Stricture is one of the main complications of Crohn's disease (CD). Among the main conservative therapeutic alternatives, endoscopic balloon dilation (EBD) of the strictures stands out, which can improve the symptoms and delay or even avoid the need for more surgeries. The main aim of this study was to evaluate the efficacy of the EBD in CD patients with post-surgical anastomotic strictures from a previous surgery.
Patients and methodsAn observational study of a cohort of 32 patients with CD who underwent EBD due to uncomplicated strictures at a tertiary hospital, since 2009. Demographic, clinical and disease variables, medical treatments and previous surgeries and types, analytical variables at the time of dilation, number of dilations, complications and need for subsequent surgery were collected by searching data in clinical records.
ResultsThirty-two patients were included, performing a total of 63 endoscopic dilations. A technical success of 63.5%, a therapeutic success by dilation of 58.75% and a therapeutic success per patient of 62.5% were achieved. Regarding complications, the percentage of post-dilation adverse events was 3.2% and post-dilation incidents were 4.8%. Thirty EBD did not need any medical treatment modification, 9 EBD remained untreated and 12 EBD required further surgery. The length of the strictures, but not the ongoing treatment, was the only statistically significant factor of therapeutic success by dilation and per patient.
ConclusionsEBD seems a safe technique in short post-surgical strictures, can avoid the need for new surgery and prevents unnecessary immunosuppression in patients with CD anastomotic strictures.
La estenosis es una de las principales complicaciones de la enfermedad de Crohn (EC). La dilatación endoscópica con balón (DEB) es una de las principales alternativas terapéuticas para mejorar los síntomas y retrasar o evitar nuevas cirugías. El objetivo principal fue evaluar la eficacia de la DEB en pacientes con EC y estenosis anastomótica posquirúrgica.
Pacientes y métodosEstudio observacional de una cohorte de 32 pacientes con EC tratados con DEB por estenosis no complicadas en un hospital terciario, desde 2009. Se recogieron variables demográficas, clínicas y de la enfermedad, tratamientos médicos y cirugías previas, variables analíticas en el momento de la dilatación, número de dilataciones, complicaciones y necesidad de cirugía posterior mediante la búsqueda de datos en las historias clínicas.
ResultadosSe incluyó a 32 pacientes, con un total de 63 dilataciones endoscópicas. Se obtuvo un éxito técnico del 63,5%, un éxito terapéutico por dilatación del 58,75% y un éxito terapéutico por paciente del 62,5%. En cuanto a las complicaciones, el porcentaje de eventos adversos fue del 3,17% y de incidentes del 4,8%. No necesitaron ninguna modificación del tratamiento médico 30 DEB, 9 permanecieron sin tratamiento y 12 requirieron una nueva cirugía. La longitud de la estenosis, pero no el tratamiento en curso, fue el único factor estadísticamente significativo del éxito terapéutico por dilatación y por paciente.
ConclusionesLa DEB parece una técnica segura en las estenosis posquirúrgicas cortas, ya que podría evitar nuevas cirugías y evitar la inmunosupresión innecesaria en pacientes con estenosis anastomóticas de EC.
Stricture is a very frequent complication of Crohn's disease (CD) patients and defines a specific phenotypic pattern (B2 of Montreal Classification). Approximately 10% of patients estimated to have a structuring pattern at the onset of the disease and one third of patients can develop stricture in the first 10 years of the disease's evolution.1 It is due to chronic transmural inflammation that causes tissue remodeling, mesenchymal cell proliferation and fibrosis2,3 and subsequently, narrow the bowel. The most frequent locations of stricture in CD are the terminal ileum, surgical anastomosis, ileocecal valve and recto sigma.
Fibrotic strictures do not respond to anti-inflammatory treatments. In this point, patients end up having surgery with resection of the affected intestinal segment. On the other hand, it is known that CD frequently recurs after surgery. The risk of endoscopic recurrence is more than 60% after one of surgery and clinical recurrence is estimated to be 20%–25% per year.4 On the other hand, previous studies have reported that new resections were required in 15%–45% of patients at 3 years, in 26%–65% at 10 years and in 33%–82% at 15 years.5
For these reasons, it is imperative to use conservative endoscopic treatments as endoscopic balloon dilation (EBD) in order to avoid new resections. The objective of EBD is to treat fibrotic strictures by increasing the diameter of the intestinal lumen and thus improve the patient's clinic and try to delay and/or to avoid the requirement of new surgeries with the associated morbidity and mortality, and to avoid the subsequent short bowel syndrome.
