Choledocholithiasis causing acute biliary pancreatitis (ABP) may migrate to the duodenum or persist in the common bile duct (CBD). We developed a model for predicting persistent choledocholithiasis (PC) in patients with ABP.
MethodsThis retrospective cohort study included 204 patients, age ≥18 years (mean age: 73 years, 65.7% women), admitted for ABP in 2013–2018, with at least a magnetic resonance cholangiopancreatography (MRCP), endoscopic ultrasonography (EUS), and/or endoscopic retrograde cholangiopancreatography (ERCP). Epidemiological, analytical, imaging, and endoscopic variables were compared between patients with and without PC. Multivariate logistic regression analyses were performed to develop a predictive model of PC.
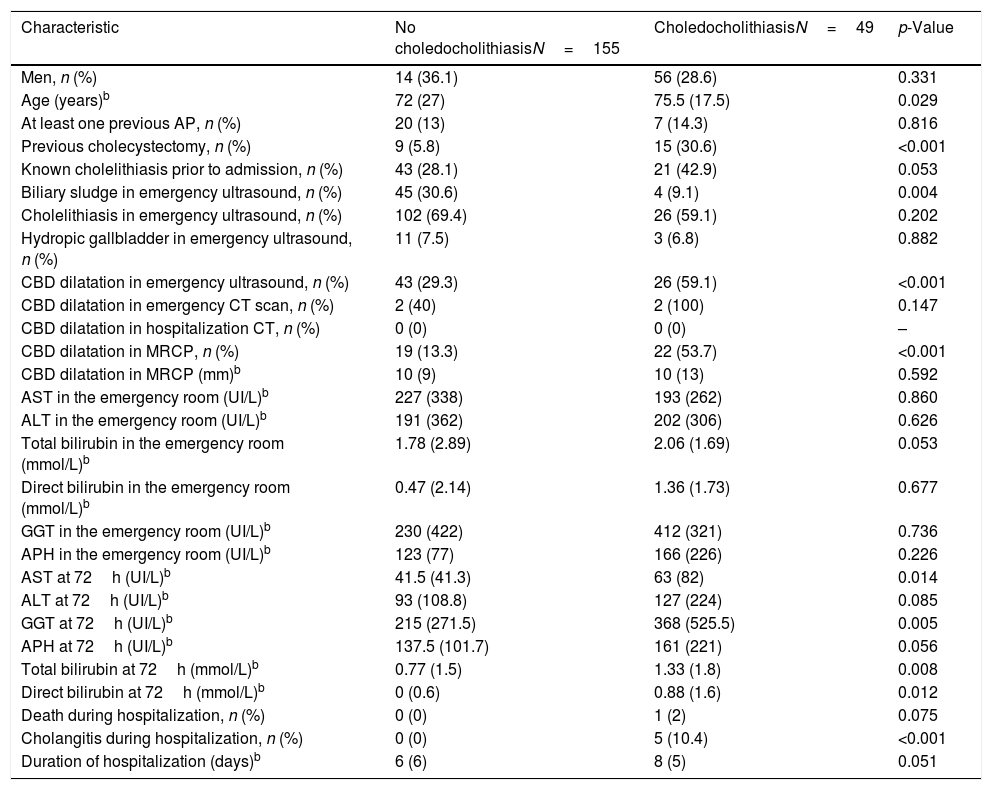
ResultsPatients underwent MRCP (n=145, 71.1), MRCP and ERCP (n=44, 21.56%), EUS and ERCP (n=1, 0.49%), or ERCP (n=14, 6.86%). PC was detected in 49 patients (24%). PC was strongly associated with CBD dilation, detected in the emergency ultrasound (p<0.001; OR=27; 95% CI: 5.8–185.5), increased blood levels of gamma glutamyl transpeptidase, detected at 72h (p=0.008; OR=3.4; 95% CI: 1.5–8.9); and biliary sludge in the gallbladder (p=0.008; OR=0.03; 95% CI: 0.001–0.3).
ConclusionsThe predictive model showed a validated area under the curve (AUC) of 0.858 for detecting PC in patients with ABP. A nomogram was developed based on model results.
