Colonoscopy is the diagnostic/therapeutic confirmation test for colorectal cancer. The monitoring of the experience of people who have undergone the test is interesting to improve the quality of the colonoscopy. The aim of the project was to study factors affecting patients’ experience and their relationship with the quality indicators of the Clinical Practice Guidelines.
Patients and methodsAn observational cross-sectional study was conducted, including quality and experience indicators (adapted mGHAA-9 questionnaire and clinical history) in a sample of 432 participants aged between 40- and 75-years-old who had undergone a colonoscopy in 2015. Univariate and multivariate analysis with multiple logistic regression.
ResultsSatisfaction was associated in the multivariate analysis with evaluating the waiting time for the colonoscopy as short (OR=3.80) (1.76–10.90, 95% CI), >55-years-old (OR=2.60) (1.19–5.68, 95% CI), rating the experience with the preparation positively (OR=7.34) (3.15–17.09, 95% CI), not reporting pain or discomfort during the procedure (OR=3.71) (1.03–13.40, 95% CI) (p=0.006) and being examined in a tertiary hospital (OR=2.81) (1.17–6.72; 95% CI) (p=0.020).
DiscussionThe mGHAA-9 questionnaire adapted to Spanish is useful to evaluate patient experience factors. There are aspects to improve in terms of waiting time, colon cleansing, satisfaction with preparation and post-colonoscopy problems. Interventions should be implemented to enhance patient experience and colonoscopy quality.
La colonoscopia es la prueba de confirmación diagnóstica/terapéutica del cáncer colorrectal. La monitorización de la experiencia de las personas que se han realizado la prueba resulta de interés en la mejora de su calidad. El objetivo fue estudiar los factores relacionados con la experiencia y su relación con los indicadores de calidad de las guías de práctica clínica.
Pacientes y métodosSe realizó un estudio transversal observacional, incluyendo indicadores de calidad y experiencia (cuestionario mGHAA9 adaptado e historia clínica) con una muestra de 432 participantes de entre 40-75 años que se realizaron una colonoscopia en 2015. Análisis univariante y multivariante con regresión logística múltiple.
ResultadosLa satisfacción se asoció en el análisis multivariante con una valoración del tiempo de espera para la colonoscopia como corto (OR=3,80) (1,76-10,90; IC 95%), tener más de 55 años de edad (OR=2,60) (1,19-5,68; IC 95%), una valoración positiva de la experiencia de la preparación (OR=7,34) (3,15-17,09; IC 95%), no referir dolor o molestias durante el procedimiento (OR=3,71) (1,03-13,40; IC 95%) (p=0,006) y la realización de la exploración en un hospital terciario (OR=2,81) (1,17-6,72; IC 95%) (p=0,020)
DiscusiónEl cuestionario mGHAA9 adaptado al castellano es útil para estudiar los factores relativos a la experiencia. Hay aspectos de mejora en los tiempos de espera, limpieza colónica, satisfacción con la preparación y los problemas poscolonoscopia. Se deben implementar intervenciones que permitan mejorar la experiencia de las personas y la calidad de la colonoscopia.
Colorectal carcinoma (CRC) is the most common cancer in developed countries.1 Colonoscopy is a confirmatory diagnostic test and is used both to screen for and diagnose inflammatory diseases, premalignant and malignant lesions, and other disorders of the large intestine. Colonoscopy quality is an essential requirement for achieving health outcomes.2–4
The importance of the experience and perceptions of patients undergoing colonoscopy has been recognised, with their assessment being included among the quality indicators for gastrointestinal endoscopy.5 Information on the benefits and risks of the procedure, as well as instructions on bowel preparation, influence quality indicators such as bowel cleanliness and the repetition of colonoscopies.6,7 In turn, pain during the investigation and uncertainty about the results are related to procedure adherence.8 Embarrassment and fear of the test are factors that can influence whether or not people agree to have a colonoscopy.9,10
The implementation of CRC screening in the Basque Country in 2009, using colonoscopy as a confirmatory diagnostic test, led to all indications for colonoscopy being made to adhere to common quality criteria, including bowel cleansing, deep sedation and pre- and post-colonoscopy care.11,12
The aim of this study was to identify the factors which affect peoples’ experience when having a colonoscopy in Osakidetza – Basque Health Service, and how these factors relate to the quality indicators and standards of the European2 and Spanish4 clinical practice guidelines.
Patients and methodsWe conducted an observational cross-sectional study with 15 variables relating to colonoscopy and 26 to the participants’ experience, collected using a questionnaire and their medical records. We estimated that we needed to recruit a sample of 428 patients (accuracy of 3%), estimating losses of 10% (minimum 385 participants). The investigations carried out in November and December 2015 in the 12 endoscopy units in Osakidetza were taken as a reference.
We included people aged 40–75 years, who attended said units to undergo a colonoscopy for any reason, excluding those who had undergone a colonoscopy in the previous six months and hospital inpatients.
