Multidrug-resistant organisms (MDROs) are a reality that can alter the paradigm of treatment and prevention of infection in patients with liver cirrhosis (LC).
ObjectiveIdentify risk factors for the occurrence of MDROs in patients with LC.
Patients and methodsProspective study from October 2017 to March 2018 in consecutively hospitalized patients with decompensated LC with infection. Blood, urine and ascitic fluid cultures were analyzed. A p-value ≤0.05 was considered statistically significant.
ResultsMDROs isolated in 18 of 52 episodes of infection. MDROs were associated with the use of proton pump inhibitors (PPIs) (p=0.0312), antibiotic therapy in the last 90 days (p=0.0033) and discharge within preceding 30 days or current hospitalization above 48h (p=0.0082). There was higher 90-day mortality in patients with MDROs infection (71.4% versus 35.7%, p=0.0316).
ConclusionMDROs infections were prevalent in this cohort and associated with 90-day mortality. Use of PPIs and antibiotics increased the risk of MDROs infections, suggesting that its prescription should be restricted to formal indication. Hospitalization was associated with the onset of MDROs, so LC patients should stay at the hospital the least possible. It is relevant to investigate other factors predisposing to the emergence of these microorganisms, in order to prevent it.
Los organismos multirresistentes (MDROs, por sus siglas en inglés) son una realidad que puede alterar el paradigma del tratamiento y la prevención de la infección en los pacientes con cirrosis hepática (LC, por sus siglas en inglés).
ObjetivoIdentificar los factores de riesgo para la aparición de MDROs en pacientes con LC.
Pacientes y métodosEstudio prospectivo de octubre de 2017 a marzo de 2018 en pacientes hospitalizados consecutivamente con LC descompensada con infección. Se analizaron los cultivos de sangre, orina y líquido ascítico. Se consideró estadísticamente significativo un valor de p≤0,05.
ResultadosSe aislaron MDROs en 18 de los 52 episodios de infección. Los MDROs se asociaron con el uso de inhibidores de la bomba de protones (IBP) (p=0,0312), la terapia antibiótica en los últimos 90 días (p=0,0033) y el alta en los 30 días anteriores o la hospitalización actual superior a 48h (p=0,0082). Hubo una mayor mortalidad a los 90 días en los pacientes con infección por MDROs (71,4 frente al 35,7%; p=0,0316).
ConclusiónLas infecciones por MDROs fueron prevalentes en esta cohorte, y se asociaron con la mortalidad a los 90 días. El uso de IBP y antibióticos aumentó el riesgo de infecciones por MDROs, lo que sugiere que su prescripción debe restringirse a la indicación formal. La hospitalización se asoció a la aparición de MDROs, por lo que los pacientes con LC deberían permanecer en el hospital el menor tiempo posible. Es relevante investigar otros factores que predisponen a la aparición de estos microorganismos para prevenirla.
Liver cirrhosis (LC) is one of the most common causes of death worldwide, and infection, the leading cause of acute liver decompensation, is associated with high morbidity and mortality.1,2 Infection is present at admission or develops during hospitalization in 25–35% of patients, an incidence which is 4 to 5 folds higher than that observed in the general population.2,3 Overall mortality of infected cirrhotic patients is around 30% at 1 month and more than 50% at 12 months.1,4 The high mortality rate of infections in cirrhotic patients is related not only to its direct effects but also to their pivotal role in triggering acute-on-chronic liver failure (ACLF).1,5,6
During the natural history of LC, there is a favorable environment for the development of bacterial infections, not only as a consequence of dysbiosis, but also due to immune dysfunction.7,8
Although Gram-negative bacteria from intestinal origin are very often isolated, Gram-positive bacteria are an increasingly frequent cause of infection, particularly in hospitalized patients. In the last years, multidrug-resistant organisms (MDROs) are becoming an important clinical problem worldwide.1,2,6,7 MDROs are organisms resistant to 3 or more of the main antibiotic families. The main MDROs bacteria are extended-spectrum β-lactamase-producing Enterobacteriaceae (ESBL); non-fermentable Gram-negative bacilli such as Pseudomonas aeruginosa, Stenotrophomonas maltophilia or Acinetobacter baumannii, methicillin-resistant Staphylococcus aureus (MRSA) and vancomycin-susceptible or resistant Enterococci (VSE, VRE).1–3 MDROs infections have increased in frequency, not only related to healthcare exposure, but also in the community.1
There are many factors associated with an increased risk of infection, such as poor liver function, variceal bleeding, low ascitic fluid protein levels, prior spontaneous bacterial peritonitis (SBP), hospitalization and antibiotic administration (including long-term norfloxacin prophylaxis).2,8
SBP and urinary tract infections are the most frequent infections, followed by pneumonia, skin and soft tissue infections, and bacteremia.2,8
The main objective of this study is to identify risk factors for the occurrence of MDROs in patients with LC.
