Absent contractility is considered a disorder of peristalsis. The literature about the etiology and clinical characteristics is scarce and the evidence on systemic diseases associated with this esophageal disorder is limited. Therefore, we aimed to determine the etiology of absent contractility in our population using the clinical algorithm recently described in the literature.
MethodsWe conducted a retrospective, descriptive study at a single tertiary hospital of all patients diagnosed of absent contractility between May 2018 and February 2020. Data on demographic characteristics, medication, comorbidities, and laboratory and paraclinical tests were recorded from clinical records.
ResultsA total of 72 patients with absent contractility were included for analysis. There was a predominance of female sex (n=43, 59.7%), with a mean age of 55.4 (±15.0) years. We identified a systemic disorder associated with absent contractility in 64 (88.9%) patients. From these, 31 (43.1%) patients were diagnosed with a systemic autoimmune disease, 26 (36.1%) patients were considered to have absent contractility secondary to pathological exposure to acid-reflux and 15 (20.8%) patients were diagnosed with other non-autoimmune systemic disorders. In the remaining eight (11.1%) patients, there were no underlying systemic disorders that could justify the diagnosis of absent contractility.
ConclusionsA systematic approach to search for an underlying cause in patients diagnosed with absent contractility is warranted. Up to 90% of patients with absent contractility have a systemic disorder associated with this condition.
La contractilidad ausente se considera un trastorno de la peristalsis esofágica. La literatura que existe sobre la etiología y las características clínicas es escasa y la evidencia sobre enfermedades sistémicas asociadas a este trastorno esofágico es limitada. Nuestro objetivo fue determinar la etiología de la contractilidad ausente en nuestra población utilizando el algoritmo clínico recientemente descrito en la literatura.
MétodosSe realizó un estudio descriptivo retrospectivo en un hospital terciario de todos los pacientes diagnosticados de ausencia de contractilidad entre mayo de 2018 y febrero de 2020. Se recogieron datos de características demográficas, medicación, comorbilidades y pruebas de laboratorio y estudios paraclínicos.
ResultadosSe incluyeron para el análisis un total de 72 pacientes con ausencia de contractilidad. Predominó el sexo femenino (n=43, 59,7%), con una edad media de 55,4 (±15,0) años. Identificamos un trastorno sistémico asociado con la ausencia de contractilidad en 64 (88,9%) pacientes. De estos 31 (43,1%) pacientes fueron diagnosticados de una enfermedad autoinmune sistémica, 26 (36,1%) pacientes se consideraron con ausencia de contractilidad secundaria a exposición patológica al reflujo ácido y 15 (20,8%) fueron diagnosticados con otras enfermedades no autoinmunes sistémicas. En los 8 pacientes restantes (11,1%) no hubo trastornos sistémicos subyacentes que pudieran justificar el diagnóstico de contractilidad ausente.
ConclusionesUn enfoque sistemático está justificado para investigar una causa subyacente en pacientes diagnosticados de contractilidad ausente. Hasta el 90% de los pacientes con contractilidad ausente tienen un trastorno sistémico asociado con esta afectación de la motilidad esofágica.