A survey was designed based on the modified Group Health Association of America-9 (mGHAA9) patient satisfaction questionnaire of the American Society for Gastrointestinal Endoscopy (ASGE).13 The survey was adapted into Spanish and validated in our population by the research team with 20 cases in October 2015. The research team trained two survey experts who conducted the interviews. The variables recorded were: (1) characteristics of the people (gender, age, weight, height, risk factors, family and personal history); (2) pre-colonoscopy phase (explanations, waiting time, etc.); (3) preparation process (bowel habit, bowel clearing product, tolerance, time of effect, etc.); (4) procedure and post-procedure phase (pain or discomfort, explanations received, overall experience, etc.). The survey was conducted by telephone 24–48h after the test. The healthcare professionals in the endoscopy units did not know which patients were going to be interviewed. Gastrointestinal disturbances (flatulence, diarrhoea, abdominal pain), general pain (headache, nausea, fatigue) and bleeding were considered post-colonoscopy problems. We should mention that these problems are not considered complications derived from the test.
30 days after the colonoscopy, the research team encoded the examination variables and the pathology results according to the clinical practice guidelines.2,4 The aspects recorded were: (a) type of hospital (tertiary/local); (b) indication for the test (screening, surveillance of polyps, diagnostic suspicion, family history of CRC); (c) waiting time for the test; (d) personal and family risk factors; (e) quality of the bowel preparation, assessed by the Boston scale (adequate ≥6 points); (f) fasting time prior to the colonoscopy; (g) results of the examination (normal or no relevant findings, adenomatous polyps, and CRC; (h) complications in the 30 days post-colonoscopy.
With the aim of studying the association with the dependent variables (experience with the preparation, pain or discomfort during the procedure, problems after the examination, quality of bowel cleansing and overall satisfaction) a multivariate analysis with multiple logistic regression was performed, following a predictive model (forward) and using a p value ≤0.20. For the modelling, the dependent variables were dichotomised, as were the categorical and quantitative independent variables where no linear relationship was observed with the log (odds) of the variable under study (likelihood ratio test).
This study was part of the multicentre project “Factores relacionados con la calidad de la colonoscopia en la práctica clínica” (CalCol) [Factors related to the quality of colonoscopy in clinical practice] to assess and improve the quality of colonoscopy following the recommendations of current clinical practice guidelines, approved by the Basque Country Independent Ethics Committee (PI2015085). All the people signed the informed consent form.
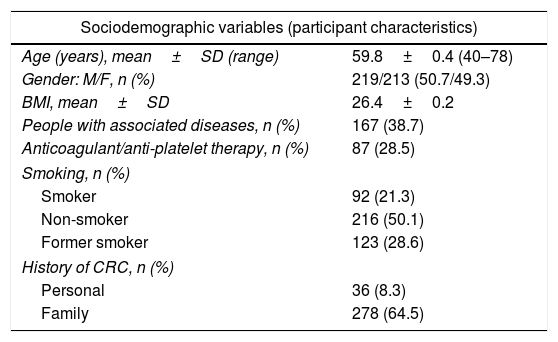
ResultsOf the entire sample (481 people), 432 people (89.81%) finally participated in this study. The mean age of the participants was 59.8±0.4 years (40–78). Certain characteristics of the participants are worth highlighting, such as the mean body mass index (BMI), showing them to be overweight (26.4±0.2), people on anticoagulant/antiaggregant treatment (28.5%) and comorbidities (38.7%). There were 92 smokers (21.3%) and more than half of the participants had a family history of CRC (64.5%). We also found that 46.8% waited less than 30 days for a colonoscopy. Low-volume product was used primarily (92.2%), achieving adequate cleansing in 87.7% of cases. Adenomatous polyps were found in over half of the colonoscopies (50.5%) and there were three cases of CRC. The main reason for the colonoscopy was diagnostic (33.6%) (Table 1).
Description of the characteristics of the study participants and colonoscopies (n=432).
