Thrombosis of the splenoportal axis not associated with liver cirrhosis or neoplasms is a rare disease whose prevalence ranges from 0.7 to 3.7 per 100,000 inhabitants. However, this entity is the second most common cause of portal hypertension. Prothrombotic factors are present as an underlying cause in up to 70% of patients and local factors in 10–50%. The coexistence of several etiological factors is frequent. Clinical presentation may be acute or chronic (portal cavernomatosis). The acute phase can present as abdominal pain, nausea, vomiting, fever, rectorrhagia, intestinal congestion, and ischaemia. In this phase, early initiation of anticoagulation is essential to achieve portal vein recanalization and thus improve patient prognosis. In the chronic phase, symptoms are due to portal hypertension syndrome. In this phase, the aim of treatment is to treat or prevent the complications of portal hypertension. Anticoagulation is reserved to patients with a proven underlying thrombophilic factor.
La trombosis del eje esplenoportal (TVP) no asociada a cirrosis hepática o neoplasias es una enfermedad rara con prevalencia que oscila entre el 0,7 y el 3,7 por 100.000 habitantes. Sin embargo, es la segunda causa de hipertensión portal. Hasta el 70% de los pacientes presentan factores protrombóticos como causa subyacente y entre el 10 y el 50%, factores locales. Es frecuente la coexistencia de varias entidades etiológicas. La presentación clínica puede ser aguda o crónica (cavernomatosis portal). La fase aguda se puede manifestar como dolor abdominal, náuseas, vómitos, fiebre, rectorragia, congestión intestinal e isquemia. Es esencial el inicio precoz de la anticoagulación en esta fase para conseguir la recanalización portal y, con ello, mejorar el pronóstico del paciente. En la fase de cavernomatosis portal, los síntomas vienen derivados del síndrome de hipertensión portal. En esta fase el tratamiento va dirigido a tratar o prevenir las complicaciones de la hipertensión portal. La anticoagulación quedará reservada a aquellos pacientes en los que se demuestre un factor trombofílico subyacente.
Portal vein thrombosis (PVT) is obstruction of the portal vein, with or without extension to other segments of the splanchnic venous system (splenic vein or superior mesenteric vein). The term, however, does not include isolated thrombosis of the splenic or superior mesenteric veins. Since PVT associated with cirrhosis or due to tumour invasion or compression has different therapeutic and prognostic implications, these should be considered different entities.1–8 This paper refers only to non-cirrhotic, non-tumour PVT.
PVT can be classified as acute or chronic, constituting successive stages of the same disease. Although the causes are the same, clinical manifestations and management differ for each stage.3–6,8–11
Optimal management of patients with PVT is based initially on proper patient identification. Familiarity with the clinical manifestations of the disease will increase clinical suspicion, and evaluation of imaging tests by radiologists will be essential for making the correct diagnosis. Diagnosing the disease or risk factor that caused the thrombosis is also crucial. Finally, specific treatment of the PVT and its complications is vital.
Clinical manifestationsThe clinical manifestations depend on the developmental stage at which the PVT is detected (acute vs chronic) and the thrombus extension. PVT can be diagnosed in the acute phase, but this initial episode often goes unnoticed and the PVT is diagnosed in the chronic phase, when the patient has developed portal cavernoma. In recent years—thanks to better understanding of this disease and the availability and improvement of radiological techniques—this trend appears to be changing so that, at present, PVT is more frequently diagnosed in the acute phase. It is sometimes very difficult to differentiate an acute thrombosis from a re-thrombosis on a previously undetected portal cavernoma.