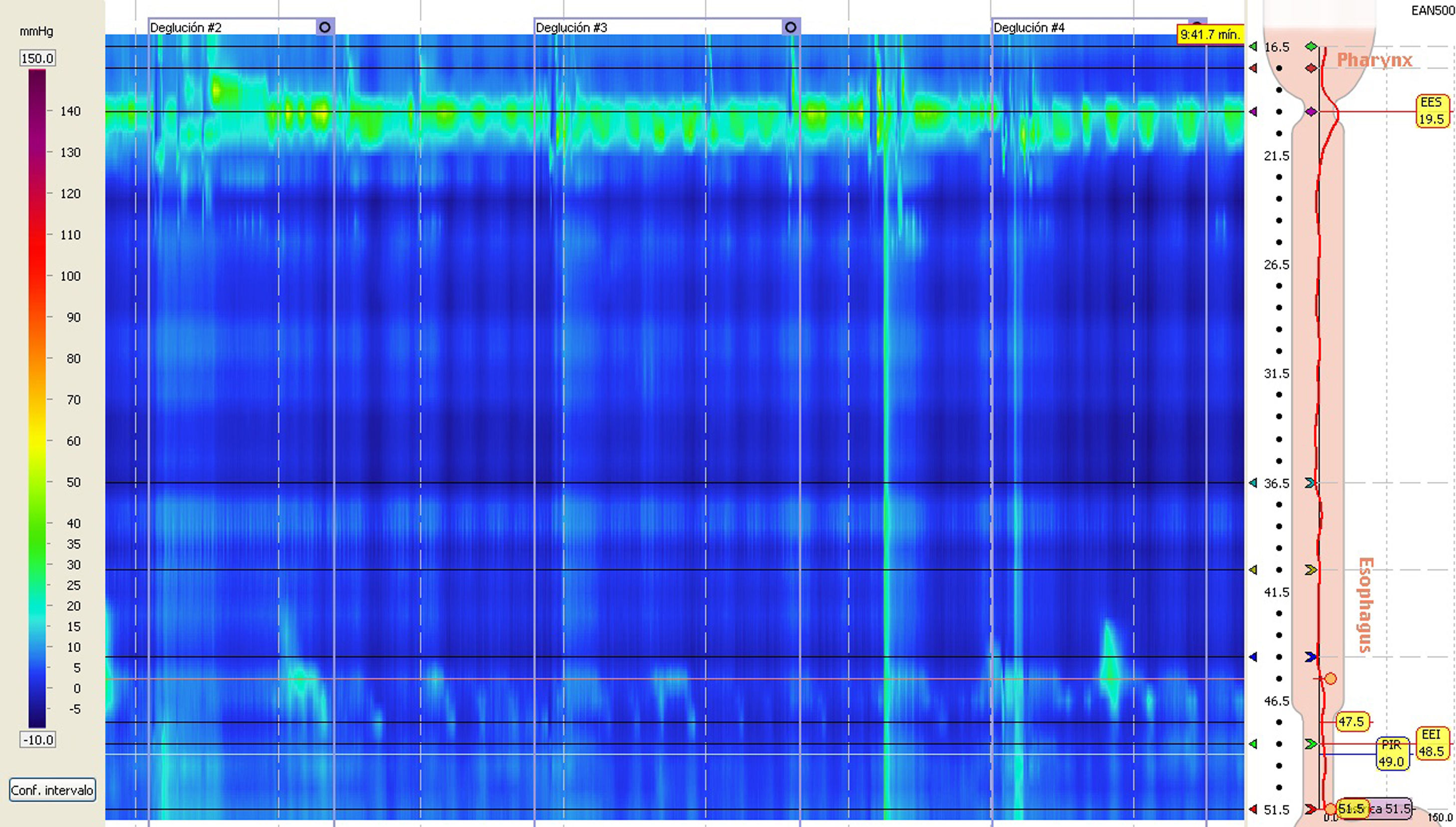
Nowadays, high-resolution esophageal manometry (HRM) is the gold standard test for the evaluation of non-obstructive dysphagia and the diagnosis of esophageal motility disorders.1 Absent contractility (AC) is diagnosed in HRM when all single swallows are failed (DCI<100mmHgmmHgscm) and the lower esophageal sphincter (LES) relaxation is normal (defined by an integrated relaxation pressure (IRP)<15mmHg).2 It is considered a disorder of peristalsis because it is never seen in normal asymptomatic subjects.3 Although it is considered a motility disorder, there is a lack of evidence about the underlying causes and the clinical characteristics of patients with AC in the literature. So far, it has been associated with connective tissue disorders, especially scleroderma (SSc), and it has also been described in patients with severe gastroesophageal reflux disease (GERD). Nonetheless it has been seldom mentioned in association with other esophageal or systemic diseases and, to our knowledge, only two studies have addressed this issue.4,5 Therefore the main goal of the present study is to determine the etiology of AC in our population using the clinical algorithm recently described in the literature.4 As a secondary goal, we also sought to describe the clinical and manometric characteristics of patients with AC in our setting.