ConclusionsThe predictive model was highly effective in detecting PC in patients with ABP. Therefore, this model could be useful in clinical practice.
La coledocolitiasis que provoca una pancreatitis aguda biliar (PAB) puede migrar al duodeno o persistir en el conducto biliar común (CBC). Desarrollamos un modelo para predecir la coledocolitiasis persistente (CP) en pacientes con PAB.
MétodosEste estudio de cohortes retrospectivo incluyó a 204 pacientes, edad ≥ 18 años (edad media: 73 años, 65,7% mujeres), ingresados por PAB entre los años 2013 y 2018, a los que se les realizó al menos una colangiopancreatografía por resonancia magnética (CPRM), una ultrasonografía endoscópica (USE) o una colangiopancreatografía retrógrada endoscópica (CPRE). Se compararon variables epidemiológicas, analíticas, de imagen y endoscópicas entre pacientes con y sin CP. Se realizaron análisis de regresión logística multivariante para desarrollar un modelo predictivo de CP.
ResultadosLos pacientes se sometieron a CPRM (n=145, 71,1%), CPRM y CPRE (n=44, 21,56%), USE y CPRE (n=1, 0,49%) o CPRE (n=14, 6,86%). Se detectó CP en 49 pacientes (24%). La CP se asoció fuertemente con la dilatación del colédoco, detectada en la ecografía de urgencias (p <0,001; OR=27; IC del 95%: 5,8-185,5), aumento de los niveles sanguíneos de gamma glutamil transpeptidasa, detectados a las 72h (p=0,008; OR=3,4, IC del 95%: 1,5-8,9), y barro biliar en la vesícula (p=0,008; OR=0,03; IC del 95%: 0,001-0,3). El modelo predictivo alcanzó un área bajo la curva validada de 0,858 para la detección de CP en pacientes con PAB. Se desarrolló un nomograma basado en los resultados del modelo.
ConclusionesEl modelo predictivo fue altamente efectivo en la detección de CP en pacientes con PAB. Por lo tanto, este modelo podría ser útil en la práctica clínica.
The incidence of acute pancreatitis has increased in recent decades.1,2 Acute pancreatitis is an important cause of morbidity and mortality in Western countries, and it is one of the main causes of hospital admission for digestive reasons.3,4 In most countries, acute pancreatitis is most frequently due to biliary etiology.5 Acute biliary pancreatitis (ABP) is produced by stones traveling from the gallbladder to the common bile duct (CBD). These stones can obstruct the passage of pancreatic juice, which then triggers pancreatitis.6
In one in five patients with ABP, persistent gallstones in the CBD are detected in imaging tests after the patient has presented in the emergency room. Among these patients, only one third experience spontaneous resolution.7 The presence of persistent choledocholithiasis (PC) can predispose to episodes of recurrent pain, acute cholangitis, and the recurrence of pancreatitis in the short term.8,9
Magnetic resonance cholangiopancreatography (MRCP), endoscopic ultrasonography (EUS) or endoscopic retrograde cholangiopancreatography (ERCP) are the most common techniques for diagnosing PC as conventional abdominal ultrasonography has limited accuracy.10 However, those techniques are expensive, endoscopy is invasive, they can increase hospital stay and delay cholecystectom if performed on patients with a low probability of PC.11
Although non-invasive predictive models of PC (based on blood tests and ultrasound findings) have been published previously,10–13 few have focused exclusively on patients with ABP. Most study populations included patients with biliary colic and acute cholangitis.14 Moreover, the pathophysiology of ABP differs from that of choledocholithiasis without pancreatitis.15 Therefore, the predictors of choledocholithiasis identified in those studies might have limited applicability to patients with ABP. On the other hand, studies that focused on patients with ABP exclusively have shown conflicting results.9,16,17
The present study aimed to identify a combination of epidemiological, analytical, and ultrasound variables that could predict the presence of PC in CBD, among patients with ABP.