| Sociodemographic variables (participant characteristics) | |
|---|---|
| Age (years), mean±SD (range) | 59.8±0.4 (40–78) |
| Gender: M/F, n (%) | 219/213 (50.7/49.3) |
| BMI, mean±SD | 26.4±0.2 |
| People with associated diseases, n (%) | 167 (38.7) |
| Anticoagulant/anti-platelet therapy, n (%) | 87 (28.5) |
| Smoking, n (%) | |
| Smoker | 92 (21.3) |
| Non-smoker | 216 (50.1) |
| Former smoker | 123 (28.6) |
| History of CRC, n (%) | |
| Personal | 36 (8.3) |
| Family | 278 (64.5) |
| Colonoscopy variables (colonoscopy characteristics) | |
|---|---|
| Waiting time for the colonoscopy, n (%) | |
| Less than 30 days | 225 (46.8) |
| More than 30 days | 203 (42.2) |
| Product used for bowel cleansing, n (%) | |
| Low volume | 390 (92.2) |
| High volume | 33 (7.8) |
| Quality of bowel cleansing, n (%): | |
| Boston scale ≥6 points | 341 (87.7) |
| Boston scale <6 points | 48 (12.3) |
| Caecal intubation, n (%) | 398 (96.6) |
| Findings, n (%) | |
| Normal/No relevant findings | 209 (48.4) |
| Adenomatous polyps | 218 (50.5) |
| CRC | 3 (0.1) |
| Reason for the colonoscopy, n (%) | |
| Screening | 139 (33.2) |
| Polyp surveillance | 105 (24.3) |
| Diagnosis | 145 (33.6) |
| Family history of CRC | 43 (10) |
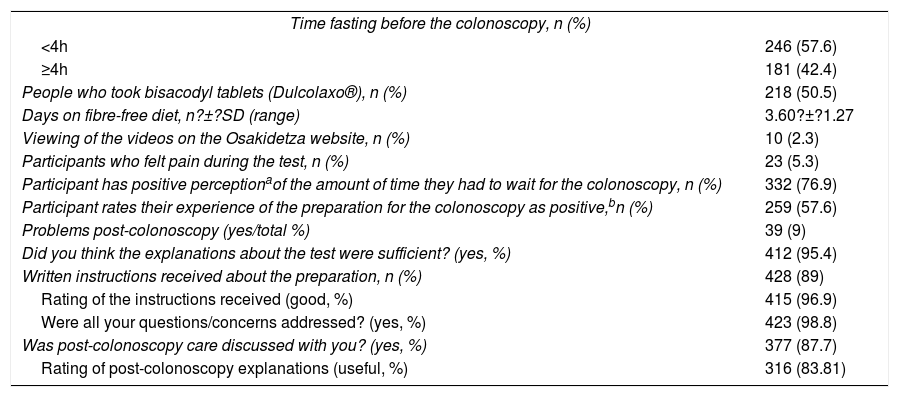
The participants reported that they had stopped eating fibre-containing foods 3.60 (±1.26) days before the colonoscopy; 50.5% took bisacodyl tablets (Dulcolaxo®) and fasted for a mean of 314min (±220min). The time spent fasting was ≤4h in over half of the cases (57.6%).
It proved significant that the waiting time was positively assessed (short/reasonable) in most cases (332 cases, 76.9%) and the experience of preparing for the colonoscopy was perceived as positive by 57.6%. However, 39 participants (9%) reported having had post-colonoscopy problems. Only one serious complication was recorded (lower gastrointestinal bleeding, with hospital admission but no blood transfusion) in the 0–30 days post-procedure; according to clinical practice guideline criteria the event was classed as severe.
The majority of participants reported that they had received information about the procedure (95.4%), instructions about preparation (89%) and about post-colonoscopy care (87.7%). These explanations were rated as useful in 83.81% of the cases (Table 2).
Description of the participants’ responses to the main questions in the survey.
| Time fasting before the colonoscopy, n (%) | |
| <4h | 246 (57.6) |
| ≥4h | 181 (42.4) |
| People who took bisacodyl tablets (Dulcolaxo®), n (%) | 218 (50.5) |
| Days on fibre-free diet, n?±?SD (range) | 3.60?±?1.27 |
| Viewing of the videos on the Osakidetza website, n (%) | 10 (2.3) |
| Participants who felt pain during the test, n (%) | 23 (5.3) |
| Participant has positive perceptionaof the amount of time they had to wait for the colonoscopy, n (%) | 332 (76.9) |
| Participant rates their experience of the preparation for the colonoscopy as positive,bn (%) | 259 (57.6) |
| Problems post-colonoscopy (yes/total %) | 39 (9) |
| Did you think the explanations about the test were sufficient? (yes, %) | 412 (95.4) |
| Written instructions received about the preparation, n (%) | 428 (89) |
| Rating of the instructions received (good, %) | 415 (96.9) |
| Were all your questions/concerns addressed? (yes, %) | 423 (98.8) |
| Was post-colonoscopy care discussed with you? (yes, %) | 377 (87.7) |
| Rating of post-colonoscopy explanations (useful, %) | 316 (83.81) |
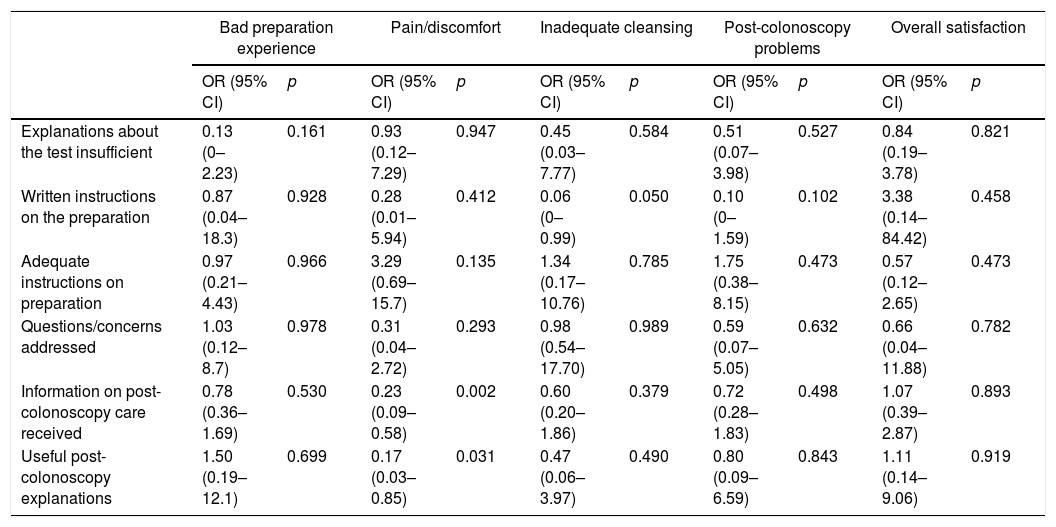
In the univariate analysis, statistically significant associations were found between receiving written instructions about the preparation and a reduction in the risk of inadequate cleansing (OR=0.06) (0–0.99, 95% CI), and between receiving information about post-colonoscopy care (OR=0.23) (0.09–0.58, 95% CI) and a decrease in the likelihood of having discomfort or pain during the procedure (Table 3).
