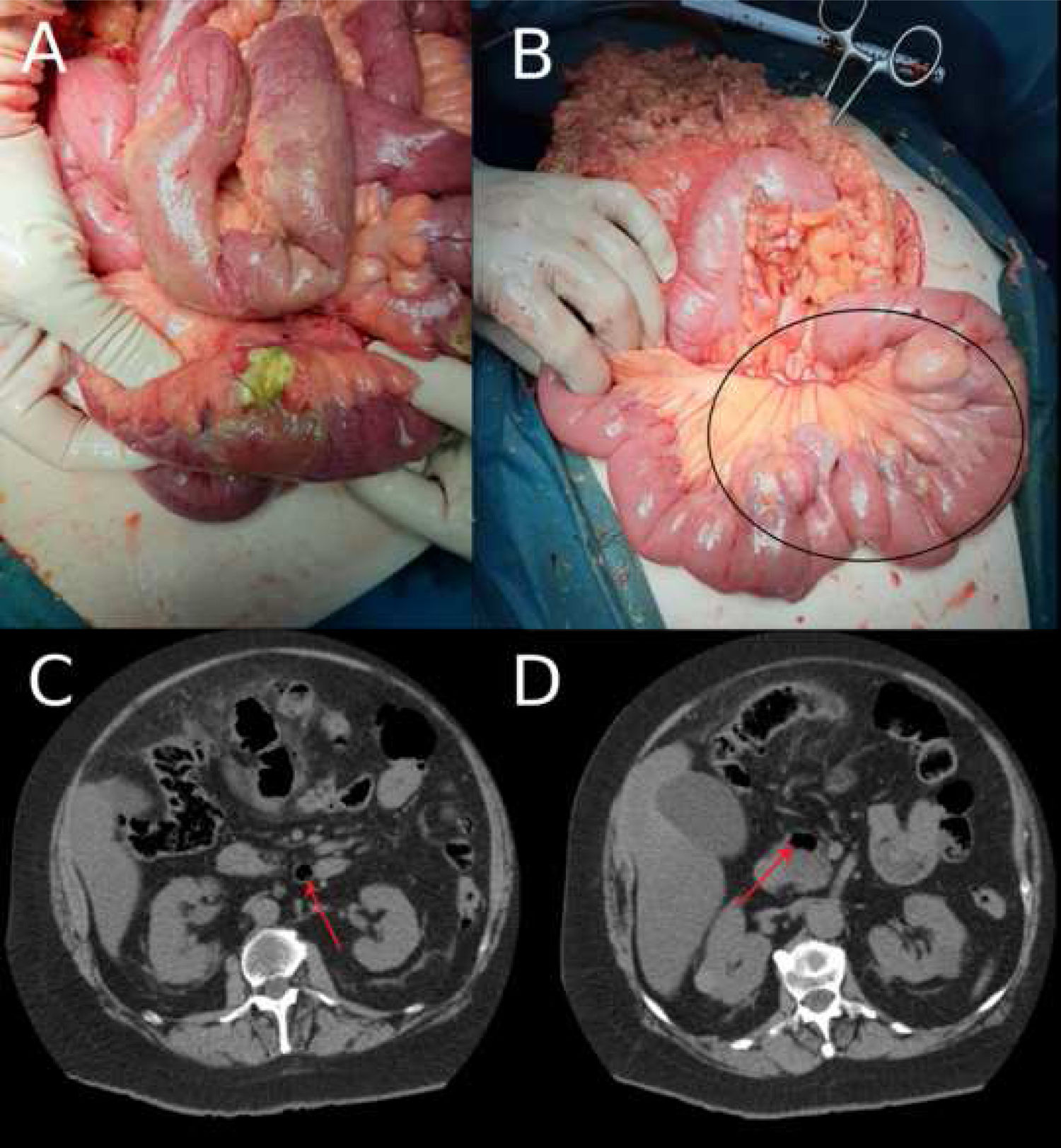
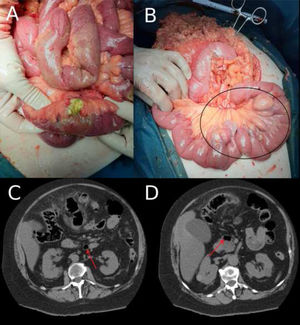
A 66-year-old woman who attended the Emergency Department due to colic-type abdominal pain in the epigastric region of four days’ evolution, with associated nausea and vomiting. She presented a fever of 38 °C, and in the physical examination the abdomen was soft and depressible, with diffuse pain to palpation. Blumberg’s sign was positive. The analysis revealed leukocytosis (15.9 × 109/l) and elevated C-reactive protein (CRP) (3.3 mg/dl). Abdominal and pelvic computed tomography (CT) was performed, finding pneumoperitoneum, intra-pelvic free fluid and increased mesenteric fat density in the left hemiabdomen. Diverticulosis was also found in the sigmoid colon. The patient’s initial diagnosis was perforated sigmoid diverticulitis, and the decision was made to perform emergency surgical treatment. Intraoperatively, disseminated peritonitis was observed in all quadrants with inter-loop collections and multiple jejunal diverticula (10 diverticula distributed in the jejunum, beginning immediately distal to the duodenojejunal flexure) with a large perforation of one diverticulum on the mesenteric face of the jejunum at 80 cm from the duodenojejunal flexure (Fig. 1). The jejunal fragment with the perforated diverticulum was resected and termino-terminal (T-T) mechanical anastomosis carried out. The postoperative period was without incident and the patient was discharged on day seven after the procedure. On reviewing the CT following the surgery, it was possible to identify the diverticula (Fig. 1B). Subsequently, the anatomopathological study confirmed jejunal diverticular disease with perforation, as well as marked inflammation of the intestinal mesentery.
1A) Intraoperative image: perforation of a single large distal jejunal diverticulum. 1B) Intraoperative image: multiple large jejunal diverticula, on the mesenteric face, from practically the duodenojejunal flexure to 80 cm from the same (black circle). 1C and 1D) Abdominal and pelvic CT image, axial view. The image shows the jejunal diverticula (red arrows).