Acute portal vein thrombosisThe main manifestation is usually abdominal pain, accompanied by non-specific symptoms such as fever, general malaise, systemic inflammatory response and dyspeptic symptoms (nausea and postprandial fullness). Symptoms often overlap with those of the local triggering factor (e.g. recent surgery, acute/chronic pancreatitis, colitis, etc.). If the thrombosis affects the mesenteric venous arches, the patient can develop intestinal ischaemia that can lead to intestinal necrosis. This should be suspected when there is abdominal pain, haematochezia, signs of peritonism, intra-abdominal free fluid and metabolic acidosis with renal or respiratory failure. The onset of intestinal stenosis may be the late sequela of mesenteric venous ischaemia. Recent series have shown a marked decrease in the incidence of intestinal ischaemia in patients in whom anticoagulation is instigated promptly.2,11,14,15,17,18
Gastro-oesophageal varices can appear early on (1 month after the acute episode), but in other patients, onset can be delayed a few months and then manifest in the form of variceal bleeding.2,3,5,9,11 Early screening of varices 2–3 months after the acute episode is therefore recommended in patients with acute PVT, and again at 6–9 months in cases in which the varices are not present in the initial endoscopy and the PVT has not been recanalized.2,8,11–17
Isolated thrombosis of a large intrahepatic portal vein branch (lobar or segmental) is a special situation that is often detected incidentally,5,9,11,14,15 and can be accompanied by a moderate, transient increase in transaminases. Atrophy of the affected hepatic territory may subsequently occur, with hypertrophy of the rest of the parenchyma, but portal hypertension does not usually develop.
Chronic portal vein thrombosis. Portal cavernomaAfter an acute PVT episode, the collaterals that make up the cavernoma form within a few days and stabilise within 3–5 weeks.12,15,19 At the same time, vasodilation of the hepatic arterial territory occurs in response to decreased portal venous flow.14,18 The activation of both mechanisms enables the total hepatic blood flow to remain stable or decrease only minimally, while portal vein pressure increases.
Portal cavernoma or chronic PVT is usually diagnosed incidentally during an endoscopic or radiological study performed in a patient with thrombocytopenia, splenomegaly or other signs of portal hypertension.3–6,8,10,14,20 The complications of portal hypertension are the main clinical manifestations of portal cavernoma. Early endoscopy is therefore recommended to rule out the presence of varices. There is no evidence to recommend a specific screening regimen for varices in patients in whom these are not observed in the initial endoscopy. However, once the cavernoma has been established and “stabilised”, the risk of varices in patients who have not already developed them in the early years might be lower. Nevertheless, further research is needed to confirm this, so current recommendations suggest the same practice established in cirrhotic patients, namely endoscopy every 2 years. The prevalence of ectopic varices is higher than in cirrhotic patients, although portal hypertensive gastropathy is rarer.14,23–25
Gastrointestinal (GI) bleeding from oesophageal varices is the most common clinical manifestation in both children14,26 and adults.23,24,27 Predictive factors for variceal bleeding are the size of the varices and history of previous bleeds. Although the severity and transfusion requirements may be high, the associated mortality is lower than in cirrhotic patients.4,6,28,29
Patients with portal cavernoma can also present ascites, which is usually associated with the existence of triggering factors (upper GI bleeding, infection, etc.). Ascites is usually easy to manage and resolve with diuretic treatment or by resolving the precipitating factor.28,30–32 In the case of ascites that are difficult to manage, an additional cause must always be ruled out. While clinical encephalopathy is less common than in patients with cirrhosis, patients with portal cavernoma can develop minimal hepatic encephalopathy,1,28,33 although its impact on the quality of life of these patients has yet to be defined.
Recurrent thrombotic episodes are another common complication.4,6,8,10,29 The presence of an underlying prothrombotic factor is an independent factor for re-thrombosis.4,6–8,34,35
Liver function tests are minimally altered and liver function is normal in general.