MethodsDefinitionsAcute pancreatitis was defined according to the revision of the Atlanta classification: at least two of the following three criteria must be met: elevated blood levels of amylase or lipase (>3-fold the upper limit of normal); typical abdominal pain; or typical findings of acute pancreatitis on imaging tests (i.e., CT or preferably nuclear magnetic resonance).18 Biliary etiology for acute pancreatitis was defined as the presence of cholelithiasis or gallbladder sludge on imaging, in the absence of another clear etiology of pancreatitis.16 Biliary etiology was also defined, in cholecystectomy patients without choledocholithiasis in imaging tests, as a history of biliary pathology together with elevated liver markers in analytics, in the absence of other clear etiologies of AP. The gold standard of choledocholithiasis was the detection of stones in the CBD on EUS, MRCP, and/or ERCP. We consider any of these tests as high-technology imaging based on its suitable sensitivity, specificity, positive- and negative predictive values (PPV and NPV, respectively).15,19,20 Persistent choledocholithiasis (PC) was defined as biliary lithiasis in the CBD that did not spontaneously resolve during the interval between arrival at the emergency department and performance of EUS, MRCP, and/or ERCP. Patients were considered to have a PC on cholangiography, when a filling defect could be interpreted as the effect of a stone or biliary sludge.9 CBD dilatation was defined as a CBD diameter>8mm, in patients aged<75 years, or >10mm, in patients aged>75 years.16 Hydropic gallbladder was defined as distended gallbladder with mucus, water, or clear liquid content instead of bile, caused by the prolonged blockage of the cystic duct, usually by an impacted gallstone.21
Study design, patients, and data collectionThis retrospective cohort study was carried out in the Hospital Universitario y Politécnico la Fe, a tertiary hospital in Valencia, Spain. The study was approved by the hospital ethics committee (Medication Research Ethics Committee; registration number 2020-109-1; approval date 07/22/2020). Informed consent was not required, given the retrospective nature of the study, the absence of conflicts of interest among the investigators, and the potential benefit of the study to future patients.
We included adult patients (≥18 years) that visited the hospital emergency department from January 2013 to December 2018 (6 years), were diagnosed with ABP, and underwent a MRCP, EUS, or ERCP during admission or early after hospital discharge. Following the protocol of our center, an MRCP was initially performed. If the result was negative or inconclusive and there was a high suspicion of choledocholithiasis, then EUS was performed. All selected patients were followed up for at least 6 months after hospital discharge. We excluded patients with previous bile duct manipulations, chronic pancreatitis, or previous altered pancreatic or liver blood tests. We also excluded patients that lacked a significant amount of data in their medical records due to lack of tests, loss to follow-up, or referral to their health department. Patients with acute pancreatitis and concomitant acute cholangitis (who had to undergo ERCP within the first 72h) were also excluded.
Data were collected by accessing patient clinical records through the computer programs Orion Clinic® and Abucasis. The collection was conducted over 6 months by several authors of the present study.
VariablesStudy variables included epidemiological data (age and sex), history of biliary diseases, blood parameters of liver function, and ultrasound findings. Variables that indicated liver function included measurements of aspartate aminotransferase (AST, normal value [NV]: 5–34U/L) and ALT (NV: 0–55U/L) in the emergency room, total and direct bilirubin (NV: 0.2–1.2mg/dl) measured in the emergency room, and GGT (NV: 12–64U/L) and alkaline phosphatase (NV: 40–150U/L) measured on admission. We also collected data on liver function measured on the third day of hospitalization (i.e., AST and ALT, total and direct bilirubin, GGT, and alkaline phosphatase). The ultrasound findings included cholelithiasis, choledocholithiasis, dilation of the CBD (mm), biliary sludge, and hydropic gallbladder. Hospital stay was also collected.