Patients and methodsThis is a prospective and observational cohort study, where all patients with LC and infection hospitalized in a Hepatology Unit between October 2017 and March 2018 were included. Clinical and demographic characteristics were evaluated, namely gender, age, Child-Turcotte-Pugh (CTP) scores, cirrhosis etiology, type of infection, antibiotic use and mortality rate. Blood, urine and ascitic fluid cultures were analyzed.
We have excluded patients under 18 years of age, evidence of current malignancy (except hepatocellular carcinoma within transplant criteria or non-melanocytic skin cancer), severe critical myopathy and those under immunosuppressive therapy within the last three months or acquired or innate immunodeficiency.
The study was approved by the ethical review board (number 41/2020, Hospital Professor Doutor Fernando Fonseca, 06/05/2020). Patients were not required to give informed consent because this analysis used anonymous registry data. The study protocol conforms to the ethical guidelines of the 1975 Declaration of Helsinki as reflected in a priori approval by the institution's human research committee.
DefinitionsLC is the irreversible fibrosis of the liver. Diagnosis of cirrhosis was made based on clinical, analytical and radiological parameters or liver histology.
MDROs were defined as organisms nonsusceptibility to at least 1 agent in at least 3 antimicrobial categories.
Community acquired infection was diagnosed when infection was identified at admission or within the first 48h after hospitalization. Nosocomial infection was diagnosed when infection was acquired after 48h of hospitalization; or within 30 days of discharge when the patient was admitted in a hospital prior to the current admission.
Microbiological investigationsAll patients were subjected to infection-screen with clinical evaluation, followed by chest radiogram, urinalysis, urine culture-sensitivity, ascitic fluid for total and differential counts, culture-sensitivity, paired blood cultures, pus for Gram stain/culture-sensitivity, sputum/bronchoalveolar lavage/endotracheal aspirates and stools when required. All bacterial isolates were identified by standard microbiological techniques including colony morphology, Gram staining followed by colorimetry and turbidimetry. Antimicrobial susceptibility testing was done for third and fourth generation cephalosporins, piperacillin-tazobactam, carbapenems, tetracycline, tigecycline, fosfomycin, chloramphenicol and colistin and interpreted as per EUCAST guidelines.
Statistical analysisStatistical analysis was performed using SPSS software. The quantitative variables were presented as mean with standard deviation and qualitative variables as proportions with percentages. Comparison between groups was done using Student's t-test and Mann–Whitney test. A p-value ≤0.05 was considered significant.
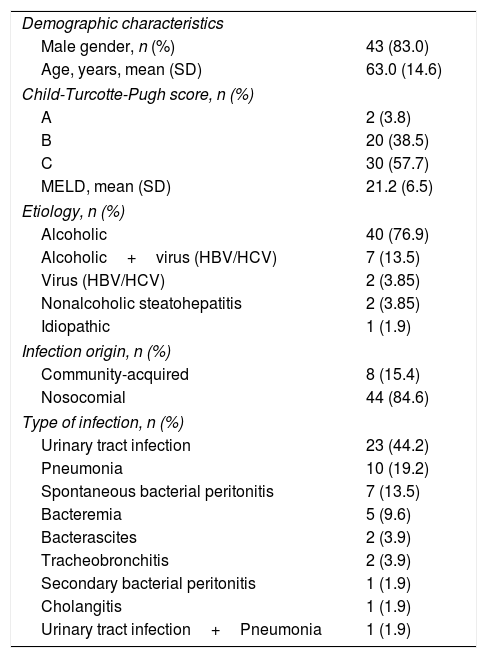
ResultsClinical and demographic dataWe included a total of 52 episodes of infection, corresponding to 22 different patients, of whom 83% were males, with a mean age of 63.0±14.6 years. The majority of patients belonged to CTP class C (n=30, 57.7%), followed by class B (n=20, 38.5%) and A (n=2, 3.8%). The median Model for End Stage Liver Disease (MELD) was 21.2±6.5 (7–36). The most common etiology of LC was alcoholic (n=40, 76.9%), followed by alcoholic and viral, such as hepatitis B virus (HBV) and/or hepatitis C virus (HCV) (n=7, 13.5%), viral (HBV/HCV) (n=2, 3.85%), nonalcoholic steatohepatitis (n=2, 3.85%) and idiopathic (n=1, 1.9%), which are represented in Table 1.