Univariate analysis of the association (OR) between the perception of the information received and its relationship with the main quality indicators linked to satisfaction with the colonoscopy process.
| Bad preparation experience | Pain/discomfort | Inadequate cleansing | Post-colonoscopy problems | Overall satisfaction | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p | |
| Explanations about the test insufficient | 0.13 (0–2.23) | 0.161 | 0.93 (0.12–7.29) | 0.947 | 0.45 (0.03–7.77) | 0.584 | 0.51 (0.07–3.98) | 0.527 | 0.84 (0.19–3.78) | 0.821 |
| Written instructions on the preparation | 0.87 (0.04–18.3) | 0.928 | 0.28 (0.01–5.94) | 0.412 | 0.06 (0–0.99) | 0.050 | 0.10 (0–1.59) | 0.102 | 3.38 (0.14–84.42) | 0.458 |
| Adequate instructions on preparation | 0.97 (0.21–4.43) | 0.966 | 3.29 (0.69–15.7) | 0.135 | 1.34 (0.17–10.76) | 0.785 | 1.75 (0.38–8.15) | 0.473 | 0.57 (0.12–2.65) | 0.473 |
| Questions/concerns addressed | 1.03 (0.12–8.7) | 0.978 | 0.31 (0.04–2.72) | 0.293 | 0.98 (0.54–17.70) | 0.989 | 0.59 (0.07–5.05) | 0.632 | 0.66 (0.04–11.88) | 0.782 |
| Information on post-colonoscopy care received | 0.78 (0.36–1.69) | 0.530 | 0.23 (0.09–0.58) | 0.002 | 0.60 (0.20–1.86) | 0.379 | 0.72 (0.28–1.83) | 0.498 | 1.07 (0.39–2.87) | 0.893 |
| Useful post-colonoscopy explanations | 1.50 (0.19–12.1) | 0.699 | 0.17 (0.03–0.85) | 0.031 | 0.47 (0.06–3.97) | 0.490 | 0.80 (0.09–6.59) | 0.843 | 1.11 (0.14–9.06) | 0.919 |
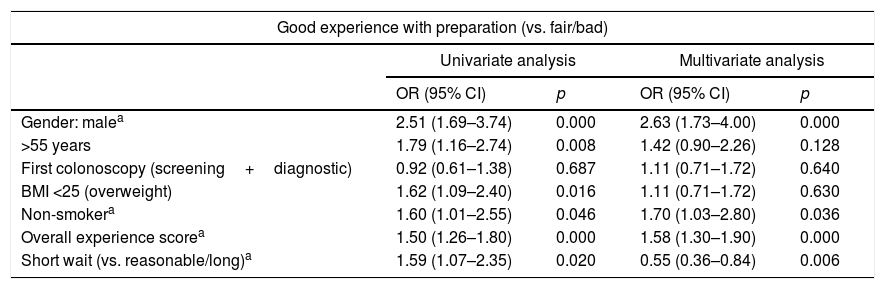
Experience with the preparation turned out to be an important aspect in this study. A positive (good) rating regarding the preparation was associated with being male (OR=2.63) (1.73–4.00, 95% CI) and there was a linear association with the score of the overall experience (OR=1.58) (1.30–1.90, 95% CI) and rating the waiting time as short (OR=0.55) (0.36–0.84, 95% CI).
A significant relationship was found between reporting having felt pain or discomfort (23 participants) during the procedure and having problems in the days after the colonoscopy (OR=4.39) (1.35–14.25, 95% CI) and having had more than six days on a low-fibre diet (OR=4.99) (1.05–23.86, 95% CI). Meanwhile, having received information about post-colonoscopy care (OR=0.32) (0.11–0.97, 95% CI), having the colonoscopy as part of the surveillance of previously diagnosed polyps (OR=0.22) (0.06–0.78, 95% CI) and being treated at a local hospital (OR=0.10) (0.12–0.81, 95% CI) served as factors which reduced the risk of problems after the test (Table 4).