Statistical analysisData are expressed as the mean (standard deviation) or median (interquartile range) for numerical variables, depending on whether they had a normal or non-parametric distribution, respectively, based on the Shapiro–Wilks test. Qualitative variables are expressed as the absolute frequency (%). We used T-student or Mann–Whitney U for continuous variables (normal and non-parametric, respectively) and Chi-square (or Fisher's exact test if needed) for categorical variables. A p-value<0.05 was considered statistically significant. To predict the risk of PC we performed a multivariable logistic regression with the factors that seemed to have a greater predictive power. Model performance was evaluated with the unvalidated area under the receiver-operating characteristic curve (ROC-AUC) and a bootstrap-validated ROC-AUC. The Youden and top-left points were used to evaluate the performance of variables in a dichotomous manner. In addition, the conditional plot and its 95% confidence intervals (CIs) were plotted to explore relationships between each variable included in the model. Statistical analyses were performed with R version 4.0, the click R package version 0.4.39, and SPSS version 25.0 (IBM, Armonk, USA).
ResultsWe reviewed the medical records of 753 patients diagnosed with ABP. Of these patients, 204 were finally included in the study. Fig. 1 shows the flow chart of patient selection, with the main reasons for patient exclusion.
Baseline patient characteristicsThe predominant sex was female, with 134 women (65.7%). The median age at the time of acute pancreatitis was 73 (25) years. PC was identified in 49 patients (24%). Among the 204 patients analyzed, 64 (31.4%) had previous gallstones, 24 (11.8%) had undergone a cholecystectomy, and 27 had had a previous episode of acute pancreatitis (13.2%).
Among patients without and with a history of cholecystectomy, there were no differences in age at diagnosis, sex, or the analytical parameters measured in the emergency department or during hospitalization. CBD dilation was found in 60% of patients with and 33.5% of patients without a previous cholecystectomy (p-value 0.020).
In the emergency department, 191 patients (93.6%) underwent an ultrasound scan, and 7 patients (3.4%) underwent a CT scan. The ultrasound findings, in order of frequency, were: cholelithiasis (62.7%), CBD dilatation (33.8%), biliary sludge (24%), choledocholithiasis (8.3%), and hydropic gallbladder (6.9%). During hospitalization, CT was the imaging test performed most frequently (n=21 patients, 10.3%). Analytical data were obtained from the tests performed in the emergency department and at 72h after admission.
Among the 204 patients, 145 patients (71.07%) underwent MRCP only; 44 patients (21.56%) underwent MRCP and ERCP; 1 patient (0.49%) underwent EUS and ERCP; and 14 patients (6.86%) underwent ERCP only. The median time from arrival at the emergency room and completion of the gold standard test was 4 (5) days.
The mean hospital stay was 8 days. Only one death (0.5%) occurred as a consequence of PC, due to sepsis, hypotension and renal failure in an elderly patient.
Baseline characteristics of patients with and without PCCholedocholithiasis was detected in 49 patients (24%). The median age of choledocholithiasis presentation was 75.5 years, and the median age of patients without choledocholithiasis was 72 years (p=0.029). No association was found between patient sex and the presence of PC. A history of cholecystectomy was found in 9 patients without PC and in 15 patients with PC (5.8% vs. 30.6%; p<0.001).
Among the ultrasound findings in the emergency room, the presence of CBD dilatation was significantly associated with the presence of PC, diagnosed with the gold standard test (29.3% in patients without PC vs. 59.1% in patients with PC; p<0.001). However, cholelithiasis was not related to the presence of PC (p=0.200). Biliary sludge was inversely associated with PC; it was present in 30.6% of patients without PC compared to 9.1% of patients with PC (p=0.004).
The median time between tests was 72h (24), and the intervals did not differ significantly between the PC and non-PC groups. In the 72-h analysis, AST, total bilirubin, and GGT were significantly associated with PC. Among patients without and with choledocholithiasis, the median AST levels were 65IU/L and 100IU/L, respectively (p=0.014); the total bilirubin levels were 1.06mmol/L and 1.52, respectively (p=0.008); and the GGT levels were 215IU/L and 368IU/L, respectively (p=0.005).
The groups without and with choledocholithiasis were not significantly different in the length of hospital stay, the death rate, or the number of subsequent episodes of cholangitis, pancreatitis, or cholecystitis. The main demographic characteristics, the history of biliary pathology, the ultrasound findings, and the analytical results are presented in Table 1.