Characteristics of patients with liver cirrhosis and infections.
| Demographic characteristics | |
| Male gender, n (%) | 43 (83.0) |
| Age, years, mean (SD) | 63.0 (14.6) |
| Child-Turcotte-Pugh score, n (%) | |
| A | 2 (3.8) |
| B | 20 (38.5) |
| C | 30 (57.7) |
| MELD, mean (SD) | 21.2 (6.5) |
| Etiology, n (%) | |
| Alcoholic | 40 (76.9) |
| Alcoholic+virus (HBV/HCV) | 7 (13.5) |
| Virus (HBV/HCV) | 2 (3.85) |
| Nonalcoholic steatohepatitis | 2 (3.85) |
| Idiopathic | 1 (1.9) |
| Infection origin, n (%) | |
| Community-acquired | 8 (15.4) |
| Nosocomial | 44 (84.6) |
| Type of infection, n (%) | |
| Urinary tract infection | 23 (44.2) |
| Pneumonia | 10 (19.2) |
| Spontaneous bacterial peritonitis | 7 (13.5) |
| Bacteremia | 5 (9.6) |
| Bacterascites | 2 (3.9) |
| Tracheobronchitis | 2 (3.9) |
| Secondary bacterial peritonitis | 1 (1.9) |
| Cholangitis | 1 (1.9) |
| Urinary tract infection+Pneumonia | 1 (1.9) |
SD: Standard deviation, MELD: Model for End-Stage Liver Disease Score, HBV: Hepatitis B virus, HCV: Hepatitis C virus,.
Most infections were nosocomial (n=44, 84.6%) followed by community-acquired (n=8, 15.4%). Urinary tract infection (UTI) was the most prevalent (n=23, 44.2%), followed by pneumonia (n=10, 19.2%), SBP (n=7, 13.5%), bacteremia (n=5, 9.6%), bacterascites (n=2, 3.9%), tracheobronchitis (n=2, 3.9%); secondary bacterial peritonitis (n=1, 1.9%) and cholangitis (n=1, 1.9%). UTI and pneumonia were seen in 1 (1.9%) patient, simultaneously (Table 1).
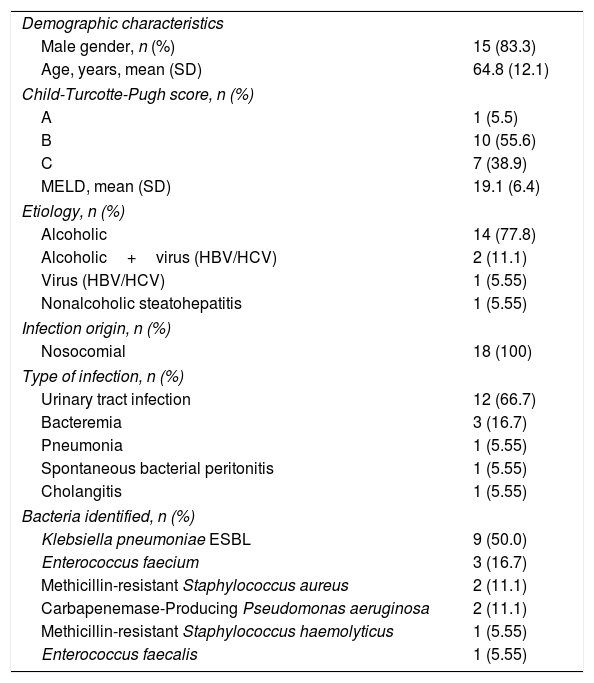
Characterization of MDROs infectionsIn 37 of the 52 episodes (71.1%) of infection microorganisms in cultural examinations were identified. In 2 patients there were 2 microorganisms isolated. MDROs were isolated in 18 episodes (48.6%) of which: 15 (83.3%) were males, with a mean age of 64.8±12.1 years; 1 patient (5.5%) was CTP A, 10 (55.6%) CTP B, and the remaining CTP C (n=7, 38.9%). The median MELD score was 19.1±6.4 (8–31). All patients have had previous decompensations. In 4 patients, 2 different MDRO infections (2 of them on the same admission) were identified. The remaining had just 1 MDRO infection during this period. Klebsiellapneumoniae ESBL was the most frequently isolated MDRO (n=9, 50.0%), followed by methicillin-resistant Enterococcus faecium (n=2, 11.1%), methicillin-resistant Staphylococcus aureus (n=2, 11.1%), carbapenemase-producing Pseudomonas aeruginosa (n=2, 11.1%), vancomycin-resistant Enterococcus faecium (n=1, 5.55%), methicillin-resistant Staphylococcus haemolyticus (n=1, 5.55%) and methicillin-resistant Enterococcus faecalis (n=1, 5.55%). The most prevalent etiology of LC was alcoholic (n=14, 77.8%), followed by alcoholic and viral (HBV/HCV) (n=2, 11.1%), viral (HBV/HCV) (n=1, 5.55%) and nonalcoholic steatohepatitis (n=1, 5.55%). All infections were nosocomial. The most common sites of isolation of MDROs were urine (n=12, 66.7%), blood (n=4, 22.2%), ascitic fluid (n=1, 5.55%) and sputum (n=1, 5.55%). (Table 2)
Characteristics of patients with liver cirrhosis and multidrug-resistant organisms’ infections.