Portal cavernoma cholangiopathyPatients with portal cavernoma can present alterations of the intra- and extrahepatic bile ducts and gallbladder, called portal cavernoma cholangiopathy (PCC).17,36 The most widely accepted pathophysiological mechanism for its onset is compression of the bile duct by the large periportal collaterals that grow in the hilar and perivesicular zone, and an ischaemic component due to poor portal venous flow or prolonged compression by the collaterals.3,5,6,9,11,37,38
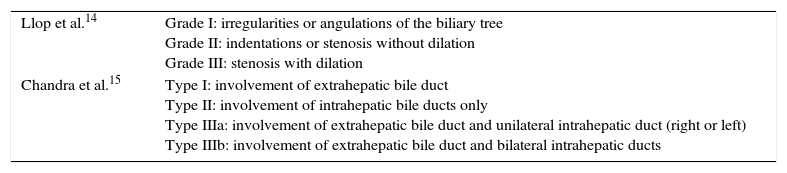
The prevalence of PCC in magnetic resonance (MR) cholangiography is very high (over 80%).3,5,9,11,14–17 There are 2 classifications of PCC to date3,5,9,11,14,15: one being an anatomical classification based on the extension of the biliary lesion,3,5,9,15,38 while the other is based on the type of biliary lesion and also shows a clinical-radiological correlation (only patients with grade III present biliary complications) (Table 1).14,37,39,40 Despite the high prevalence of radiological alterations, clinical manifestations of PCC are rare. Only 5% to 35% of patients in the series studied presented complications such as jaundice, abdominal pain, gallstones and cholangitis,3,5,14,20,41–44 and only cases of severe PCC (grade III) developed symptoms.14,45,46 Moderately elevated cholestatic enzymes with normal bilirubin and discretely elevated transaminases is a much more common finding.
Classification of portal cavernoma cholangiopathy.
| Llop et al.14 | Grade I: irregularities or angulations of the biliary tree Grade II: indentations or stenosis without dilation Grade III: stenosis with dilation |
| Chandra et al.15 | Type I: involvement of extrahepatic bile duct Type II: involvement of intrahepatic bile ducts only Type IIIa: involvement of extrahepatic bile duct and unilateral intrahepatic duct (right or left) Type IIIb: involvement of extrahepatic bile duct and bilateral intrahepatic ducts |
Note: The system devised by Chandra et al. is an anatomical classification based on the extension of the biliary lesion, while the one by Llop et al. is based on the type of biliary lesion and also shows a clinical radiological correlation (only patients with grade III present biliary complications).
A recent Spanish series showed that if PCC appears, it does so early on (1 year after the acute PVT episode).14,47,48 The same study showed that radiological progression of this entity is very rare if the portal cavernoma remains stable and there are no re-thrombosis phenomena. Thus, if the patient has not developed cholangiopathy 1 year after an acute PVT, or this is lower than grade III (and therefore with little likelihood of developing symptoms), they are highly unlikely to develop cholangiopathy symptoms during follow-up.3,9,14,38 However, data from an Indian series suggest that PCC is a slowly progressive disease and much more symptomatic. These differences may be due to differing PVT populations: in India, PVT usually presents in childhood, while in the West, it generally occurs in adulthood; the prevalence of idiopathic PVT and choledocolithiasis is higher in India compared to the West.27,43
Diagnosis of portal vein thrombosisDoppler ultrasound is the procedure of choice for first-line diagnosis of PVT.3,28,29,38,49 Computed tomography (CT) or MR angiography should subsequently be performed to confirm the diagnosis.22 These techniques are also very useful for evaluating the extension of the thrombosis, presence of intestinal ischaemia, and presence of local factors (e.g. abscesses, neoplasms, abdominal inflammatory processes) or for diagnosing PVT if the findings on Doppler ultrasound are not definitive.5,28,31
Radiological findings that suggest acute PVT are the presence of iso- or hypoechoic material inside the vein on Doppler ultrasound, presence of hyperdense material on CT prior to the administration of intravenous contrast and the absence of large portoportal or portosystemic collaterals.21,28,33
Radiological findings that suggest chronic PVT are the presence of cavernoma (multiple twisted vessels that replace the normal portal vein) or portosystemic collaterals and splenomegaly.29,50–53 Alterations may also be found in the architecture of the liver (areas of atrophy/hypertrophy), and even nodular images corresponding to areas of nodular regenerative hyperplasia in relation to the impaired hepatic perfusion.2,9,34,35 In these cases, it is important to establish the differential diagnosis of cirrhosis with associated PVT. Biopsy enables underlying chronic liver diseases to be ruled out. Transient elastography (FibroScan) may be useful for non-invasively ruling out or diagnosing cirrhosis.22
MR-cholangiography is the technique of choice for the diagnosis and classification of PCC.9,13,36,54 Endoscopic retrograde cholangiopancreatography (ERCP) should be reserved for symptomatic cases that require endoscopic treatment.