Baseline characteristics of patients without and with PC.
| Characteristic | No choledocholithiasisN=155 | CholedocholithiasisN=49 | p-Value |
|---|---|---|---|
| Men, n (%) | 14 (36.1) | 56 (28.6) | 0.331 |
| Age (years)b | 72 (27) | 75.5 (17.5) | 0.029 |
| At least one previous AP, n (%) | 20 (13) | 7 (14.3) | 0.816 |
| Previous cholecystectomy, n (%) | 9 (5.8) | 15 (30.6) | <0.001 |
| Known cholelithiasis prior to admission, n (%) | 43 (28.1) | 21 (42.9) | 0.053 |
| Biliary sludge in emergency ultrasound, n (%) | 45 (30.6) | 4 (9.1) | 0.004 |
| Cholelithiasis in emergency ultrasound, n (%) | 102 (69.4) | 26 (59.1) | 0.202 |
| Hydropic gallbladder in emergency ultrasound, n (%) | 11 (7.5) | 3 (6.8) | 0.882 |
| CBD dilatation in emergency ultrasound, n (%) | 43 (29.3) | 26 (59.1) | <0.001 |
| CBD dilatation in emergency CT scan, n (%) | 2 (40) | 2 (100) | 0.147 |
| CBD dilatation in hospitalization CT, n (%) | 0 (0) | 0 (0) | – |
| CBD dilatation in MRCP, n (%) | 19 (13.3) | 22 (53.7) | <0.001 |
| CBD dilatation in MRCP (mm)b | 10 (9) | 10 (13) | 0.592 |
| AST in the emergency room (UI/L)b | 227 (338) | 193 (262) | 0.860 |
| ALT in the emergency room (UI/L)b | 191 (362) | 202 (306) | 0.626 |
| Total bilirubin in the emergency room (mmol/L)b | 1.78 (2.89) | 2.06 (1.69) | 0.053 |
| Direct bilirubin in the emergency room (mmol/L)b | 0.47 (2.14) | 1.36 (1.73) | 0.677 |
| GGT in the emergency room (UI/L)b | 230 (422) | 412 (321) | 0.736 |
| APH in the emergency room (UI/L)b | 123 (77) | 166 (226) | 0.226 |
| AST at 72h (UI/L)b | 41.5 (41.3) | 63 (82) | 0.014 |
| ALT at 72h (UI/L)b | 93 (108.8) | 127 (224) | 0.085 |
| GGT at 72h (UI/L)b | 215 (271.5) | 368 (525.5) | 0.005 |
| APH at 72h (UI/L)b | 137.5 (101.7) | 161 (221) | 0.056 |
| Total bilirubin at 72h (mmol/L)b | 0.77 (1.5) | 1.33 (1.8) | 0.008 |
| Direct bilirubin at 72h (mmol/L)b | 0 (0.6) | 0.88 (1.6) | 0.012 |
| Death during hospitalization, n (%) | 0 (0) | 1 (2) | 0.075 |
| Cholangitis during hospitalization, n (%) | 0 (0) | 5 (10.4) | <0.001 |
| Duration of hospitalization (days)b | 6 (6) | 8 (5) | 0.051 |
Values are the number (%) or b the median and interquartile range (Q1–Q3), as indicated.
AP, acute pancreatitis; CBD, common bile duct; CT, computerized tomography; MRI, magnetic resonance imaging; AST; aspartate aminotransferase; ALT, alanine aminotransferase; GGT, gamma glutamyl transpeptidase; APH, alkaline phosphatase; ERCP, endoscopic retrograde cholangiopancreatography.
The multiple linear regression analysis yielded a predictive model of PC (Table 2). The variables selected for this model were: previous episodes of acute pancreatitis, previous cholecystectomy, previous cholelithiasis, dilated CBD in the emergency ultrasound, biliary sludge in the emergency ultrasound, and GGT in the blood analysis performed during hospitalization. Although some studies showed that an elevation of AST increases the probability of choledocholithias, since there are many other factors that affect its levels unrelated to choledocholithiasis, they were not included in the multivariate analysis.
