We present the case of an asymptomatic 69-year-old man with a prior history of removed retroauricular epidermoid cyst. Histology revealed foci of intraluminal shadow cells, a finding consistent with Gardner's syndrome. He did not exhibit any other associated extraintestinal manifestations and had no family history of gastrointestinal disease. The panendoscopy revealed multiple millimetric oesophageal polyps, the histology of which did not indicate adenomatous changes. The colonoscopy showed six polyps of between 2 and 20mm, which were resected. The histological study was consistent with tubular adenoma, with low-grade dysplasia observed in three of them and high-grade dysplasia in the other three. In addition, a 15-mm ulcerated neoformation was identified in the rectosigmoid junction, the biopsies of which were consistent with adenocarcinoma. Five days after the colonoscopy, the patient had low-grade fever and pain in the right iliac fossa. A CT scan was ordered that revealed findings suggestive of acute appendicitis, which was initially managed conservatively. Neoadjuvant radiotherapy was started and the follow-up CT scan revealed a focal hepatic injury. Surgery was performed, consisting of lower anterior rectal resection, liver metastasectomy and appendectomy, finding adenocarcinoma with lymph node involvement, adenocarcinoma liver metastasis and appendiceal goblet cell carcinoid tumour with free edges in the histological study, respectively. The genetic study for the APC mutation was negative. Adjuvant chemotherapy with fluorouracil and oxaliplatin was then administered, with no evidence of tumour recurrence to date.
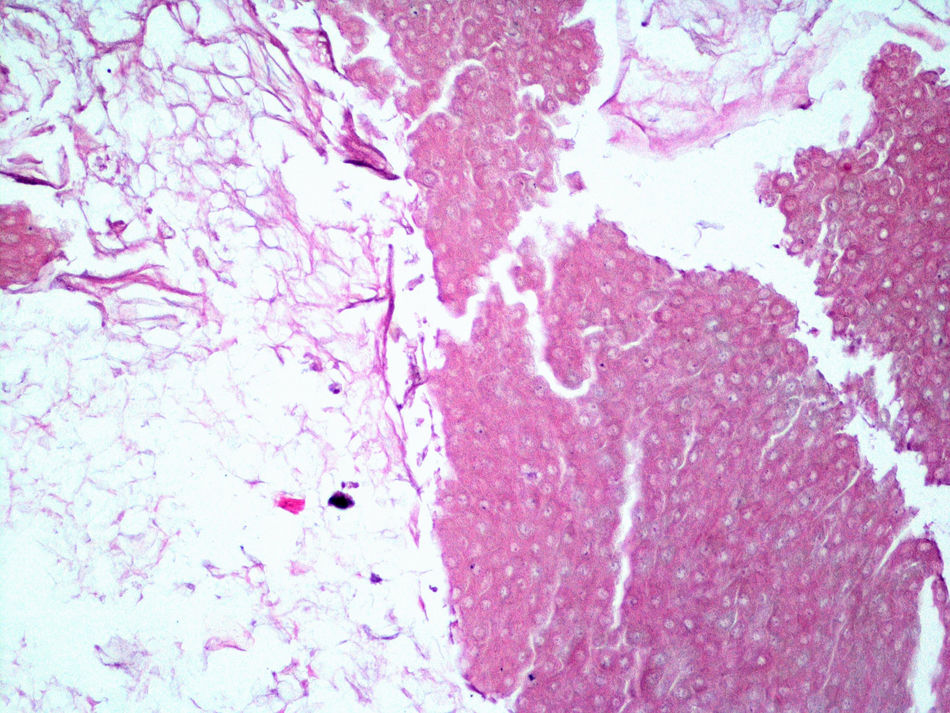
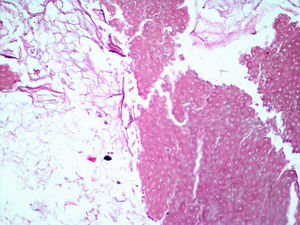
Shadow or ghost cells are keratinised eosinophilic cells with an unstained central area at the site of the shadow of the lost nucleus. Their presence is an indication of an aborted attempt to form hair shafts (Fig. 1). They are a characteristic, albeit nonspecific, histological finding of pilomatricoma and pilomatrical carcinoma.1 Familial adenomatous polyposis is an autosomal dominant disorder secondary to the mutation of the APC tumour suppressor gene and is characterised by the development of multiple premalignant adenomatous colon polyps. There are numerous variants of this disease, one of which is Gardner's syndrome, which is defined as the association of colonic polyposis with the onset of various extraintestinal manifestations.2 Of these, the most common are epidermoid cysts and skin fibromas, osteoma of the face and long bones, hypertrophy of the retinal pigment epithelium, dental abnormalities and desmoid tumours of the abdominal and intra-abdominal wall, as well as the development of malignant tumours at various sites (thyroid, duodenal, ampullary, pancreatic, gastric, etc.).3 Some of these extraintestinal manifestations may occur years before the onset of gastrointestinal symptoms.
Epidermoid cysts occur in 50–60% of all cases of Gardner's syndrome compared to 9–10% in the general population.2 They generally develop before puberty, may be the first sign of the disease and carry no risk of malignancy. Accumulations of shadow cells and foci of matrix keratinisation inside these cells have been reported, similar to what occurs in pilomatricoma.4 Although they constitute a common finding in the physical examination of patients with Gardner's syndrome, they are not specific to the disease and have been associated with other conditions like MUTYH-associated adenomatous polyposis (germline mutations) and with somatic mutations in the catenin beta 1 gene (CTNNB1).5 Familial adenomatous polyposis associated with MUTYH mutations is an autosomal recessive disorder characterised by the appearance in adult age of multiple adenomatous polyps with an increased risk of developing colorectal cancer. In the event of histological findings consistent with pilomatricoma in a patient with multiple adenomatous polyps, the differential diagnosis should include more conditions than just Gardner's syndrome, and potentially test for genetic mutations responsible for attenuated polyposis syndromes, like the MUTYH gene, and not exclusively associated with the APC gene.
In conclusion, the identification of shadow cells in cutaneous epidermoid cysts may be the first finding to generate suspicion of polyposis syndromes like Gardner's syndrome. In our patient, the detection of shadow cells inside a removed cutaneous cyst guided us to this potential diagnosis. Although it ultimately did not meet the characteristic endoscopic or genetic criteria for this syndrome, these findings led to a colonoscopy being requested, which identified colorectal cancer. The onset of post-colonoscopy appendicitis led to the diagnosis of an appendiceal goblet cell tumour.
Please cite this article as: García de la Filia Molina I, Crespo Pérez L, Ríos León R, Barbado Cano A, Moreno García del Real C, Aburto Bernardo A, et al. Quiste epidermoide cutáneo con células sombra: a la búsqueda de un síndrome polipósico. Gastroenterol Hepatol. 2019;42:386–387.