Jejunoileal diverticulosis was first described by Sömmering in 1794 as a herniation of the mucosa and submucosa on the mesenteric face of the wall of the small intestine, through the muscular layer (pseudodiverticulum).2 Its aetiology is unknown and it is believed to be caused by a combination of abnormal peristalsis, intestinal dyskinesia and an increase in pressure.3 These diverticula generally occur in conjunction with other diverticula that coexist in other locations, such as the colon in up to 75% of cases,3 as occurred in our patient.
Jejunal diverticulosis is often asymptomatic; just 29% of patients develop nonspecific symptoms such as chronic postprandial abdominal discomfort, flatulence, diarrhoea, malabsorption or steatorrhoea, which can easily lead to an erroneous diagnosis and necessitates a high degree of clinical suspicion.1,3 Some 10% develop complications such as bowel obstruction, peritonitis, lower gastrointestinal haemorrhage or perforation, the latter being a serious complication that occurs in 2%–6% of cases.3
Diagnosis is often challenging, as although computed tomography is the best imaging method to diagnose complicated jejunal diverticulosis, on up to 75% of occasions imaging tests are not initially diagnostic and the diagnosis is obtained intraoperatively,3 as occurred in our patient.
The majority of complications of jejunal diverticulosis require surgical treatment. Although conservative management of a perforated jejunal diverticulum can be carried out in stable patients who present localised abdominal signs and symptoms,4 surgical exploration with segmental resection and primary anastomosis is the cornerstone of treatment.5 Alternative surgical procedures such as primary closure, diverticulectomy or invagination are associated with extremely poor results and high mortality rates, and so should be avoided.5
Due to poor prognostic factors, such as advanced age and delays in diagnosis and treatment, mortality due to jejunal diverticulitis varies from 0% to 5%, increasing to 40% in the event of perforation.1,5
In conclusion, given the low incidence of jejunal diverticula, their nonspecific clinical picture and the low sensitivity of imaging tests, they are often an incidental finding during surgery and confused with other pathologies, as in our case, which may delay the treatment of this condition.
Please cite this article as: Santos Rancaño R, Delgado Morales M, Hernández García M, Cerdán Santacruz C, Buendía Pérez E, Alonso Guillén R. Diverticulitis yeyunal perforada: una causa rara de abdomen agudo. Gastroenterol Hepatol. 2021;44:563–564.