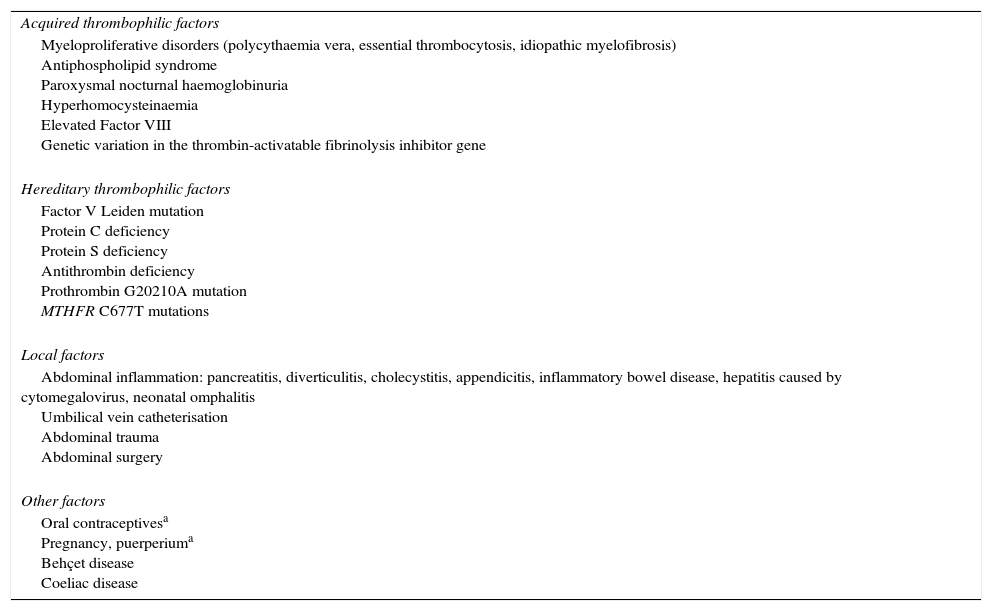
Aetiological diagnosisA prothrombotic factor causing the thrombosis can be identified in up to 70% of patients. A systemic factor is responsible for approximately 60% of these cases, while a local factor is responsible for 20–40% (Table 2).2,3,5,6,9,37,38,55 Several aetiological factors coexist in around 15% of cases.2–5,9 It is therefore vitally important to perform a complete aetiological study despite having identified a local factor or prothrombotic disorder.22 No cause is identified in up to 30% of patients (idiopathic PVT), despite an exhaustive study.2,3,5,9
Risk factors for non-cirrhotic, non-tumour portal vein thrombosis and their prevalence.
| Acquired thrombophilic factors |
| Myeloproliferative disorders (polycythaemia vera, essential thrombocytosis, idiopathic myelofibrosis) Antiphospholipid syndrome Paroxysmal nocturnal haemoglobinuria Hyperhomocysteinaemia Elevated Factor VIII Genetic variation in the thrombin-activatable fibrinolysis inhibitor gene |
| Hereditary thrombophilic factors |
| Factor V Leiden mutation Protein C deficiency Protein S deficiency Antithrombin deficiency Prothrombin G20210A mutation MTHFR C677T mutations |
| Local factors |
| Abdominal inflammation: pancreatitis, diverticulitis, cholecystitis, appendicitis, inflammatory bowel disease, hepatitis caused by cytomegalovirus, neonatal omphalitis Umbilical vein catheterisation Abdominal trauma Abdominal surgery |
| Other factors |
| Oral contraceptivesa Pregnancy, puerperiuma Behçet disease Coeliac disease |
MTHFR: Methylene tetrahydrofolate reductase.