There are very few studies published to date in which only anastomotic strictures have been analyzed,6 excluding de novo stricture. Only including anastomotic strictures allows us to homogenize patients and to analyze the efficacy of this technique in this type of stricture. Furthermore, the definitions used to stablish the aims in the published studies are variable and not homogeneous and it has not been analyzed whether the type of anastomosis or inflammatory parameters could impact in therapeutic success.
The main aim of this study was to evaluate the efficacy of the EBD in CD patients with anastomotic strictures from a previous surgery. On the other hand, to examine the rate of adverse events of this technique and to determine the factors independently related to therapeutic success by dilation and by patient.
Patients and methodsStudy designObservational study of a cohort of patients diagnosed of CD according to Montreal criteria attended at the tertiary Hospital University and Polytechnic La Fe, Valencia (Spain). The patients had post-surgery anastomosis strictures that underwent EBD and were collected consecutively between January 2009 and June 2019 and follow-up since June 2020.
Characteristics of study populationInclusion criteria were patients with CD over the age of 18 who underwent EBD as a treatment for anastomotic strictures in our hospital. We excluded patients who were under 18 years of age, patients with ulcerative colitis or undetermined colitis and complicated strictures with fistula, abscess and/or perforation. The data was collected from the medical history: demographic data, disease data, current treatments, type of previous surgery and type of anastomosis. Analytical variables (C-reactive protein (CPR) and fecal calprotectin (FC)) at the time of dilation, the characteristics of strictures (length, type), the number of dilations per patient and the adverse events were also collected. We collected the physician therapeutic decision after EBD (switch of treatment, intensification of doses or addition of new drugs).
DefinitionsIn this study, we used the same definitions as Andujar et al. in their study7:
- -
Technical success by dilation: the endoscope managed to pass through the strictures after the procedure and/or managed to increase the caliber of the stricture area.7
- -
Therapeutic success by dilation: it is considered when another endoscopic procedure (stenting or other endoscopic dilation) or surgical treatment was not necessary after 1 year of follow-up after the endoscopic dilation.7
- -
Therapeutic success per patient: when the patient does not require stenting or surgical treatment after follow-up, regardless of the number of dilations required by the patient.7
- -
The adverse events were classified according to the report of an ASGE workshop8:
- -
Adverse event: event which prevents the completion of the planned procedure and/or causes hospital admission, extension of hospital stays, another procedure (with need for sedation/anesthesia) or medical consultation.8
- -
Incident: unplanned event that does not interfere with the performance of the planned procedure or changes in the plan of care.8
After dilatation the grade of recurrence in neoileon was assessed according to the Rutgeerts index.9
Statistical analysisWe recorded data in Excel sheets. Continuous variables were expressed as mean and standard deviation and median with interquartile ranges, while qualitative variables were expressed as frequency and percentage. First, a descriptive analysis was made, analyzing the different characteristics of the included patients and of the dilations that were performed in total during the period of the study.
On the other hand, a descriptive analysis was carried out according to the therapeutic success by dilation and by patient.
A statistical analysis was carried out to evaluate the variables associated with therapeutic success by dilation and by patient. For this purpose, a multivariate analysis was performed both for therapeutic success by dilation and by patient. The odds ratio (OR) and its 95% confidence interval (CI) were calculated to assess the strength of each significant association. Data were analyzed using the SPSS (Statistical Package for Social Sciences).
Ethical statementThe study protocol was approved by the Ethic Committee of Health research institute La Fe. All included patients signed an informed consent authorizing the use of their clinical data for research purposes. Additionally, the study complies with the principles of Good Clinical Practice and the Helsinki Declaration.
ResultsClinical characteristics of patientsThe clinical characteristics of the patients included are shown in Table 1.
Clinical characteristics of patients with Crohn's disease.
| Variable | Patients (n=32) |
|---|---|
| Mean (SD)/n (%) | |
| Median (1st, 3rd) | |
| Age | 45.1 (13.7) |
| 46 (36, 54) | |
| Sex | |
| Man/women | 18 (56%)/14 (44%) |
| Tobacco habit at the time of dilation | 45.15 (13.72) |
| Ex-smoker | 5 (16%) |
| Smoker | 8 (25%) |
| Not smoker | 19 (59%) |
| Location of CD | |
| L1: ileal | 19 (59%) |
| L3: ileocolonic | 12 (37.5%) |
| L4: upper gastrointestinal tract | 1 (3%) |
| Perianal disease | 4 (12.5%) |
| Number of surgeries prior to 1st dilation | |
| 1 | 19 (60%) |
| 2 | 10 (31%) |
| 3 | 2 (6%) |
| 4 | 1 (3%) |
| Time (months) from surgery to first dilation | 13.3 (10.2) |
| 12.2 (4.8, 18.7) | |
| Number of dilations per patient | |
| 1 | 17 (53%) |
| 2 | 9 (28%) |
| 3 | 3 (9.5%) |
| ≥4 | 3 (9.5%) |
A total of 32 patients with CD were included (18 males; mean age 45.15±13.72 years) in which a total of 63 dilations were made. Forty percent of the patients had suffered more than one surgery before the first dilatation. Approximately half of the patients underwent more than one dilatation. Therapeutic success per patient was achieved in 20 patients (62.5%) and 12 patients needed additional surgery (37.5%).
