We have read with interest the scientific letter of Pineño-Flores C et al.,1 where they describe a subvesical duct injury after laparoscopic cholecystectomy resolved by percutaneous drainage. In this letter, the lesion is described as a type A injury according to the Strasberg classification.2 The type of lesion was determined after an abdominal radiography with contrast which is shown in Fig. 1 of the aforementioned article.
Bile injury during laparoscopic cholecystectomy, one of the most serious iatrogenic complications, occurs due to anatomical misidentification during surgery.3 To prevent them, the technique established is not staying close to the gallbladder wall as recommended in the letter, but to achieve the critical view of safety whenever it is safe to do so.4 The critical view of safety concludes after (1) clearing the hepatocystic triangle, (2) separating the lower on third of the gallbladder to expose the cystic plate and (3) only identifying two structures entering the gallbladder (cystic artery and cystic duct).2
According to the literature of systematic review of subvesical bile ducts made by Schnelldorfer,5 a subvesical bile duct should be defined as any bile duct traversing in close contact with the gallbladder fossa with a tendency to originate from and/or drain into the right lobe. This definition includes from aberrant subvesical bile ducts or hepaticocholecystic bile ducts to accessory subvesical bile ducts or typical anatomy of bile ducts with unusual superficial course, as could be a right posterior sectorial duct. The clinical relevance related to an injury of an accessory bile duct or a superficial typical anatomy bile duct is higher because of the risk of developing hepatic atrophy or repeated cholangitis in the future.
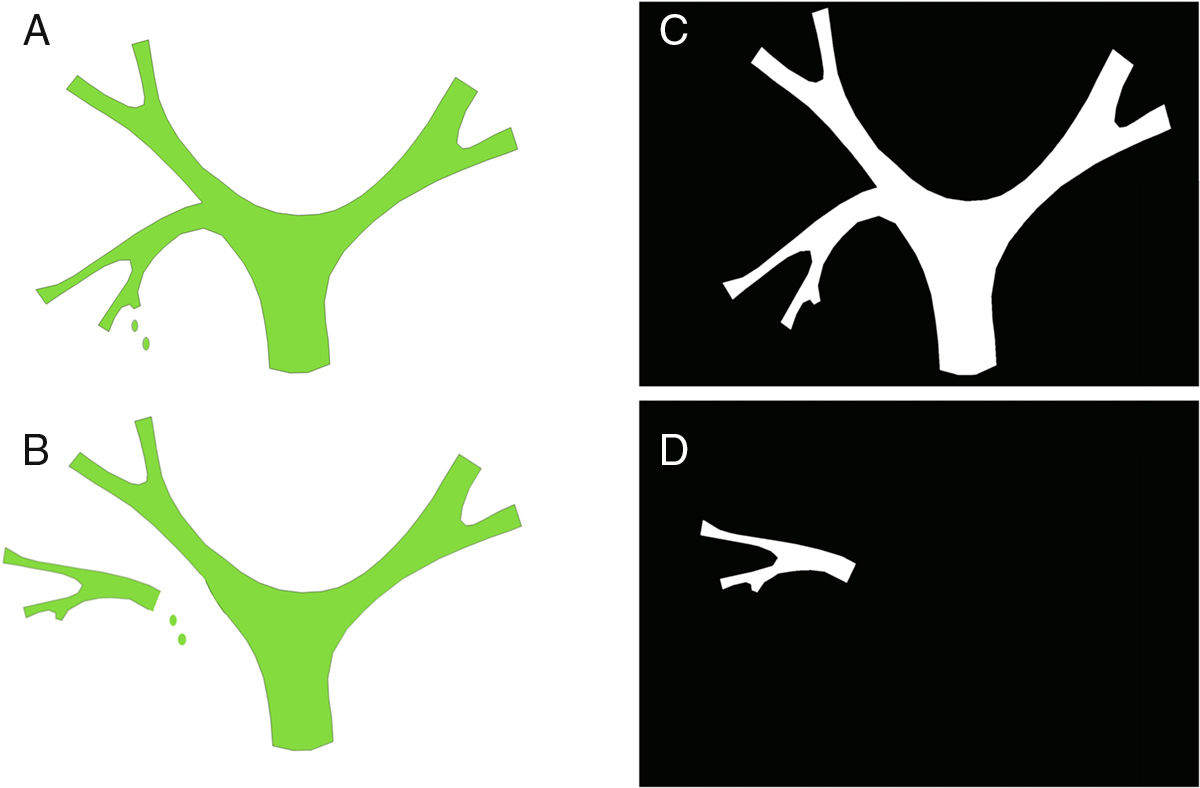
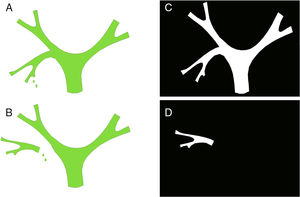
While we agree that we face a subvesical duct injury, we believe the type of injury is poorly classified. A Strasberg type A biliary injury corresponds to a bile leak from the cystic duct stump or a minor biliary radical in the gallbladder fossa. In front of this kind of lesion, we should expect the contrast to enter the radical and spread to the main biliary duct. After revising the radiography aforesaid, we note that the only structure contrasted is a terminal branch without continuation to proximal structures. This image corresponds, to our best knowledge, to a Strasberg type C biliary injury, a bile leak from divided right posterior sectorial duct (Fig. 1).
To end with, we think it is essential to perform a CT scan or MRI some months after the surgery to detect any biliary dilatation. This dilatation would confirm a Strasberg type C biliary injury.