We present the case of a 60-year-old woman with a history of Crohn’s disease (A2L3B2) and rheumatoid arthritis, for which she had been started on treatment with methotrexate (MTX) three months earlier. She came to the A&E department with spiking fever of up to 38 °C, dry cough and dyspnoea on exertion that progressively increased until she was at rest, with baseline oxygen saturation of 88%. On auscultation of the lungs, dry crackles were heard in both lung bases. Blood tests showed elevation of inflammatory markers, with C-reactive protein (CRP) reading of 10 mg/dl and leucocytosis with neutrophilia.
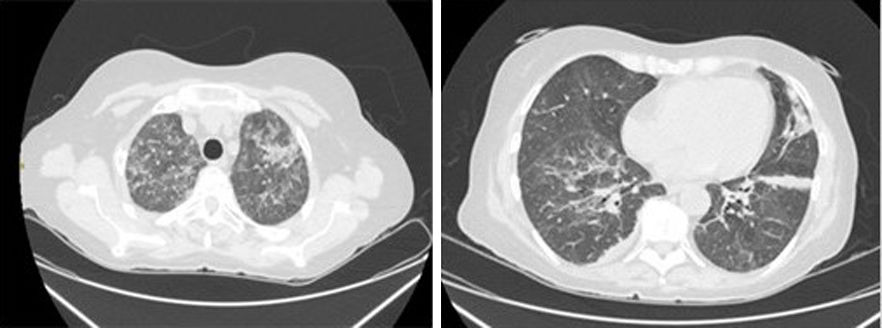
A chest X-ray showed no abnormalities, but chest computed tomography (CT) revealed ground-glass opacities in both lungs.
Pneumonia associated with active COVID-19 infection was ruled out after three negative PCR tests, although the serology (ELISA) was compatible with past infection (positive IgG antibodies). The patient had shown symptoms suggestive of COVID at the beginning of the lockdown during the pandemic three months before her admission, which were not investigated at the time. Spirometry was requested, only showing a moderate decrease in lung diffusion capacity. Finally, bronchoscopy with bronchoalveolar lavage (BAL) showed an increase in lymphocyte cellularity (30%). As MTX pneumonitis was suspected, the MTX was withdrawn and treatment started with methylprednisolone 60 mg/24 h, with clear clinical improvement, no fever and gradual improvement in the patient’s dyspnoea, supporting the diagnosis of MTX-induced hypersensitivity pneumonitis.
MTX is an effective immunosuppressive agent in both induction and maintenance of remission in Crohn’s disease and rheumatoid arthritis. Although it has a high incidence of adverse effects (in up to 50% of patients), commonly in the skin, gastrointestinal tract or central nervous system, most are mild. However some, like pneumonitis, despite being very rare, can be serious.
Although MTX-induced pulmonary toxicity is unpredictable, various risk factors have been identified, including advanced age, diabetes, hypoalbuminaemia, previous lung disease, altered respiratory function tests prior to treatment, and previous kidney or liver damage.1 The mechanisms by which lung injury occurs are unknown, but the pathogenesis is probably multifactorial, including a hypersensitivity reaction, a direct toxic effect, and impaired host resistance to acquired or latent viral infection. There does not seem to be any association with the cumulative dose, the route used or the posology (Fig. 1).
In most patients, pulmonary toxicity develops within the first year (most often in the first months) and can present in an acute, subacute or chronic form, the subacute being the most common. Patients typically develop a non-productive cough, dyspnoea, fever and general malaise.2 Findings on physical examination include tachypnoea, cyanosis and crackles on auscultation. The diagnosis is made from clinical history and suggestive laboratory and radiological results, and after ruling out infections with a similar radiological pattern including, particularly at the moment, the COVID-19 virus. Chest CT may show ground-glass opacities, consolidation, centrilobular lung nodules or traction bronchiectasis. Bronchoscopy with BAL usually detects the presence of lymphocytes and/or eosinophils and an increase in the CD4/CD8 ratio.3 Although rarely necessary, lung biopsy typically shows alveolitis with epithelial cell hyperplasia and, possibly, small granulomas and eosinophilic infiltration.1 Treatment of pneumonitis caused by MTX consists of its definitive withdrawal and the use of oral or intravenous corticosteroids, which should be started after ruling out an infectious cause. However, there are no clear guidelines as to the optimal dose or duration of steroid therapy. Clinical improvement after discontinuation of MTX and/or response to corticosteroid treatment help confirm the diagnosis. The respiratory prognosis is generally favourable, with complete radiological and functional recovery in most cases. However, progression to pulmonary fibrosis occurs in 10% of patients and the approximate mortality rate is 1%.4
Please cite this article as: de los Mozos Ruano A, Casas Deza D, Calvo Galindo R, Solana Hidalgo MP, Aguirre Portu N, Aranda Alonso Á, et al. Neumonitis por metotrexato en paciente con enfermedad de Crohn, durante la pandemia COVID: un caso clínico inusual y revisión de la literatura. Gastroenterol Hepatol. 2021;44:302–303.