Univariate and multivariate analysis of factors associated with experience with preparation, pain/discomfort during the procedure and post-colonoscopy problems.
| Good experience with preparation (vs. fair/bad) | ||||
|---|---|---|---|---|
| Univariate analysis | Multivariate analysis | |||
| OR (95% CI) | p | OR (95% CI) | p | |
| Gender: malea | 2.51 (1.69–3.74) | 0.000 | 2.63 (1.73–4.00) | 0.000 |
| >55 years | 1.79 (1.16–2.74) | 0.008 | 1.42 (0.90–2.26) | 0.128 |
| First colonoscopy (screening+diagnostic) | 0.92 (0.61–1.38) | 0.687 | 1.11 (0.71–1.72) | 0.640 |
| BMI <25 (overweight) | 1.62 (1.09–2.40) | 0.016 | 1.11 (0.71–1.72) | 0.630 |
| Non-smokera | 1.60 (1.01–2.55) | 0.046 | 1.70 (1.03–2.80) | 0.036 |
| Overall experience scorea | 1.50 (1.26–1.80) | 0.000 | 1.58 (1.30–1.90) | 0.000 |
| Short wait (vs. reasonable/long)a | 1.59 (1.07–2.35) | 0.020 | 0.55 (0.36–0.84) | 0.006 |
| Pain or discomfort during the procedure | ||||
|---|---|---|---|---|
| Univariate analysis | Multivariate analysis | |||
| OR (95% CI) | p | OR (95% CI) | p | |
| Gender: female | 1.13 (0.49–2.61) | 0.777 | 1.07 (0.42–2.75) | 0.882 |
| Age: >55 years | 0.85 (0.34–2.12) | 0.730 | 0.50 (0.18–1.43) | 0.199 |
| Overall satisfaction: 8–10 | 0.25 (0.09–0.68) | 0.006 | 0.30 (0.09–1.00) | 0.052 |
| Good experience with preparation | 0.71 (0.52–0.97) | 0.029 | 2.12 (0.83–5.43) | 0.119 |
| Post-colonoscopy problemsa | 3.06 (1.07–8.77) | 0.037 | 4.39 (1.35–14.25) | 0.014 |
| Explanations about the test: useful | 0.17 (0.03–0.85) | 0.031 | 0.58 (0.32–10.51) | 0.714 |
| Information about post-colonoscopy care receiveda | 0.23 (0.09–0.58) | 0.002 | 0.32 (0.11–0.97) | 0.044 |
| High-vol. product (vs. others) | 5.16 (1.57–17.01) | 0.007 | 1.67 (0.30–9.44) | 0.560 |
| Reason examination: polyp surveillance (vs. others)a | 0.25 (0.09–0.77) | 0.015 | 0.22 (0.06–0.78) | 0.019 |
| Fibre-free diet: >6 daysa | 4.02 (1.07–15.06) | 0.039 | 4.99 (1.05–23.86) | 0.044 |
| Local hospitala | 0.14 (0.02–1.06) | 0.056 | 0.10 (0.12–0.81) | 0.031 |
| Post-colonoscopy problems | ||||
|---|---|---|---|---|
| Univariate analysis | Multivariate analysis | |||
| OR (95% CI) | p | OR (95% CI) | p | |
| Gender: female | 1.72 (0.88–3.39) | 0.113 | 1.78 (0.86–3.67) | 0.119 |
| Age: >55 years | 0.73 (0.36–1.47) | 0.378 | 0.56 (0.26–1.19) | 0.129 |
| Reason examination: screening (vs. others) | 2.16 (1.11–4.20) | 0.023 | 1.53 (0.73–3.16) | 0.253 |
| Waiting time >30 days for colonoscopy | 0.40 (0.19–0.83) | 0.014 | 0.48 (0.22–1.05) | 0.066 |
| Number of polyps removeda | 1.10 (1.00–1.19) | 0.043 | 1.10 (1.02–1.2) | 0.012 |
| Fasting time >5ha | 0.34 (0.14–0.84) | 0.019 | 0.26 (0.10–0.72) | 0.009 |
| Paina | 3.06 (1.07–8.77) | 0.037 | 4.09 (1.30–12.77) | 0.016 |
| Chronic kidney failurea | 16.29 (2.64–100.70) | 0.003 | 13.66 (2.19–85.35) | 0.005 |
The problems people reported having had after the colonoscopy were divided into the following categories: gastrointestinal disturbances (flatulence, diarrhoea, abdominal pain); general pain (headache, nausea, fatigue); and bleeding. Gastrointestinal complaints accounted for 75% of the problems reported. The following factors were identified as related to problems after colonoscopy: the number of polyps removed (OR=1.10) (1.02–1.2, 95% CI); reporting having felt pain or discomfort (OR=4.09) (1.30–12.77, 95% CI); and having chronic kidney disease (OR=13.66) (2.19–85.35, 95% CI). Meanwhile, having fasted for more than 5h was a factor that reduced the likelihood of having these problems (OR=0.26) (0.10–0.72, 95% CI) (Table 4).