Multiple logistic regression model for predicting persistent choledocholithiasis in patients with acute biliary pancreatitis.
| Variable | Odds ratio (CI 95%) | p-Value |
|---|---|---|
| Previous AP | 0.34 (0.051–1.886) | 0.177 |
| Previous cholecystectomy | 2.343 (0.371–14.461) | 0.614 |
| Previous cholelithiasis | 2.632 (0.545–12.488) | 0.120 |
| CBD dilation in emergency ultrasound | 15.218 (4.32–66.814) | <0.001 |
| Biliary sludge on emergency ultrasound | 0.072 (0.01–0.406) | 0.008 |
| High GGT in blood analysis at 72h | 2.812 (1.368–6.247) | 0.008 |
CI, confidence interval; AP, acute pancreatitis; CBD, common bile duct; GGT, gamma glutamyl transpeptidase.
We evaluated the final model with a ROC analysis, which resulted in an unvalidated ROC-AUC of 0.901. We validated the model with a bootstrap analysis, which resulted in a ROC-AUC of 0.858 (Fig. 2). Based on those findings, we developed a nomogram to calculate the risk of persistent choledocholithiasis with the variables from the model (Fig. 3).
When we used the Youden point as a cutoff value, the model had a sensitivity of 89% and a specificity of 80%, with a PPV of 47% and an NPV of 97%. When we used the top-left point as a cutoff value, the sensitivity was 84%, the specificity was 77%, the PPV was 50%, and the NPV was 95%.
DiscussionABP is an inflammation of the pancreatic gland that can either be self-limiting, or it can lead to the development of local and/or systemic complications, which significantly increase the morbidity and mortality risk.1 The presence or absence of PC in the CBD during an episode of ABP has prognostic implications.8,9 However, the high-technology techniques commonly used to diagnose PC (MRCP, EUS, and ERCP) are costly, not always available, and there is often a delay in performing them. Moreover, this pathology has a high prevalence and entails an enormous health cost.4 Thus, there was a pressing need to develop an alternative predictive model of PC.
In the present study, we developed a model for predicting PC in the CBD for patients with ABP to determine the urgency for subsequent MRCP, EUS, or ERCP. This model could identify patients with a direct indication for ERCP, without the need for a prior MRCP or EUS. Conversely, the model could identify patients that did not require an ERCP, which could reduce costs, reduce the risk to patients, and shorten waiting lists.
Our results showed that patients with PC were more likely to have a dilated CBD, detected on an ultrasound performed in the emergency room, and a lower probability of biliary sludge in the gallbladder. It could be due to the fact that the presence of choledocholithiasis was greater in cholecystectomized patients who therefore do not present biliary sludge in the gallbladder. Moreover, we found that the blood analysis carried out at 72h showed that the levels of AST, total bilirubin, and GGT were significantly higher in patients with choledocholithiasis than in patients without choledocholithiasis. Finally, older age and a history of cholecystectomy were significant factors associated with choledocholithiasis. The final predictive model comprised the following variables: previous acute pancreatitis, previous cholecystectomy, previous cholelithiasis, CBD dilatation on ultrasound, biliary sludge on ultrasound, and GGT in a blood test performed at 72h. The combination of these variables produced a very high ROC-AUC for predicting PC.