Characteristics of dilatationsThe descriptive analysis of the dilations carried out is shown in Table 2. A total of 63 dilations were performed during the study period. The endoscopic technique was not always performed by the same endoscopist. A total of 5 expert endoscopists have participated. The types of endoscopies used were Olympus 180 high-definition colonoscope, Exera II (CV-180) or Exera III (CV-190) processor, with CO2 insufflation. Two types of CRE™ PRO Wireguided dilatation balloons (Boston Scientific®) of 3 sizes each (12–13.5–15mm or 15–16.5–18mm) were used. The type of balloon used for dilatation was chosen according to the diameter of the stenosis. The dilation protocol is to hold the first and second balloon measurement for 30s and the third measurement for 1min.
Clinical characteristics of the dilations.
| Variable | Dilations (n=63) |
|---|---|
| Mean (SD) | |
| Median (1st, 3rd) | |
| CPR (mg/l) at dilation time | 4 (7) |
| 1.4 (0.7, 4) | |
| FC (μg/g) at dilation time | 182.5 (286.1) |
| 99 (43.2, 176.5) | |
| Ball diameter (mm) | 14.9 (1.8) |
| 15 (14.5, 15) | |
| Medical treatment at dilation time | |
| Infliximab | 3 (4.5%) |
| Adalimumab | 7 (11%) |
| Vedolizumab | 1 (1.5%) |
| Ustekinumab | 1 (1.5%) |
| Immunosuppressant alone (AZA/6MP) | 26 (41.5%) |
| Comboa | 10 (16%) |
| None | 15 (24%) |
| Rutgeerts index at dilation time | |
| i0 | 32 (51%) |
| i2a | 19 (30%) |
| i2b | 6 (9%) |
| i3 | 3 (5%) |
| i4 | 3 (5%) |
Regarding the type of previous surgery, the most frequently was ileocolonic resection (73%) and less frequently ileal resection (22%) and right hemicolectomy (5%).
In 54% of the cases, a mechanical latero-lateral anastomosis was performed, while in the remaining, a manual termino-terminal anastomosis was performed. No statistically significant differences were observed in technical success depending on the type of anastomosis (p=0.315).
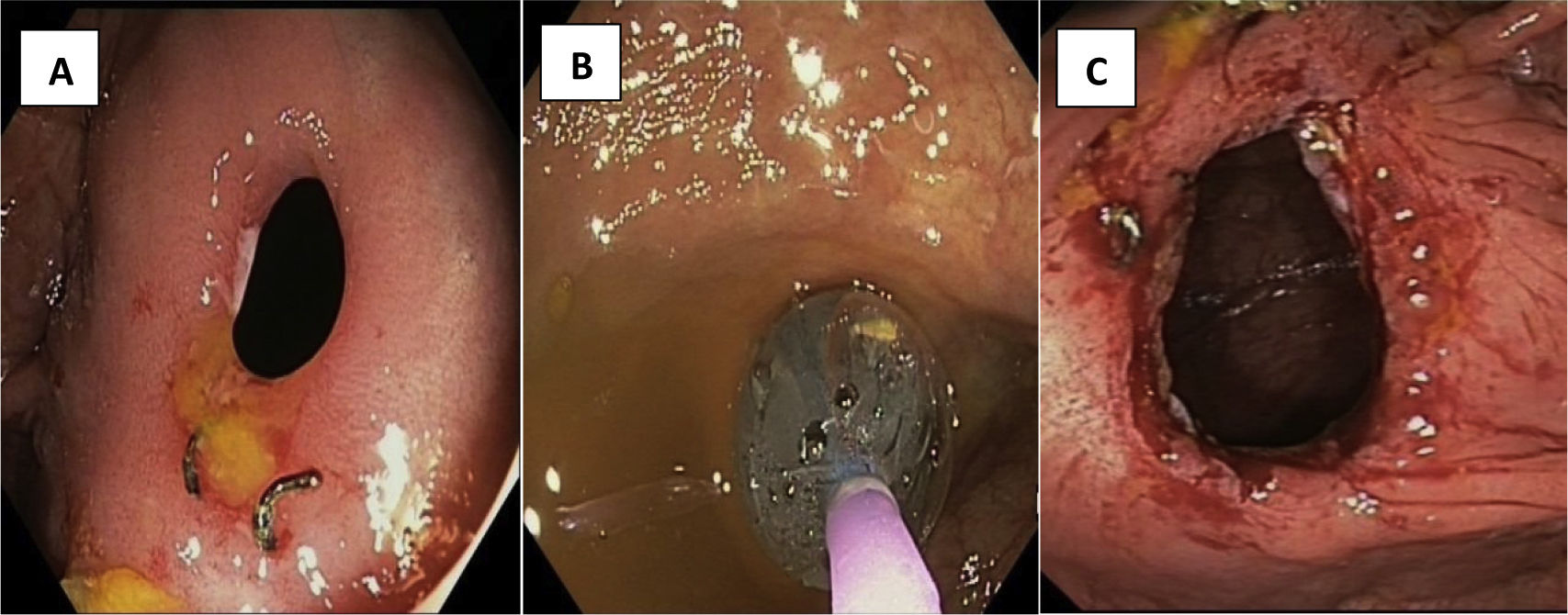
The median strictures length was 35mm. A technical success was obtained in 63.5% (n=40) of the cases and a therapeutic success by dilation were achieved in 59% (n=37) of the cases. Fig. 1 shows an example of EBD performed in a patient with an anastomotic stricture, with technical and therapeutic success.
Regarding to the complications, the percentage of post-dilatation adverse events was 3.1% (one micro perforation and one bleeding requiring hospitalization and blood transfusion) and the frequency of post-dilatation incidents was 4.8% (two self-limited bleedings and one mucosal tear).
Most strictures (64%) were purely fibrotic, 19% were ulcerated or inflammatory, and 17% had a mixed fibrotic-ulcerated component.
After EBD, the 81% of patients did not show recurrence (i0–i2a).