| Demographic characteristics | |
| Male gender, n (%) | 15 (83.3) |
| Age, years, mean (SD) | 64.8 (12.1) |
| Child-Turcotte-Pugh score, n (%) | |
| A | 1 (5.5) |
| B | 10 (55.6) |
| C | 7 (38.9) |
| MELD, mean (SD) | 19.1 (6.4) |
| Etiology, n (%) | |
| Alcoholic | 14 (77.8) |
| Alcoholic+virus (HBV/HCV) | 2 (11.1) |
| Virus (HBV/HCV) | 1 (5.55) |
| Nonalcoholic steatohepatitis | 1 (5.55) |
| Infection origin, n (%) | |
| Nosocomial | 18 (100) |
| Type of infection, n (%) | |
| Urinary tract infection | 12 (66.7) |
| Bacteremia | 3 (16.7) |
| Pneumonia | 1 (5.55) |
| Spontaneous bacterial peritonitis | 1 (5.55) |
| Cholangitis | 1 (5.55) |
| Bacteria identified, n (%) | |
| Klebsiella pneumoniae ESBL | 9 (50.0) |
| Enterococcus faecium | 3 (16.7) |
| Methicillin-resistant Staphylococcus aureus | 2 (11.1) |
| Carbapenemase-Producing Pseudomonas aeruginosa | 2 (11.1) |
| Methicillin-resistant Staphylococcus haemolyticus | 1 (5.55) |
| Enterococcus faecalis | 1 (5.55) |
SD: Standard deviation, MELD: Model for End-Stage Liver Disease Score, HBV: Hepatitis B virus, HCV: Hepatitis C virus, ESBL: extended-spectrum β-lactamase.
Comparing the group of patients with MDROs and the one without MDROs, the group with MDROs was associated with: the use of proton pump inhibitors (PPI) (72.2% versus 36.8%, p=0.0312), antibiotic therapy in the last 90 days, including norfloxacin prophylaxis (94.4% versus 47.4%, p=0.0033) and hospitalization for more than 48h or discharge for less than 30 days (100% versus 68.4%, p=0.0082). The presence of diabetes mellitus (38.9% versus 31.6%), hepatocellular carcinoma (33.3% versus 31.6%) and invasive procedures, such as bladder catheter (61.1% versus 42.1%) and central venous catheter (38.9% versus 26.3%) were not relevant as factors predisposing to MDROs infection (p=0.6526, p=0.9124, p=0.2599 and p=0.4283, respectively).
In the MDRO group there were more patients with ACLF (n=5, 27.8%) than in the group without MDRO (n=4, 21.1%), p=0.6340. In both groups 1 patient had ACLF grade 2 and the remaining patients had ACLF grade 1.
There was higher 90-day mortality in patients with MDROs infection (71.4% versus 35.7%, p=0.0316), although 28-day mortality was not statistically different between the 2 groups (27.8% versus 26.3%, p=0.9230).