MethodsWe conducted a retrospective study at a single tertiary hospital of patients diagnosed with AC between May 2018 and February 2020. All patients with diagnosis of AC on HRM performed during the study period were selected. We proceeded to review the HRM studies and, if compatible with AC, the electronic medical records were reviewed to obtain data on: age, gender, associated medical conditions, surgical history, active medications, autoimmune and infectious serologic antibodies, upper endoscopy, 24-h ambulatory pH monitoring and esophageal emptying tests.
The study protocol was approved by the Institutional Review Board at Hospital Vall d’Hebron.
HRM techniqueHRM was performed using a catheter with 36 solid-state sensors spaced at 1-cm intervals with an outer diameter of 4.2mm (Medtronic, Inc., Shoreview, MN, USA). Patients were studied in the semi-supine position after an overnight fast. After calibration, the catheter was passed transnasally and fixed by taping it to the nose when the pressure from pharynx to the stomach was recorded simultaneously. After a 5-min adaptation period, all patients were provided with 10 swallows of 5mL water administered with a syringe. At the end of the single swallows, subjects were instructed to drink rapidly 200mL of water using a straw. Analysis of the RDC was performed following standard criteria.2 Esophageal body pressurization during RDC was analyzed using the isobaric contour on 30mmHg. HRM tracings were analyzed using ManoView analysis software (Medtronic).
HRM studies that met the Chicago classification v.4.0.2 Criteria for AC, defined as normal median IRP<15.0mmHg and 100% of failed peristalsis without esophageal pressurization, were re-analyzed by two reviewers to corroborate diagnosis and inclusion. Patients with high suspicion to have obstruction during the RDC (high suspicion of achalasia type 1 were excluded.
24-h ambulatory pH monitoring and Esophageal emptying evaluation24-h ambulatory pH monitoring was performed using a single catheter pH testing system (Zephyr, Sandhill Scientific, Inc., Highlands Ranch, CO, USA). The catheter-based pH probe was passed transnasally and positioned 5cm above the upper border of the LES seen during the HRM procedure performed on the same day, all studies were conducted off acid suppression medication. GERD disease was defined according to Lyon Consensus Criteria.6 Esophageal emptying was evaluated by fluoroscopic esophagogram. Patients were instructed to ingest a maximal tolerable amount of low-density barium sulfate suspension (200mL). After ingestion of the barium suspension radiographs were taken at 0, 1, 2, and 5min to determine esophageal stasis by an experience radiologist in the technique and results were considered as a dichotomical variable; compatible with obstruction or no signs of obstruction.
Statistical analysisThe statistical analysis was performed using commercial software (SPSS 20.0, SPSS Inc., Chicago, Illinois, USA). Descriptive statistics were used to characterize all patients included. Continuous variables are shown as means and standard deviation, and categorical variables are shown as n (%), unless otherwise stated. The Kolmogorov–Smirnov test was used to check the normality of data distribution. Fisher's exact test was used for two-group comparisons of categorical variables. For two-group comparisons of quantitative variables, between-group differences were analyzed using the Mann–Whitney U-test. Statistical significance was defined as a p-value<0.05.