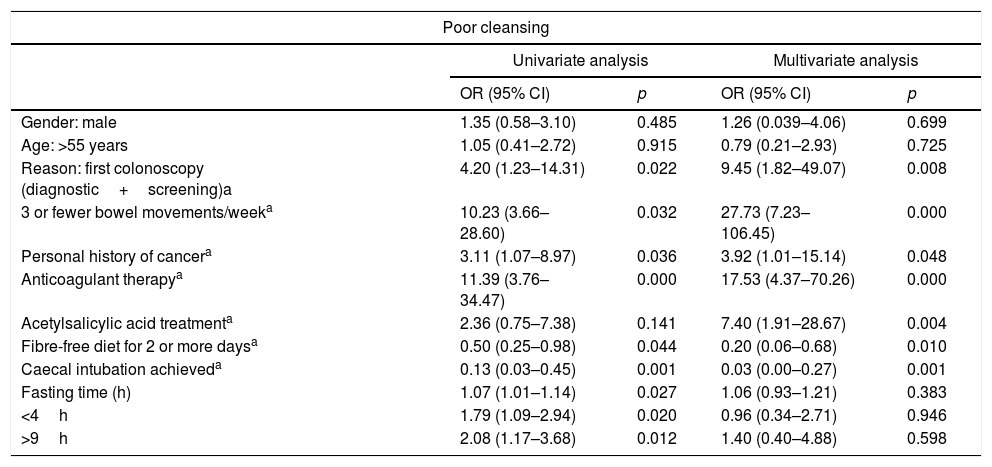
The risk of poor bowel preparation was independently related to being on anticoagulant therapy (OR=17.53) (4.37–70.26, 95% CI) or anti-platelet therapy (OR=7.40) (1.91–28.67, 95% CI), having a personal history of cancer (3.92 (1.01–15.14, 95% CI) and generally having fewer than three bowel movements per week (OR=27.23) (7.23–106.45, 95% CI). However, following a fibre-free (fruit seeds, vegetables, etc.) diet for two or more days was associated with a high likelihood of adequate bowel preparation (OR=0.20) (0.06–0.68, 95% CI).
Lastly, an overall positive rating or satisfaction was associated with having had a positive experience (good+fair) in relation to the bowel preparation (OR=7.34) (3.15–17.09; 95% CI), not reporting pain or discomfort (OR=3.71) (1.03–13.40, 95% CI), rating the wait until the appointment for the test as short (OR=4.38) (1.76–10.90), being over the age of 55 (OR=2.35) (1.1–5.02, 95% CI) and having the colonoscopy in a tertiary hospital (OR=2.81) (1.17–6.72, 95% CI) (Table 5).
Univariate and multivariate analysis of factors associated with poor cleansing and overall satisfaction.
| Poor cleansing | ||||
|---|---|---|---|---|
| Univariate analysis | Multivariate analysis | |||
| OR (95% CI) | p | OR (95% CI) | p | |
| Gender: male | 1.35 (0.58–3.10) | 0.485 | 1.26 (0.039–4.06) | 0.699 |
| Age: >55 years | 1.05 (0.41–2.72) | 0.915 | 0.79 (0.21–2.93) | 0.725 |
| Reason: first colonoscopy (diagnostic+screening)a | 4.20 (1.23–14.31) | 0.022 | 9.45 (1.82–49.07) | 0.008 |
| 3 or fewer bowel movements/weeka | 10.23 (3.66–28.60) | 0.032 | 27.73 (7.23–106.45) | 0.000 |
| Personal history of cancera | 3.11 (1.07–8.97) | 0.036 | 3.92 (1.01–15.14) | 0.048 |
| Anticoagulant therapya | 11.39 (3.76–34.47) | 0.000 | 17.53 (4.37–70.26) | 0.000 |
| Acetylsalicylic acid treatmenta | 2.36 (0.75–7.38) | 0.141 | 7.40 (1.91–28.67) | 0.004 |
| Fibre-free diet for 2 or more daysa | 0.50 (0.25–0.98) | 0.044 | 0.20 (0.06–0.68) | 0.010 |