DiscussionInfections are increasingly recognized among hospitalized patients with LC. European Association for the Study of the Liver (EASL) describes them as a major precipitant of decompensation, among 21% patients with acute decompensation and in 30% patients with ACLF.7,9 The increase in the rate of MDROs infections, almost 10% in less than 8 years, underlines the growing clinical relevance of antibiotic resistance in decompensated cirrhosis and ACLF.6 Our study is in agreement with this global healthcare problem. The overall prevalence of MDROs infections in our study was 34.6%. This finding is identical to the whole CANONIC cohort of culture-positive infections (29.2%).6,7,10 In line with the numbers reported in literature, most infections in our cohort were nosocomial.6,7,11
In the global study, Piano et al.10 demonstrated that SBP/Secondary bacterial peritonitis followed by UTI and pneumonia were the most predominant infections in LC.7,10 However, in our study, UTI followed by pneumonia and SBP were the commonest infections in LC. In the specific setting of MDROs, SBP, UTI and pneumonia were identified as the most frequent sites of infection in European series.6,7 However, we found UTI and bacteremia the most predominant sites of infections by MDROs.
In the CANONIC cohort, ESBL-producing Enterobacteriaceae was the MDRO more frequently isolated, followed by VSE and MRSA.6 This is similar to what was found in our study: Klebsiellapneumoniae ESBL was the most frequently isolated MDRO (50.0%), followed by Enterococcus faecium (16.7%), methicillin-resistant Staphylococcus aureus (11.1%), carbapenemase-producing Pseudomonas aeruginosa (11.1%), methicillin-resistant Staphylococcus haemolyticus (5.55%) and Enterococcus faecalis (5.55%).
Multiple risk factors for MDROs infections have been identified in LC, including: recent use of antibiotics, healthcare exposure, nosocomial origin, invasive procedures and sarcopenia.6,7,12 The CANONIC cohort only identified three risk factors for MDROs: a nosocomial origin of infection, the need of Intensive Care Unit (ICU) admission and recent hospitalization within the previous 3 months. Instrumentation and exposure to broad-spectrum antibiotics could account for this finding.7 Our study found an association between these type of microorganisms and a nosocomial origin of infection, previous exposure to antibiotics and recent hospitalization too. We have not looked for the relation with sarcopenia and ICU admission, but we think these might be interesting risk factors to evaluate in a future study. Our study did not find any relevant statistical association between MDROs and invasive procedures, as was previously described in the literature.
PPI use is a known risk factor for bacterial infections in LC, such as SBP. PPI use, which diminishes the body's natural defense from microorganisms and causes dysbiosis, in combination with increased bacterial translocation in decompensated cirrhosis, could increase hepatic decompensation, infection risk and mortality in patients with LC.13–15 Janka et al.14 and Dam et al.15 considered the effect of PPI administration on the appearance of different types of infections, other than SBP. Our study also found a relevant statistical association between PPI and different types of infections, particularly different types of MDROs infection. Our study is the first to consider the effect of PPI use on the development of MDROs infections. These results warrant a cautious approach to prescribe PPIs to patients with LC.
Fernandez et al.6 and Piano et al.10 reported higher septic shock and 28-day mortality in MDROs infections in cirrhosis (35.1%). Piano et al.10 also showed more ICU admission and organ failure in this type of infections. We demonstrated similar 28-day mortality to the global study10 in MDROs infections (27.8% versus 29%). However, in our study there was no relevant statistical association between MDROs infection and 28-day mortality (27.8% versus 26.3%, p=0.9230). Nevertheless, our study also evaluated 90-day mortality, not analyzed in the previous studies, which was significantly higher (71.4% versus 35.7%, p=0.0316).
In conclusion, we want to highlight that efforts should be made to limit the emergence of MDROs in patients with LC and this involves MDROs epidemiologic investigation at each hospital, as we have done in our study. We also consider important to research other risk factors predisposing to these organisms.
In the near future, we hope there will be models or biomarkers to identify high-risk patients in order to prevent this kind of infections.2,4
Our study has several strengths and novelties: it is the first single-center study prospectively designed, is the first one which analyzes PPIs in this setting and identifies them as a risk factor for MDROs infections in LC, and also the only one that addresses the association between MDROs infection and 90-day mortality, finding that these patients have higher 90-day mortality (in opposition to the previous studies which did not find an association between MDROs infection and higher 90-day mortality).
Limitations include the relatively small number of patients and the lack of adequate data on antimicrobial usage; the single-center design of the study may be regarded as a limitation but also as a strength in the way that it represents a standardized approach to this patient population.
In conclusion, this study pretends to give information about MDROs infections in LC, focusing on its risk factors, which is of added value to the current literature.
NotePatients were not required to give informed consent because this is an anonymous registry analysis.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
AuthorshipAll authors have made substantial contributions to all of the following: (1) the conception and design of the study, or acquisition of data, or analysis and interpretation of data, (2) drafting the article or revising it critically for important intellectual content, (3) final approval of the version to be submitted.
Conflicts of interestNone declared.