ResultsA total of 1317 patients underwent HRM during the study period, from these, 91 patients had a probable diagnosis of AC in their HRM study. Eight studies were excluded because of a history of achalasia or findings consistent with achalasia on clinical testing other than HRM, 2 studies were of poor quality due to a curled catheter, 4 HRM studies were difficult to interpret due to diaphragm not traversed and 5 patients were excluded because they were referred only for esophageal motility testing and had an incomplete clinical history. Seventy-two (5.5%) patients with true AC were included for analysis. Overall, there was a predominance of female sex (n=43, 59.7%), with a mean age of 55.4 (±15.0) years. A complete overview of comorbidities and medication known to alter esophageal motility used is shown in Table 1. The indications for performing the HRM study were non-obstructive dysphagia in 23 (31.9%) patients, suspicion of GERD in 23 (31.9%) patients, and the evaluation of autoimmune disease in 18 (25.0%) patients, the remaining 8 (11.1%) patients had the study performed for other indications; 4 patients with neuropathy and gastrointestinal symptoms to rule-out motility involvement, 2 patients for the evaluation of a dilated esophagus on computer tomography, 2 patients’ oropharyngeal dysphagia.
Characteristics of patients with absent contractility.
| Demographics characteristics | |
| Gender, female, n (%) | 43 (59.7) |
| Age, years, mean (SD) | 55.4 (±15.0) |
| Comorbities | |
| Diabetes mellitus 2, n (%) | 9 (12.5) |
| Hypothyroidism, n (%) | 3 (4.2) |
| DM2+hypothyroidism, n (%) | 1 (1.4) |
| Previous surgery,an (%) | 7 (9.7) |
| Medication | |
| Prokinetics, n (%) | 13 (18.1) |
| Antidepressants, n (%) | 7 (9.7) |
| Prokinetics+antidepressants, n (%) | 3 (4.2) |
| Opioids, n (%) | 2 (2.8) |
| Corticoids, n (%) | 7 (9.7) |
| HRM metrics | |
| LES resting pressure, mmHg, mean (SD) | 13.9 (±11.5) |
| IRP, mmHg, mean (SD) | 3.2 (±3.4) |
DM2, Diabetes mellitus type 2; HRM, high resolution esophageal manometry; IRP, integrated relaxation pressure; LES, lower esophageal sphincter.
Fifty eight patients had an upper endoscopy study performed, from these, 13 (22.4%) patients had severe erosive esophagitis (5 patients with esophagitis grade C or D, eight patients Barrett's esophagus). Nineteen patients had a fluoroscopic esophagogram available without signs of retention in the esophagus, from these, five (26%) patients had a dilated esophagus. Thirty eight patients had 24 hour ph-monitoring performed and out of these 26 (68%) had a pathological acid-reflux exposure according to Lyon criteria.
After the evaluation of clinical records, we identified an underlying etiology associated with AC in 64 (88.9%) patients (Table 2). From these, 31 (43.1%) patients were diagnosed with a systemic autoimmune disease, distributed as follows; 22 (30.6%) patients with limited or diffuse SSc, six (8.3%) patients with mixed connective tissue disease (MCTD), one (1.4%) patient with systemic lupus erythematosus (SLE), one (1.4%) patient with Sjogren's syndrome and one patient with anti-synthetase syndrome. A total of 26 (36.1%) patients were considered to have AC secondary to pathological exposure to acid-reflux, from these, 20 (27.7%) patients were diagnosed following the Lyon consensus criteria on endoscopic and pH-monitoring findings4, five (6.9%) patients were diagnosed with AC after anti-reflux surgery and one (1.4%) patient had a bilateral esophageal vagotomy after neck surgery. Regretfully, preoperative HRM studies were not available in these patients to assess esophageal motility prior to surgery. Interestingly, 15 (20.8%) patients did not have autoimmune diseases or GERD that could justify the finding of AC. Of these, three patients (4.2%) had the diagnosis of chronic intestinal idiopathic pseudo-obstruction (CIPO). Two (2.7%) patients had the diagnosis of type 1 myotonic dystrophy, one (1.4%) patient had eosinophilic esophagitis and one (1.4%) patient had serologically proven Chagas disease. The etiology of AC was classified as unknown in the remaining eight (11.1%) patients, noteworthy, out of these eight patients, one patient had anti-smooth muscle positive antibodies, but no other manifestation of a systemic autoimmune disease and one patient suffered from severe rumination syndrome. In the remaining six (7.3%) patients no underlying etiology could be determined. (Table 2)
Systemic disorders associated to absent contractility.