Myeloproliferative neoplasms (MPN) are the main cause of PVT.2,3,5,9,38 The haemodilution and hypersplenism secondary to the portal hypertension can make them difficult to diagnose, as they mask the typical characteristics of MPN (polycythaemia, leukocytosis, thrombophilia).9,37,39,40 It is therefore vitally important to always investigate the presence of these MPNs in all patients, regardless of the full blood count results. The presence of an acquired mutation (V617F) in the Janus kinase 2 (JAK2) gene is present in 90% of cases of polycythaemia vera, and in around 50% of patients with essential thrombocythaemia and idiopathic myelofibrosis. Analysis of the JAK2 V617F gene mutation has thus facilitated the diagnosis of MPNs.9,41–44 However, non-invasive tests (e.g. JAK2 V617F mutation, erythropoietin levels, etc.) do not always allow the MPN phenotype to be defined, so bone marrow aspiration/biopsy must be performed. The association of somatic mutations in the calreticulin (CALR) gene has recently been described in patients with MPN. CALR mutations are present in up to 67% and 88% of patients with JAK2 V617F-negative essential thrombocythaemia and idiopathic myelofibrosis, respectively.9,45,46 It is also present in between 0.7% and 1.9% of patients with splanchnic thrombosis.3,21,47,48
Other far less common acquired diseases are anti-phospholipid syndrome and paroxysmal nocturnal haemoglobinuria. Other hereditary prothrombotic disorders have also been identified, such as Factor II mutation, protein C, protein S or antithrombin deficiency, and less often, Factor V Leiden mutation.3,9,38,56,57 The diagnosis of protein C, protein S and antithrombin deficiencies can be difficult, as values are affected by decreased hepatic synthesis and treatment with vitamin K antagonists. Hyperhomocysteinaemia is a relatively poor risk factor for thrombosis.43,56,58 Close collaboration with the haematologist is therefore essential to obtain a full picture of both hereditary and acquired prothrombotic factors, and for specific management and follow-up.
Pregnancy and the use of oral contraceptives have also been associated with PVT. These 2 hormone factors alone are not sufficient in the absence of an underlying prothrombotic factor, but it seems likely that they could play a role in triggering thrombosis in these cases.3,38,49,59–61
Local factors refer to both infectious-inflammatory diseases (pancreatitis, cholecystitis, cholangitis and appendicitis) and to lesions of the portal venous axis (splenectomy, portocaval shunt and other surgical procedures).3,5,33,62 It is important to remember that the presence of a local factor does not exclude the presence of one or several prothrombotic disorders. Accordingly, a complete evaluation of all aetiological factors is essential.6,22
Prothrombotic factors are rare in children, although a previous history of omphalitis, neonatal sepsis or umbilical vein catheterisation are factors commonly associated with PVT.4,6,50–53
TreatmentTreatment of associated diseasesClose collaboration with the haematologist or other specialists is essential for the proper management of associated diseases, such as MPN, antiphospholipid syndrome or Behçet disease.
