We present the case of a 48-year-old man with a personal history of non-Hodgkin lymphoma (mucosa-associated lymphoid tissue [MALT]-type) with intestinal involvement, diagnosed in 2004 and treated with chemotherapy. The patient has remained in remission since then.
The patient attended our clinic with a 3-month history of progressive dysphagia, chest pain irradiating to the back and weight loss of 10kg. Findings for a gastroscopy were normal, while a barium swallow test revealed a 3-cm stenosis at the level of the gastro-oesophageal junction with no mass effect, suggesting incipient achalasia. The oesophageal body was normal in calibre, with no dilation or air-fluid level. Four-channel perfusion oesophageal manometry was performed in decubitus. The upper oesophageal sphincter was located at between 25.3cm and 20cm from the nasal ala and had a slightly increased resting pressure and normal function. Good pharyngo-oesophageal coordination was observed. The oesophageal body study with at least 10 swallows of 5mL of water resulted in negative baseline pressure with respect to the fundal pressure. Waves in the body were low pressure and simultaneous. The lower oesophageal sphincter was located at between 44.5cm and 40.3cm, had an increased resting pressure (mean baseline pressure 40.6mmHg) and showed an absence of complete relaxation during the swallow.
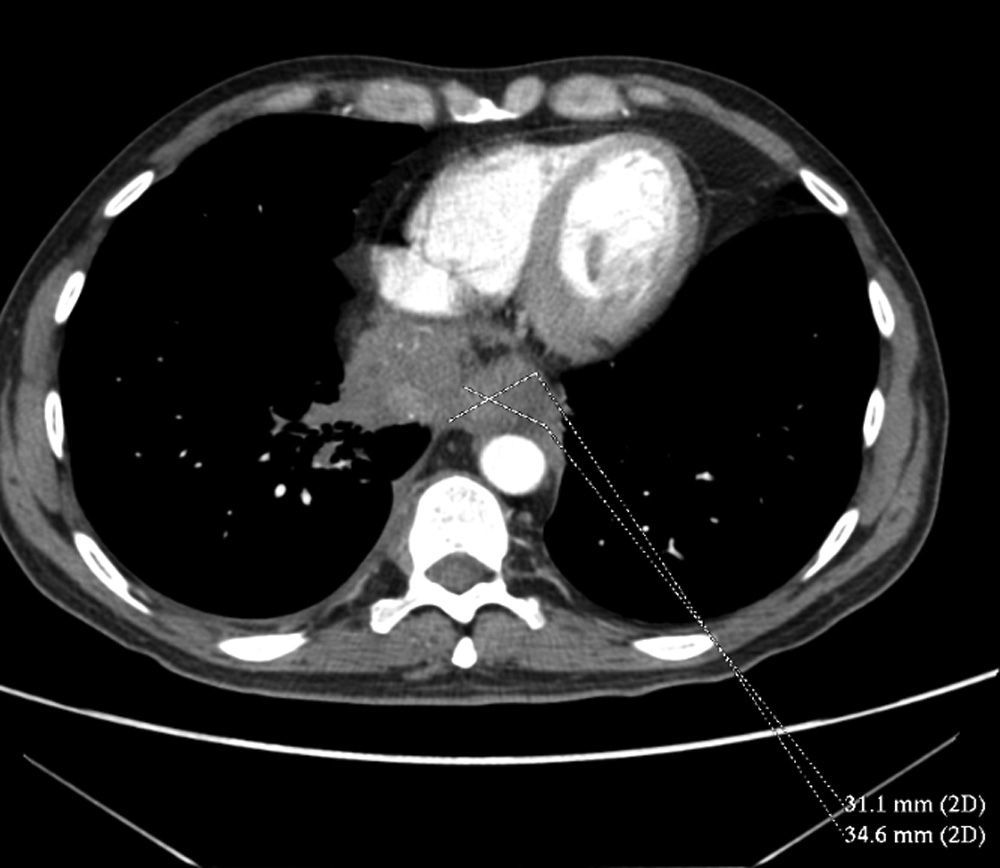
The patient progressed within a few days to aphagia with sialorrhoea. Given the rapid evolution of symptoms, a chest-abdominal computed tomography (CT) scan was performed to rule out pseudoachalasia (Fig. 1) with results pointing to a mass in the posterior–inferior mediastinum, obliterating the distal oesophagus and spreading to invade the mediastinal fat and right lung base and to surround the inferior vena cava. The plane of cleavage was lost with the inferior vena cava (although there was no clear infiltration) and also with the diaphragm. These findings suggested possible oesophageal carcinoma extending to surrounding structures or, less likely, pulmonary neoplasm with mediastinal infiltration. Pathological lymphadenopathies were also identified in the mediastinum, right retrocrural space, retroperitoneum (the largest, in the coeliac trunk, measuring 28mm), iliac chains and inguinal regions.
Repeat gastroscopy showed only concentric, punctiform stenosis at the level of the lower oesophageal sphincter that prevented the endoscope from passing. Biopsies taken at this level ruled out tumour infiltration.
Endoscopic ultrasound with aspiration of one of the mediastinal lymphadenopathies was inconclusive due to extraction of inflammatory fibrinous material corresponding to an area of extensive necrosis.
In view of this result, positron emission tomography-computed tomography (PET-CT) was performed, with the finding of an intrathoracic-extrapulmonary mass at the intercostal level of the right upper hemithorax. Biopsies again showed intense necrosis.
Finally, an exploratory laparoscopy was carried out, with resection of the coeliac axis lymphadenopathy. The findings were consistent with marginal zone B-cell non-Hodgkin lymphoma (positive for CD20).
The patient was started on chemotherapy by the haematology department, with rapid resolution of his dysphagia. He is currently in remission.
Pseudoachalasia is a rare oesophageal motor disorder—generally secondary to neoplasm—that presents with symptoms and radiological and manometric signs that are indistinguishable from achalasia.1 Pseudoachalasia affects approximately 4% of patients who present with signs and symptoms suggestive of achalasia.2
Distinguishing between the 2 conditions is crucial. Achalasia, a primary oesophageal motor disorder of unknown cause, consists of non-relaxation of the lower oesophageal sphincter and aperistalsis of the oesophageal body, whereas pseudoachalasia is mostly caused by a neoplasm resulting from mechanical compression or infiltration of the myenteric plexus by malignant cells or even secondary to a paraneoplastic syndrome.
A total of 264 cases of pseudoachalasia have been described in the medical literature, most secondary to neoplasms (53.9% primary, 14.9% secondary), 11.9% post-surgical (oesophageal or gastric surgery) and, exceptionally, 2.6% secondary to paraneoplastic syndrome.
In older patients who present with rapidly progressive dysphagia and weight loss, whose barium study, upper gastrointestinal endoscopy and manometry results are consistent with achalasia, neoplasm should be ruled out as the primary cause of symptoms.3
Please cite this article as: Cotta Rebollo J, Toscano Castilla E, Lozano Lanagrán M, Martín Ocaña F, Pérez Aísa AC, Fernández Cano F, et al. Seudoacalasia en paciente con antecedentes de linfoma no Hodgkin. Gastroenterol Hepatol. 2016;39:274–275.