| Etiology | Patients |
|---|---|
| Autoinmune diseases | 31 (43.1%) |
| Scleroderma (limited and difuse) | 22 (30.6%) |
| Mixed conective tissue disease | 6 (8.3%) |
| Systemic lupus erythematosus | 1 (1.4%) |
| Sjogren's disease | 1 (1.4%) |
| PL-1 anti-synthetase syndrome | 1 (1.4%) |
| GERD related | 26 (36.1%) |
| GERD | 20 (27.7%) |
| Post-nissen | 5 (6.9%) |
| Post bilateral vagotomy | 1 (1.4%) |
| Other systemic diseases | 7 (9.7%) |
| Chronic idiopathic pseudo-obstruction | 3 (4.2%) |
| Myotonic dystrophy type 1 | 2 (2.7%) |
| Chagas disease | 1 (1.4%) |
| Eosinophilic esophagitis | 1 (1.4%) |
| No systemic disorder found | 8 (11.1%) |
| Rumination syndrome | 1 (1.4%) |
| Anti smooth muscle positive antibodies | 1 (1.4%) |
| No etiology found | 6 (8.3%) |
GERD, gastroesophageal reflux disease.
Reviewing the clinical records of patients with AC attributed to non-autoimmune disorders (n=15), we found two patients with evidence of GERD. One patient had Barrett esophagus on endoscopy (1 CIPO), and one patient had pathological acid-reflux in pH ambulatory study (eosinophilic esophagitis).
Overall, in patients with AC, HRM metrics showed a hypotensive LES in 43 (59.7%), with a mean LES resting pressure of 13.9 (±11.5) mmHg and a mean IRP of 3.2 (±3.4) mmHg, we found no statistically significant differences in LES resting pressure or IRP between different etiologies, although the presence of a hiatal hernia was more frequent in patients with GERD than patients without GERD (38.0% vs 15.2% p 0.027) (Fig. 1).
DiscussionEven though AC is considered a disorder of peristalsis, the mechanism and pathogenesis of this disorder is currently unknown and rarely discussed in the literature Laique et al.4 performed a retrospective study on 207 patients diagnosed with AC to assess the clinical characteristics and to determine the associated systemic disorders. Kovac et al.5 aimed to report the clinical spectrum and presentation of patients diagnosed with AC in their center for a two-year period. Interestingly, SSc was the most common etiology in both series. These results are similar to the findings in our study. Worth mentioning, in the work by Laique et al.4 a third of patients with AC did not have SSc or GERD as the underlying cause. By using the diagnostic algorithm proposed4 out of the 33.3% of patients with AC not secondary to SSc or GERD, we could diagnose an underlying etiology in 16 (73.3%) of them. Nonetheless, no underlying etiology could be found in eight (26.7%) patients. We found that systemic autoimmune diseases were the most common primary cause of AC in our series, being the underlying etiology in 43.1% patients, this finding is similar to what is described in Laique et al.4 and Kovac et al. series.5 Systemic autoimmune diseases can cause a variety of gastrointestinal manifestation, and many of them may affect the esophagus. Of note, gastrointestinal manifestations may be the initial presentation of these disorders.7 Esophageal involvement in SSc, has been widely discussed in the literature,8 patients with SSc are an heterogeneous group, although most prevalent esophageal motility disorder is AC, it is important to mention that up to one third of patients with SSc may have normal motility or other motility disorders.9 Amongst the gastrointestinal manifestations of MCTD, the esophageal symptoms are the most common, and can be found in about 85% of the cases.10 Esophageal involvement in other autoimmune diseases, specifically SLE and Sjogren disease, is mostly anecdotal, dysphagia and esophageal symptoms are considered to be multifactorial (decrease saliva production, medication, mucosal ulcers), and esophageal motility disorders motility have been reported sporadically.7 In patients diagnosed with AC, the possibility of a systemic autoimmune disease should always be prioritized and an extensive diagnostic work-up should be performed.
