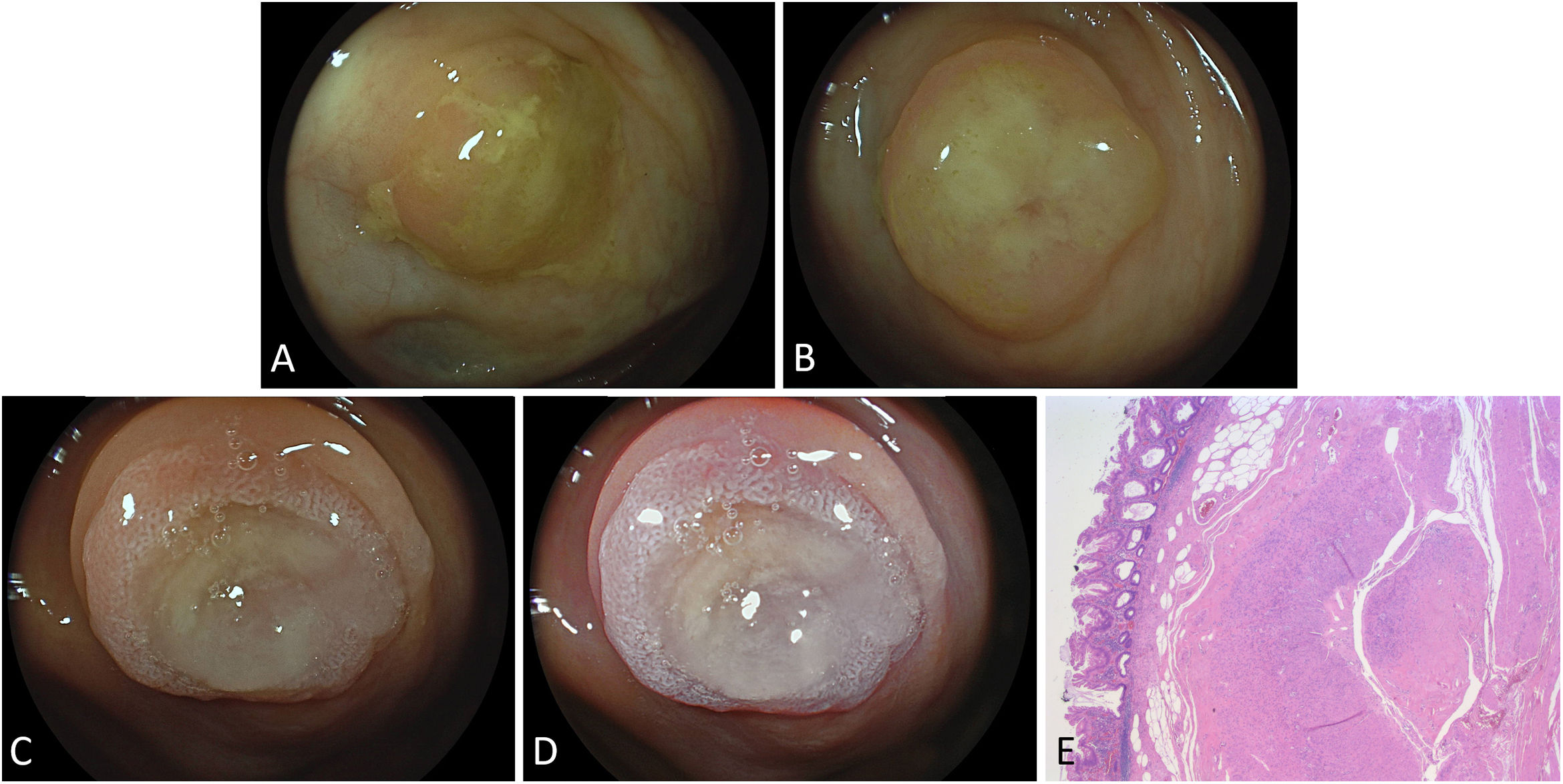
A 50-year-old female patient with a remote history of appendectomy was referred for work-up of a large hepatic mass lesion due to right upper quadrant pain. Apart from, among other examinations, an uncomplicated percutaneous fine needle biopsy (post-hoc diagnosis of advanced intrahepatic cholangiocarcinoma referred for major liver surgery), the patient underwent upper and lower endoscopy despite having had a presumably unremarkable colonoscopy 6 months before. With an optimal cleanliness throughout the whole colon (total Boston Bowel Preparation Scale score 9), in the cecum, the appendix rest was obscured by a thick mucus layer, exhibiting a classical, though oftentimes misinterpreted as staining “cecal mucus sign”1 (Fig. 1A), unrelentingly defying water jet cleansing. To better clarify the underlying pathology intensive washing and 1% acetic acid spraying, highlighting related mucosal changes in presumed serrated sessile adenoma/polyp (SSA/P) as suggested by preliminary study data and clinical experience2,3 (Fig. 1C). Albeit the lesion's center remained somewhat blurred by very tenacious mucus hard to be removed, the peripheral rim exhibited typical features of an SSA/P lesion, including “dark spots inside crypts” as per WASP classification (Workgroup serrAted polypS and Polyposis), reflective of dilated crypt openings due to related mucus production (Fig. 1D – highlighted by linked colour imaging). The patient underwent an uncomplicated device-assisted endoscopic full-thickness resection with the ancillary use of an anchor to fully center and lift the appendix rest (not shown). Albeit a transmural resection at the markedly scarred appendix rest was not achieved, final pathology of the 26×22mm specimen with a 10×9mm measuring flat polypoid lesion confirmed R0 resection of an SSA/P without dysplasia (Fig. 1E). Clinical follow-up at two months excluded any delayed complication.
(A) The “cecal mucus sign” obscuring endoscopic visualization of the appendix rest, (B) unrelentingly defying water jet cleansing. (C) Clear-cut lesion margins and highlighting of mucosal pathology after intensive washing followed by ancillary spraying of 1% acetic acid on white light imaging. (D) Image-enhanced endoscopy using linked colour imaging highlights features of an SSA/P lesion with “dark spots inside crypts” as per WASP classification reflective of dilated crypt openings. An uncomplicated device-assisted endoscopic full-thickness resection (EFTR) was performed using an anchor to center the lesion and mobilize deeper wall elements with a view to marked post-surgical fibrosis (not shown). (E) Histopathology of the SSA/P lesion with confirmed R0 resection and marked fibrosis in the deep muscle layer (H&E, 2.5×).
Nothing to declare.