Treatment modifications after EBDTreatment was not modified after 30 (48%) EBD. In 9 (14%) cases, after EDB the physician maintained the patient without treatment. In 3 (5%) cases, after EBD the physician managed to withdraw all treatments. Surgery was employed after 12 (19%) EBD, in 12 of the 32 patients (37.5%). Treatment modifications were made after 9 (14%) EBD:
- -
Start infliximab monotherapy: 1 case.
- -
Start mercaptopurine monotherapy: 2 cases.
- -
Start infliximab and azathioprine combo therapy: 1 case.
- -
Adalimumab intensification (40mg each two weeks to 40mg weekly): 1 case.
- -
Switch infliximab to adalimumab: 2 cases.
- -
Infliximab dose reduction: 2 cases.
A multivariate analysis was performed to establish the variables that independently influenced therapeutic success per dilation (Table 3) and per patient (Table 4). In both cases, the length of the strictures has a statistically significant influence. The higher length of the strictures leads lower probability of therapeutic success by dilation and by patient. In contrast, the type of anastomosis and the FC values did not influence in the results. Similarly, there was no difference in therapeutic success based on treatment at the time of dilation (biological and immunomodulator therapy). On the other hand, the higher Rutgeers index was correlated with a lower probability of therapeutic success per dilation, with a certainty of 91%. No statistically significant differences were observed in the technical success according to the type of anastomosis (p=0.315).
Multivariate analysis of therapeutic success per dilation.
| Variables | Estimate | Standard error | OR | Lower 95% | Upper 95% | PDa |
|---|---|---|---|---|---|---|
| Length of stricture (mm) | −0.14 | 0.09 | 0.87 | 0.7 | 0.98 | 99.7% |
| Anastomosis type | 0.94 | 1.81 | 2.56 | 0.05 | 100 | 71.4% |
| Ball diameter (mm) | 0.15 | 0.33 | 1.16 | 0.61 | 2.27 | 67.4% |
| Fecal calprotectin logarithm | 0.12 | 0.67 | 1.12 | 0.33 | 4.66 | 54.7% |
| Rutgeerts index | −1.37 | 1.19 | 0.25 | 0.01 | 1.58 | 91% |
Multivariate analysis of therapeutic success per patient.
| Variables | Estimate | Standard error | OR | Lower 95% | Upper 95% |
|---|---|---|---|---|---|
| Length of stricture median | −0.074 | 0.031 | 0.929 | 0.868 | 0.981 |
| CPR dilation median logarithm | −0.067 | 0.489 | 0.935 | 0.368 | 2.547 |
| FC median logarithm | −0.64 | 0.615 | 0.527 | 0.15 | 1.724 |
| Ball diameter median (mm) | 0.326 | 0.334 | 1.385 | 0.725 | 2.75 |
| Anastomosis type | 0.43 | 1.036 | 1.537 | 0.21 | 12.529 |
This study analyzes the effectiveness of EBD for the treatment of anastomotic strictures in patients with CD. According to the ECCO guidelines10 published in 2019 and a recent review,11 EBD appears efficacious and safe for anastomotic strictures under 4–5cm in length in the short term12.