Acute portal vein thrombosisAnticoagulationAnticoagulant therapy should be initiated promptly in all patients, unless contraindicated,2,7,9 because spontaneous restoration of patency is rare6,9,13,22,54 and recanalization of the portal vein prevents the development of portal hypertension,2,6,10,55,63 which in turn has an impact on prognosis. Partial or complete recanalization is achieved with anticoagulation in around 40% of patients,2,4,7,9 rising to 60% if therapy begins within the first week after symptom onset, compared to only 20% if started late (within the first month).2,3,21 It is therefore extremely important to initiate anticoagulation as soon as possible. Abdominal pain usually remits in 1–2 weeks. Even patients with extensive thrombi can expect at least partial restoration of patency with these measures. The presence of ascites (even grade I), extension of thrombosis to the splenic vein, presence of various prothrombotic factors and delay in starting anticoagulation have been described as factors that predict failure to recover patency despite anticoagulation.2,9,64 Anticoagulant therapy should be maintained for at least 6 months, as the portal vein can recover patency up to 6 months after treatment has started.9,22,65 Recanalization of the splenic and mesenteric veins can be observed up to 12 months after anticoagulation,3,9 so clinicians should consider maintaining treatment for 1 year in patients with involvement of these veins. In a recent European prospective multicentre study,9 the rate of bleeding complications in anticoagulated patients was very low, and there were no anticoagulation-related deaths. In patients with an underlying thrombophilic disorder, personal or family history of deep vein thrombosis or intestinal ischaemia, it seems reasonable to maintain this treatment indefinitely.3,22,66
Other treatmentsExperience with thrombolysis, surgical or mechanical thrombectomy and transjugular intrahepatic portosystemic shunts (TIPS) is very limited. No studies have evaluated the risk-benefit of these treatments compared with early anticoagulation. Surgical thrombectomy is not recommended, given the high rate of thrombotic recurrence and high morbidity and mortality.5,9,56,57 Experience with percutaneous mechanical thrombectomy or combined with TIPS is very limited and can cause vascular trauma or injury to the portal vein intima, thus leading to recurrent thrombosis.56,58,67 Pharmacological thrombolysis has a recanalization rate very similar to that of anticoagulation, but with a very high rate of complications and treatment-related mortality.59–61,68,69 Considering that the long-term prognosis for patients with chronic PVT is generally good, and that these techniques have high morbidity and mortality, their indication is very controversial.3,5,33,62,67
Chronic portal vein thrombosisAnticoagulationIn non-cirrhotic chronic PVT, the aim of anticoagulation is to prevent re-thrombosis of the splenoportal axis that could exacerbate the portal hypertension syndrome, and to prevent thrombotic phenomena in other vascular territories (both venous and arterial).6,11,70 Anticoagulation should be indicated on an individual basis, and should be considered when there are associated prothrombotic factors or personal or family history of deep vein thrombosis. In patients with oesophageal varices or history of upper GI bleeding due to oesophageal varices, anticoagulant treatment should not be commenced until adequate primary or secondary prophylaxis of upper GI bleeding due to oesophageal varices has been established.
No prospective controlled studies have been conducted to evaluate the risk-benefit of anticoagulation in the prevention of re-thrombosis in patients with portal cavernoma, so any information available is based on retrospective cohorts. Anticoagulation reduces the risk of new thrombotic events in most series,4,6,11,71 although one study showed only a tendency to lower this risk.7,72 These series show that anticoagulation does not increase the bleeding risk,6,16 and even has a positive impact on survival.6,10,63,73 However, one study showed that anticoagulation was a predictor of bleeding, and the presence of a new thrombotic event had a negative impact on survival, whereas anticoagulant treatment and bleeding did not.7,74 It is important to take into account that these studies are retrospective; the impact of anticoagulant treatment on the prevention of thrombosis or on survival was not evaluated separately among patients who had an underlying prothrombotic factor and those who did not; furthermore, management of anticoagulant treatment, or prevention of bleeding due to portal hypertension were not well described.