The second most common cause of AC in our series was GERD disease, being the cause in 34.7% patients. Esophageal involvement in GERD has also been described widely.11–13 Not surprisingly, in our study, patients with AC associated to GERD had a higher prevalence or hiatal hernias diagnosed by HRM (38.0% vs 15.2% p value 0.027), which is in accordance with the findings in the series by Kovac et al.5 Also, even if a systemic disorder is the probable cause of AC, patients with AC have prolonged acid exposure due to impaired esophageal clearance and reduced lower sphincter pressure.14 We believe that patients diagnosed with AC should be tested for acid reflux even if asymptomatic (Table 3).
Characteristics patients with absent contractility and other systemic diseases.
| Diagnosis | Gender | Age | Indication HRM | LESrp | IRP | Other findings |
|---|---|---|---|---|---|---|
| Chagas disease | Male | 44 | Dysphagia | 16 | 2.9 | Normal endoscopic study |
| CIPO (MNGIE) | Male | 43 | Dysphagia | 5.3 | 0 | Medium hiatal hernia, gastroparesis |
| CIPO (MNGIE) | Male | 40 | Dysphagia | 1 | 1.7 | Gastroparesis Barrett's esophagus |
| CIPO (idiopathic) | Male | 50 | Dysphagia | 3.1 | 9 | Normal endoscopic and gastric empyting studies. |
| Sjogren syndrome | Female | 51 | Dysphagia | 39.3 | 2 | Normal endoscopic study |
| Myotonic dystrophy type 1 | Female | 60 | Dysphagia | 11.5 | 10.3 | Small Schatzki ring |
| Myotonic dystrophy type 1 | Male | 61 | Dysphagia | 34.3 | 11.1 | Normal endoscopic study |
| Systemic lupus erythematosus | Male | 58 | Evaluation of autoimmune disease | 1.9 | 5 | Dilated esophagus on endoscopic study |
| PL-1 positive Anti synthetase syndrome | Male | 56 | Dysphagia | 11.8 | 3.5 | Normal endoscopic study |
| Eosinophilic esophagitis | Male | 71 | Dysphagia | 21 | 4.2 | Moderate acid reflux on pH monitoring |
| MCTD | Female | 46 | Evaluation of autoimmune disease | 2.7 | 0.3 | |
| MCTD | Female | 46 | Evaluation SD | 4.1 | 0.2 | Severe acid reflux on pH monitoring |
| MCTD | Female | 73 | Dysphagia | 7.2 | 0.5 | Moderate acid reflux on pH monitoring, small Schatski ring, hiatal hernia on endoscopic study |
| MCTD | Female | 31 | Dysphagia | 10.3 | 0 | Severe acid reflux on pH monirtoring, Dilated esophagus |
| MCTD | Female | 46 | Dysphagia | 11.6 | 5 | |
| MCTD | Female | 42 | Suspicion GERD | 48.4 | 1.8 | Normal endoscopic study |
CIPO, chronic idiopathic pseudo-obstruction; HRM, high resolution esophageal manometry; IRP, integrated relaxation pressure; LESrp, lower esophageal sphincter resting pressure; MCTD, mixed connective tissue disease; MNGIE, mitochondria neurogastrointestinal encephalomiopathy; SD, systemic disorder.
