We present the case of a 64-year-old man, with no medical or surgical history of note, who visited the accident and emergency (A&E) department for nonspecific abdominal pain associated with weight loss of 9 kg. He had no diarrhoea, fever, nausea or vomiting. He had no notable family history, had not taken any drugs in the previous few months and had no unhealthy habits. Blood testing showed no significant abnormalities, but due to his weight loss, it was decided to admit the patient from the A&E department for investigation.
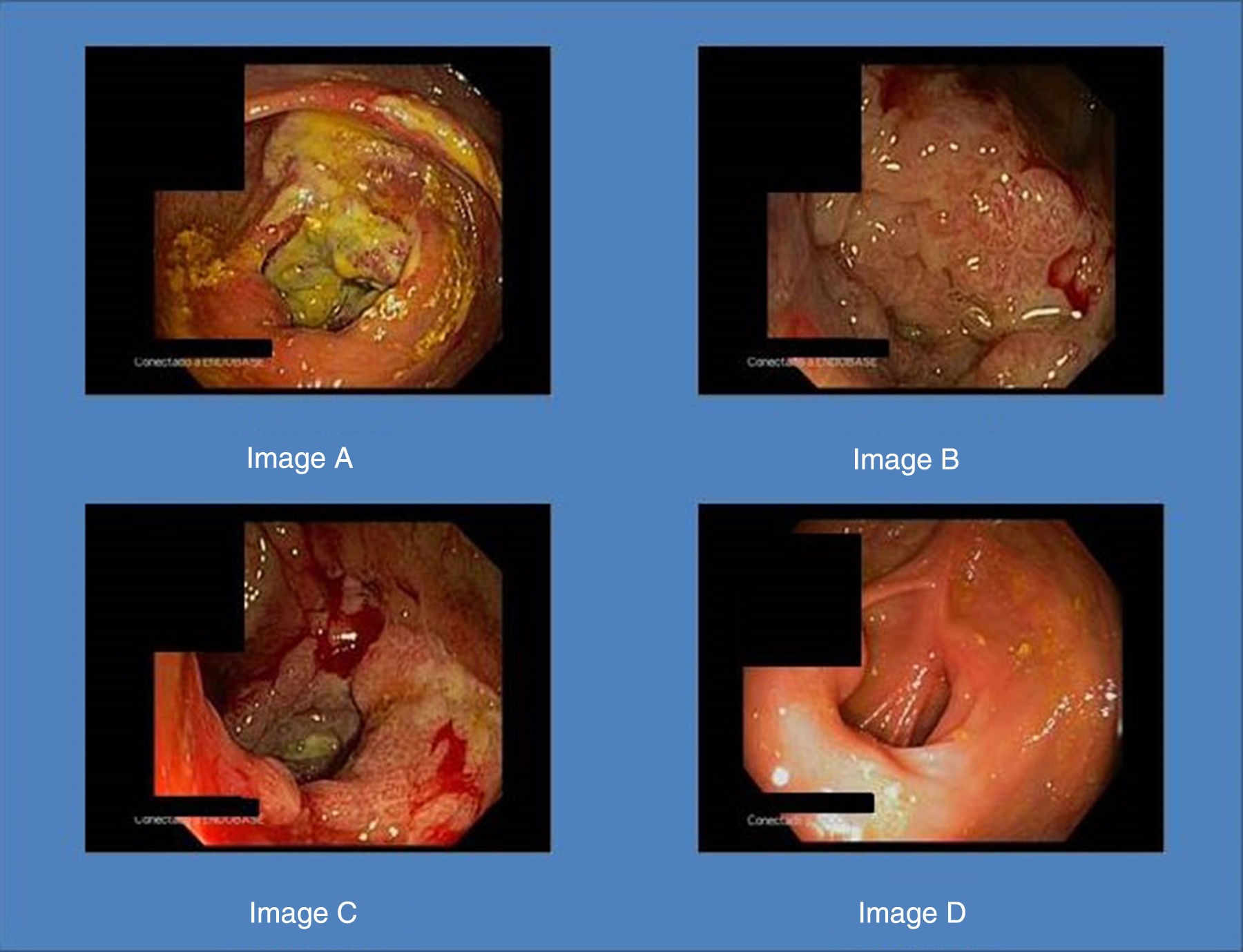
A computed tomography scan of the abdomen revealed asymmetric thickening in the caecum, whereupon a colonoscopy was ordered. It showed an ulcerated tumour occupying the entire caecum, with no abnormalities in the rest of the mucosa (Fig. 1, Image A). The biopsies were inconclusive as regards malignancy. A second colonoscopy was performed (Fig. 1, Images B and C), in which new samples were taken. This time, the immunohistochemical study showed the biopsies to be positive for cytomegalovirus, but not for dysplasia or carcinoma. Serology was positive for cytomegalovirus IgG.
The patient was treated with a 21-day course of oral valganciclovir, 900 mg every 24 h. A repeat colonoscopy two weeks after completion of treatment to assess endoscopic response and ensure healing revealed that the pseudotumour had completely disappeared (Fig. 1, Image D). The patient is currently asymptomatic.
The patient was investigated for possible immunosuppressive factors, but no disease or condition suggestive of a state of immunosuppression were found.
Cytomegalovirus infection can affect any part of the gastrointestinal tract. It is much more likely in patients with HIV, history of transplantation, use of corticosteroids, inflammatory bowel disease or chemotherapy treatment. Among immunocompetent patients, use of corticosteroids and transfusion of blood derivatives have been identified as risk factors for cytomegalovirus colitis.1 Its incidence also increases with age, due to a reduced capacity for action on the part of T cells.
The usual symptoms are abdominal pain and diarrhoea, and up to half of patients may develop rectal bleeding or haematochezia. Endoscopic findings are non-specific.2 A diagnosis should be based on observation of inclusion bodies in non-neoplastic mucosa cells with haematoxylin and eosin staining, and supported by immunohistochemical techniques using monoclonal antibodies. Approximately two-thirds of patients have positive serology.
The most common endoscopic presentation consists of well-defined ulcers and pseudomembranes, but in rare cases, it can appear as a newly formed mass,3,4 in which case, colon cancer must be ruled out.
The treatment of cytomegalovirus colitis is not well established in current guidelines, particularly in immunocompetent patients with no comorbidities, such as our patient.5 Given his good general condition, he was prescribed oral treatment and therefore could be followed up on an outpatient basis with no need to admit him.
Please cite this article as: Casas Deza D, Betoré Glaria E, Sierra Gabarda O, Luzón Solanas L, Gascón Ruiz M, Sierra Moros E. Pseudotumor asociado a citomegalovirus simulando un carcinoma de ciego en un paciente inmunocompetente. Gastroenterol Hepatol. 2020. https://doi.org/10.1016/j.gastrohep.2020.02.015