Treatment of portal hypertensionNo controlled studies have evaluated the management of variceal bleeding in this context. Current recommendations are therefore based essentially on study data from patients with portal hypertension and liver cirrhosis.3,6,22,75 Primary prophylaxis with non-selective β-blockers or endoscopic ligation is recommended in patients with large oesophageal varices (>5mm). Endoscopic eradication of oesophageal varices in patients with non-cirrhotic PVT has been found to significantly reduce the rebleeding risk.65 The combined use of β-blockers and endoscopic ligation is acceptable for secondary prophylaxis.3 No studies have evaluated the best treatment to achieve control of an acute bleeding episode due to gastro-oesophageal varices, but in these patients it seems reasonable to apply the same recommendations made for cirrhotic patients, using vasoconstrictive drugs or endoscopic treatments.21 In the event of medical or endoscopic treatment failure, a TIPS may be inserted, although this may be technically very difficult or impossible due to extension of the thrombosis to other territories such as the splenic or superior mesenteric veins. A recent study found that TIPS were successfully placed in 35% of cases, and also observed much better bleeding control in the TIPS group (69% vs.14%; p=0.057).66 Nevertheless, further studies are required with large patient series to evaluate the real role of this procedure in the treatment of these patients. If TIPS cannot be performed nor rescue surgical shunt anastomosis considered, the clinician needs to identify whether there are potentially shuntable permeable vessels, given that splenic and superior mesenteric vein thrombosis has been observed in up to 50% of patients with PVT,5,9 making shunt surgery impossible. Moreover, if there is a potentially shuntable vessel, it is important to confirm that it will resolve the portal hypertension. The distal splenorenal shunt is the preferred surgical procedure.67 The disadvantages of this treatment are the considerable morbidity and mortality rates, and a high risk of thrombosis of the anastomosis.68,69 In the case of intractable or uncontrollable bleeding, when the previously discussed techniques cannot be performed, other measures may be attempted, such as selective surgical devascularisation (oesophageal transection),67 splenectomy or surgical ligation of the varices. Anastomosis from the mesenteric vein to the permeable intrahepatic portal branch has been successfully performed in children with thrombosis of the portal vein trunk with patent intrahepatic portal veins. This technique allows the portal vein system to decompress while revascularising the liver with portal blood. There is no experience in adults.
Treatment of portal cavernoma cholangiopathyNo studies have prospectively evaluated the following therapeutic recommendations. In asymptomatic patients with radiological PCC, or only a slight increase in cholestatic enzymes, no treatment is recommended. Nevertheless, enzyme changes usually revert with the use of ursodeoxycholic acid. Whether this action can prevent the future development of symptomatic PCC will have to be evaluated in prospective studies. A recently published expert consensus recommends endoscopic biliary sphincterotomy and drainage in symptomatic patients with biliary obstruction (with or without calculi).11,70 The bile duct should be drained by inserting a stent in the common bile duct. The stent often becomes obstructed, and must therefore be changed periodically. Ursodeoxycholic acid may be beneficial in this context, although there is no controlled evidence to support this strategy. Portal decompression by placement of a shunt in the splenoportal axis or TIPS should be reserved for cases of recurrent symptoms despite endoscopic treatment.11,71 There is little evidence of the real efficacy of this technique. It has been suggested that treatment with non-selective β-blockers could be beneficial, as they reduce the portal flow, but this has not been demonstrated.72 Bilioenteric shunts are associated with high morbidity and mortality and are therefore not recommended.16
PrognosisThanks to early diagnosis and subsequent introduction of anticoagulant treatment, 5-year survival in acute PVT is currently 85%. However, if there is intestinal infarction and multiple organ dysfunction syndrome, the mortality can be 20–50%.73 In the case of chronic PVT, overall mortality is less than 10%.74 In more than 50% of cases, the cause of death has no direct relationship with the PVT. When PVT is responsible for the patient's death, in half of cases it is due to a GI bleed and in the rest to extensive or recurrent thrombosis.6 Predictors of survival have not been properly studied, although the main determining factor appears to be advanced age and mesenteric venous thrombosis.73
Conflict of interestsThe authors declare that they have no conflict of interests.
Please cite this article as: Llop E, Seijo S. Actuación ante la trombosis portal no cirrótica no tumoral. Gastroenterol Hepatol. 2016;39:403–410.