| Caecal intubation achieveda | 0.13 (0.03–0.45) | 0.001 | 0.03 (0.00–0.27) | 0.001 |
| Fasting time (h) | 1.07 (1.01–1.14) | 0.027 | 1.06 (0.93–1.21) | 0.383 |
| <4h | 1.79 (1.09–2.94) | 0.020 | 0.96 (0.34–2.71) | 0.946 |
| >9h | 2.08 (1.17–3.68) | 0.012 | 1.40 (0.40–4.88) | 0.598 |
| Overall satisfaction | ||||
|---|---|---|---|---|
| Univariate analysis | Multivariate analysis | |||
| OR (95% CI) | p | OR (95% CI) | p | |
| Gender: female | 0.81 (0.42–1.58) | 0.552 | 1.19 (0.56–2.54) | 0.654 |
| Age: >55 yearsa | 2.49 (1.27–4.87) | 0.007 | 2.35 (1.1–5.02) | 0.028 |
| Reason: successive colonoscopies (polyp surveillance+family history) | 1.95 (1.01–3.79) | 0.048 | 1.96 (0.90–4.22) | 0.087 |
| Local hospitala | 1.53 (0.75–3.14) | 0.247 | 2.81 (1.17–6.72) | 0.020 |
| Positive experience with the preparation (good/fair vs. bad)a | 5.32 (2.61–10.86) | 0.000 | 7.34 (3.15–17.09) | 0.000 |
| Short wait (vs. reasonable/long)a | 2.91 (1.31–6.51) | 0.009 | 4.38 (1.76–10.90) | 0.002 |
| No post-colonoscopy problems | 3.11 (1.31–7.35) | 0.010 | 2.13 (0.74–6.16) | 0.162 |
| 2 or more polyps removeda | 2.50 (1.01–6.16) | 0.046 | 3.12 (1.17–8.36) | 0.024 |
| No pain or discomforta | 4 (1.48–10.83) | 0.006 | 3.71 (1.03–13.40) | 0.045 |
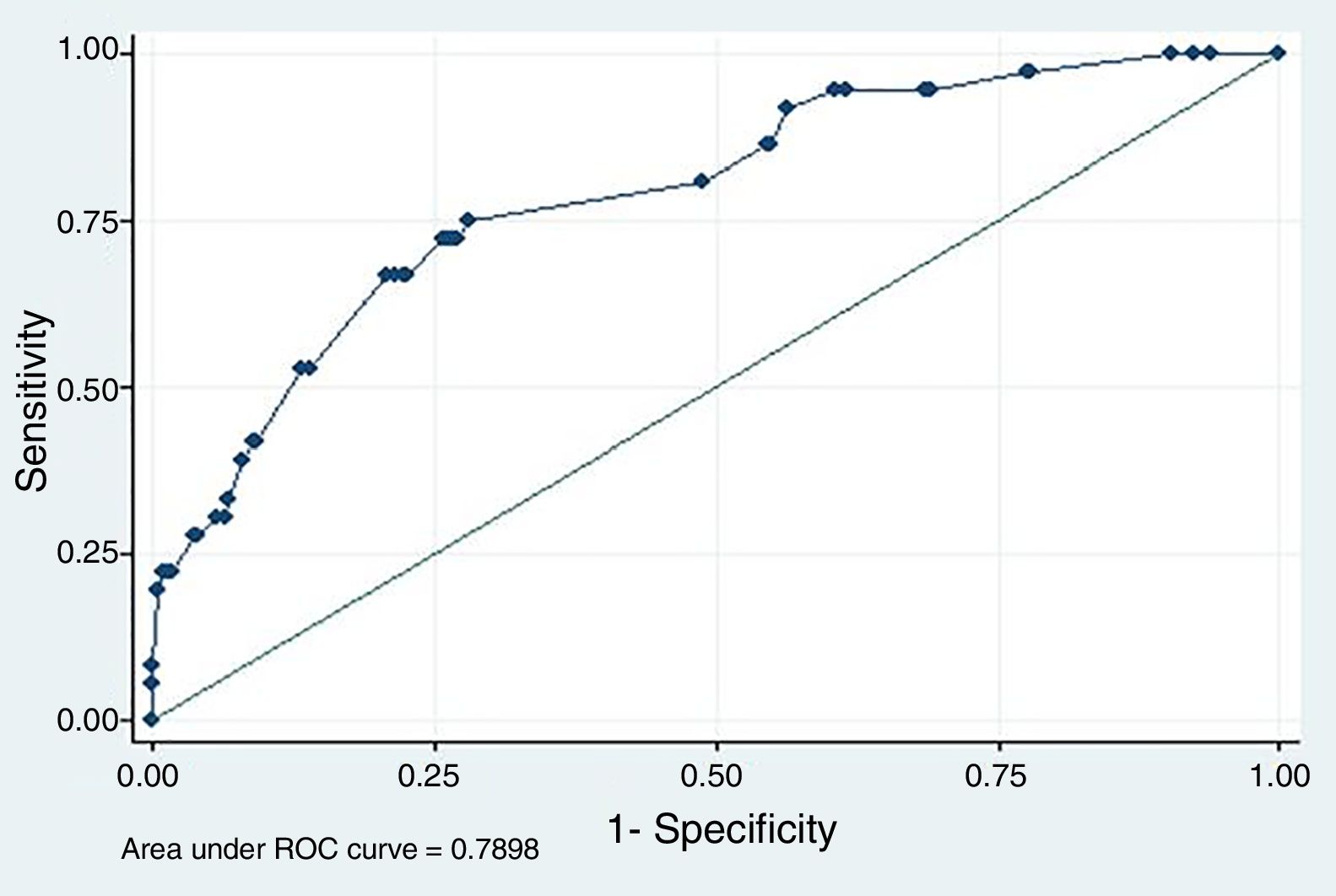
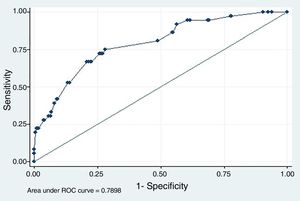
The ROC curve for the multivariate model of the predictors of satisfaction (Fig. 1) had an area under the curve of 0.79 (0.71–0.87; 95% CI). No significant association was found between satisfaction and the variables related to information, such as the quality of the explanations about the test (p=0.246), the preparation (p=0.795) or post-colonoscopy care (p=0.431).
Receiver operating characteristic (ROC) curve of the multivariate model for the prediction of overall colonoscopy satisfaction (Table 5). Variables included: positive experience with bowel preparation; no post-colonoscopy pain or discomfort; rating the waiting time as short; being >55; and undergoing the colonoscopy in a tertiary hospital. Area under the curve=0.79 with 95% CI (0.71–0.87).