In our study eight patients had a variety of non-autoinmune systemic disorders that could justify the finding of AC. Three patients were diagnosed with chronic intestinal idiopathic pseudo-obstruction (CIPO), from these, two patients were diagnosed with mitochondrial neurogastrointestinal encephalomiopathy (MNGIE)15 and one patient remained idiopathic. Evaluated esophageal motility in 14 patients with CIPO using HRM, even though all patients had abnormal HRM findings, only 1 of them had AC. They concluded that there are different grades of esophageal motility impairment that can be identified during HRM, and the most likely explanation is the widespread myopathy or neuropathy in the esophagus.
Two patients had type 1 myotonic dystrophy. Although myotonic dystrophy is primarily characterized by muscular involvement and weakness, multi-system involvement is often present, and the gastrointestinal tract is frequently altered.16,17 Dysphagia in myotonic dystrophy is mostly related to oropharyngeal motility impairment. Still, some studies suggest that esophageal dysmotility involvement may be partially responsible in some cases16,17 studied esophageal motor function on 14 patients with MD using conventional manometry, they found a significant decreases in the esophageal body peristaltic amplitude and a higher incidence of simultaneous waves. They also report that 43% of patients had lack of peristalsis of the esophageal body, resembling to what is known as scleroderma esophagus on conventional manometry, which is highly suggestive of AC.
One patient had eosinophilic esophagitis. Patients with eosinophilic esophagitis usually complain of intermittent dysphagia and may even develop food impaction due to esophageal involvement.18 In patients with this disorder, esophageal motility disorders have been described, especially hypomotility of the esophageal body characterized by weak and failed peristalsis in single swallows, but AC has been also reported in up to 2% of cases.19 In the right clinical setting, patients with AC should undergo esophageal biopsies during endoscopy to rule out eosinophilic esophagitis.
One patient in our series was diagnosed with chronic indeterminate Chagas disease. In Chagas disease, the primary mechanism of esophageal involvement is the loss of the myenteric plexus. In motility studies, this pattern is similar to idiopathic achalasia; however, LES in Chagas disease patients with esophageal involvement tends to be normal or hypotonic,20,21 evaluated esophageal involvement using HRM in 62 patients with chronic Chagas disease, in their cohort, the motility alterations were remarkably mild, and only 22.5% of patients had minor disorders of peristalsis. In the right clinical and epidemiological setting, Chagas disease is a possible explanation for AC.
After a thorough and complete review of medical records and complementary tests, the etiology of AC was classified as unknown in the remaining eight (11.1%) patients. From these, one patient had anti-smooth muscle positive antibodies, but no other manifestations of an autoimmune systemic disease and one patient suffered from severe rumination syndrome that was evident during the HRM study. In the remaining six (7.3%) patients no definitive etiology could be determine, a summary of the radiologic and endoscopic studies performed on these patients is shown in Table 3.
It is important to remember that AC is only distinguished from achalasia type 1 during HRM based on the IRP values, and therefore when the clinical history is highly suggestive, using a timed barium esophagram and/or additional testing may be warranted to safely exclude achalasia.22,23 Our study has some limitations. First, because of its retrospective design we present a heterogeneous population with the diagnosis of AC, and not all patients had all the complementary tests (i.e. esophagogram) performed, as they were only performed on a clinical need-to basis. Still, we believe that our study resembles what gastroenterologist face on real clinical practice, and even though all the tests were not standardized, an underlying etiology could be found in most patients.
Regrettably, treatment for AC is based on dietary modifications since no specific treatment has shown to be beneficial. While there is little room for esophageal body function improvement once the diagnosis of AC is made, the identification of underlying diseases associated with AC that may have multi-system involvement has the potential to early recognition and treatment if available, therefore a systematic approach to search for an underlying cause in patients diagnosed with AC is warranted.
Financial supportLA was supported by scholarships from the Instituto de Salud Carlos III (CM20/00182) and the Societat Catalana de Digestologia (Beca Iniciació Recerca).
Conflict of interestLuis Alcalá, Lucia Relea, Alba Jiménez, Claudia Barber and Elizabeth Barba, declare no conflicts of interest.
None.