In our study, therapeutic success per patient was 62.5% with a median follow-up of 6 years. This data is lower than the 73% of patient's surgery-free obtained in a meta-analysis with a follow-up period ranging from 15 to 70 months.13 This could be due to the shorter follow-up period compared to our study and because one third of our patients had ulcerations in the strictures, which is associated with a lower therapeutic success.
In 2015, a study6 was published in which only anastomosis strictures were included. 18% of the included patients required a new surgical intervention during the follow-up, whereas in our study this figure is 37.5% of the patients. This could be due to the fact that the median length of the strictures was shorter (20mm vs. 35mm in our study), with length being a predictive factor for therapeutic success described in previous studies11,13–17 and confirmed in our study.
In relation to the technical success by dilation was 63.5%, which is lower than the figures published in previous articles that are close to 90%.6,18–20 Two reasons could explain this difference: firstly, the median of the dilation balloon used was 15mm compared to the 18–20mm used in the other studies and secondly, 40% of our patients had more than 2 previous surgeries, which results in technical difficulties secondary to the angulation of the anastomosis and the presence of adherences that hamper the advancement of the endoscopy.
We highlight the absence of previous data about the influence of the inflammatory load measured by CPR and FC, and the therapeutic success rate by dilation and by patient. Although FC and CPR levels are well correlated with higher degree of inflammation, their levels did not correlate statistically significantly with therapeutic success. In multivariate analysis, it was observed that the higher the Rutgeerts index was correlated with lesser probability of therapeutic success by dilatation, with a 91% probability that this effect is real. The 3 EBD performed with a Rutgeerts index i4 (large ulcers with diffuse mucosal inflammation or nodules or strictures in the neoterminal ileum) presented FC levels above 1000μg/dL and CPR above 5mg/L, with endoscopic treatment failure in all 3 cases. When analyzing the adverse events, it should be noted that in the two endoscopic dilations in which some adverse event occurred, the index of Rutgeerts was i4 with a high inflammatory load. This date may indicate that cases with significant inflammation at the time of EBD are associated with a lower therapeutic success rate and a higher risk of complications, being a priority to adjust medical treatment prior to dilation in order to decrease this inflammation and the risk of complications, according to previous studies.6,7,11
No differences were found in therapeutic success by dilatation according to medical treatment at the time of dilatation. Moreover, after EDB, in the majority of cases (81%) no post-surgical recurrence (≤i2a) was observed, which justifies the physician's decision of not employing or adding immunosuppressive treatments in most patients. In addition, we had observed that EBD can be a technique that avoided or delayed the surgery in CD patients with higher possibilities of disease recurrence, because they had previous surgery, and in which the possibilities of medical treatments were limited, since they had fibrotic anastomosis.
It is being demonstrated that EBD seems a safe technique. Previous published data had reported a rate of 11% of severe complications.21–24 The percentage of post-dilatation adverse events in our study was lower and only occurred in patients with ulcerated anastomosis as we explained above.
This study has some limitations. First, it was a single-center study with a limited number of patients. Secondly, the data collection was performed retrospectively. And finally, the endoscopy technique was not centralized and performed by the same endoscopist. In contrast, the main strengths of the study are that we only included anastomotic strictures, allowing the homogenization of the sample and the influence of previously un-analyzed variables (CRP, fecal calprotectin and type of anastomosis) in the therapeutic success rate of EBD.
In conclusion, EBD seems a safe technique in short post-surgical anastomosis strictures in CD patients. This technique can avoid the need for new surgery and thus to prevent short bowel syndrome, morbidities, malnutrition, vitamin deficiency and to prevent unnecessary treatments in CD patients.
Ethical considerationsInformed consent was obtained from all the patients studied and all the ethical procedures were carried out. Approval was obtained from the Clinical Research Ethics Committee of our center.
FundingThis research has not received specific support from public sector agencies, the commercial sector or non-profit organizations.
Conflict of interestNone.