Monitoring of the patient's experience is a quality indicator included in the international colonoscopy guidelines, but the use of a single standardised questionnaire to assess this aspect is not yet widespread.5 Some good options include the Global Rating Scale (indirect), used to audit the quality of the endoscopy units and, among the patient-reported tools, those developed by the Gastronet ERCP (Endoscopic Retrograde Cholangiopancreatography) group and the ASGE group. The ASGE group tool was developed by the Group Health Association of America (GHAA, now AHIP [America's Health Insurance Plans]) and has been extensively used and modified, with the most widely distributed version being the ASGE mGHAA9 (2000). Del Río et al.14 first adapted said version into Spanish in 2007.
This study is the first to analyse the factors that affect the patient's experience of colonoscopy since the introduction of CRC screening policies in our region, and to that effect we adapted aspects reported in the literature about use of the mGHAA9 questionnaire over the last 10 years.15,16
The reduction we found in the risk of suffering problems post-colonoscopy after being informed about them, as well as the association between receiving written instructions about preparation and the quality of bowel cleansing, confirm that providing quality information in the different phases of the healthcare process can improve quality indicators for colonoscopies.17 In this context, it was quite striking that very few actually watched the explanatory videos on preparation and the test on the Osakidetza website, and it may be worth exploring ways of promoting the use of this resource during medical and nursing consultations.18 It is worth mentioning that the URL of the website that features these videos was included in the information sheets. In pursuit of the targets set out in the European clinical practice guidelines (>90%) there is some room for improvement in the rate of colonoscopies recorded as having good preparation (87.7%), but the lack of satisfaction we found with the pre-procedural explanations (4.6%) was lower than those of Río et al. (2007) (11.6%) and Denters et al. (2012) (10%).14
However, the absence of operational definitions in the clinical practice guidelines and the differences in the design of the mGHAA9 questionnaire make it difficult to accurately compare the results of other variables, such as the rate of self-reported problems after colonoscopy, with previous studies. This explains the differences in the percentage of cases with post-colonoscopy pain which, with a direct question, some studies have placed at around 59.28%, while in our study, it was 13.66%; or in post-colonoscopy bleeding, which was 30.5% vs. the 0.7% recorded in our series.14
The significance of the association found between satisfaction and self-reported problems after the procedure could indicate the need to ask these questions in more detail over others, such as the perception about the information received in each of the phases of the care process, for which no association with any outcome variable could be found in the multivariate analysis.
Nonetheless, the fact that bowel cleansing was better in second colonoscopies, and among those who adhered better to the preparation instructions, suggests that health education interventions could improve quality indicators such as bowel cleansing19,20, as well as subjective aspects, like overall satisfaction, which have a bearing on adherence to this type of procedure.21 Some of the associations found with bowel cleansing, such as the relationship with bowel habit,22 were expected, while others, such as the relationship between poor cleansing and having had cancer or being on anticoagulant therapy (acetylsalicylic acid) were not found in the literature. In the latter of these cases, the association found may correspond more with the associated comorbidity of people receiving anticoagulant and/or anti-platelet therapy than with the pharmacological effect of this treatment.
With regard to the risk of reporting post-colonoscopy problems, the association with patients who had chronic kidney failure was notable. This may well be due to the effects of the bowel clearing products and the volume of liquids required during the preparation.23 If this association is confirmed, it may be necessary in the future to develop specific protocols for bowel cleansing in these types of patients. In contrast, the linear relationship between the number of polyps removed and post-colonoscopy problems was consistent with reports in the literature.24
When exploring the pain outcome variable, it should be noted that the interpretation thereof was determined by the per protocol use of sedation in screening and in colonoscopies in general.25 For this reason, the association between pain/discomfort during the procedure and the type of hospital and reason for the test warrants further study, taking into account that deep sedation was used less in the colonoscopies for diagnostic purposes and that this procedure was performed mainly in tertiary hospitals.26–29
The variables predictive of overall patient satisfaction with the process were their rating of the waiting time, their experience with the preparation, pain or discomfort during the colonoscopy, age and having the test in a local hospital. The first three of the above variables are widely cited in the literature,25,30 but age and the type of hospital are not. The reasons behind this may be that people under the age of 55 are less likely to have previously undergone a similar investigation and that patients’ expectations are different depending on the complexity of the hospital.
In conclusion, bearing in mind the limitations mentioned above, the Spanish adaptation of the ASGE mGHAA9 questionnaire is a useful tool for studying factors related to the experience of patients undergoing a colonoscopy. The degree of satisfaction of those who underwent a colonoscopy was high, regardless of the reason for the test, and similar to the results observed in other studies. Although the quality indicators we registered already form part of the standards in the clinical practice guidelines, the identification of these factors related to patient experience will enable us to improve quality parameters in colonoscopy.
Conflict of interestThe authors of this study declare that they have no conflicts of interest.
The members of the EUSCOLON research group helped to conduct this study.
Please cite this article as: Fernández-Landa MJ, Aginagalde AH, Arana-Arri E, Bujanda L, Idígoras I, Bilbao I, et al. Indicadores de calidad y satisfacción de los pacientes en la colonoscopia. Gastroenterol Hepatol. 2019;42:73–81.