Previous studies, such as that by Panda et al.,12 had shown that age, liver biochemical parameter values, and ultrasound findings could predict choledocholithiasis and restrict the use of ERCP to a certain group of patients. The main problem in those studies was that they included patients with acute pancreatitis and patients with choledocholithiasis without acute pancreatitis.12 In contrast, studies that focused only on patients with ABP have shown that elevated liver and pancreatic biochemistry values, measured at 24–48h after symptom onset, could predict PC.9
Although not included in our final predictive model, our bivariate analysis showed a significant association between total bilirubin, measured on day 3 after admission, and the presence of PC. This finding was consistent with some, but not all previous studies. In the first prospective study carried out exclusively in patients with ABP, the best individual predictor of PC was total bilirubin, measured on day 2 (>1.35mg/dl, sensitivity: 90.5%, specificity 63%).15 On the other hand, the clinical practice guidelines of the American Society for Gastrointestinal Endoscopy (in which ABP is included with other biliary pathologies) highlighted that an increase in bilirubin was strongly associated with the presence of choledocholithiasis, and when it was greater than 4mg/dl, it indicated ERCP.9 However, other studies have shown that an isolated increase in bilirubin was a poor predictor of choledocholithiasis.11
As in other studies, the patients with PC in our cohort did not exhibit higher mortality than the group without choledocholithiasis.22,23 However, several previous studies found that patients with PC had higher mortality and complication rates, compared to those without PC.19 The rate of cholangitis during admission was low in our cohort, perhaps due to differences in the etiology of the gallstones. As pointed out by the authors of a study with results similar to ours, pigment stones, which develop infectious complications more frequently, are more typical in Eastern populations.14
PC was detected in 24% of our patients with ABP. These results were consistent with findings in other studies, which reported PC prevalences of around 21%.14 Of note, PC does not necessarily obstruct the flow of bile or pancreatic juice, and it does not necessarily raise liver biochemical markers or cause CBD dilatation9; in particular, when stones are smaller than 5mm, they are typically asymptomatic.24
The timing for performing the analytical tests or liver ultrasound for predicting PC seems to be relevant to the interpretation of results. One study performed early ERCP to detect PC, and demonstrated that liver markers and ultrasound findings obtained in the first hours after diagnosis were not reliable for predicting PC, in part due to local edema of the pancreatic head, secondary to inflammation of the gland.16 In contrast, some studies have used later analytical determinations (4–7th day after admission) for predicting PC; however, later analyses run the risk that spontaneous expulsion of PC might occur before the tests are performed. In our study, the median interval of 72h appeared to avoid these problems; this finding suggested that the appropriate window for obtaining analytical data might be during the 3rd day of hospitalization.11,16
Our study had several limitations. First, its retrospective nature had inherent limitations. Second, the use of a non-invasive technique for detecting PC, such as MRCP, might have reduced the global sensitivity of detecting PC, particularly for detecting small stones (<5mm).25 In our study, the technique used most frequently was MRCP, partly for reasons associated with the characteristics of our hospital. However, several studies have supported the usefulness of MRCP as the non-invasive test of choice and both, EUS and MRCP, are comparable techniques to detect choledocholithiasis and the choice of one or the other depends on the characteristics of the center/patient.26–28 The third limitation was the variability in the time interval before the gold standard technique was performed. Although the intention was to perform the test during hospitalization, in some cases, it was performed on an outpatient basis, due to the availability and organization of the hospital. In those cases, the delay could have led to the spontaneous expulsion of the lithiasis, and thus, the ability to detect choledocholithiasis might have been reduced. The fourth limitation was the unicentric nature of the study; therefore, the conclusions could not be generalized to other populations. Nevertheless, our findings, could be extrapolated to the entire Western Mediterranean area. Last limitation could be that ultrasound scan is often not useful for some body types (especially obesity).
Our study had two main strengths. First, the study population consisted exclusively of patients with ABP. Other investigations that studied trends in liver biochemistry or ultrasound findings included patients with inflammatory biliary diseases (acute pancreatitis, cholecystitis, cholangitis) and non-inflammatory biliary diseases (choledocholithiasis). However, the pathophysiology is different in these entities; thus, in patients with inflammatory diseases, increases observed in liver markers could be due to other causes.14,29,30 Second, our study included a large sample size compared to other similar studies.
In summary, our findings suggested that PC could be predicted in patients admitted with ABP with our model, which included the combination of a history of acute pancreatitis, previous cholecystectomy, previous cholelithiasis, CBD dilation, biliary sludge in the emergency ultrasound, and the blood GGT measured at 72h after admission. To date, very few studies have focused on this condition, which, as stated above, is clinically relevant.
The results of this study, if they are confirmed in prospective studies, may have clinical and economic implications. Our model could be used by clinicians as a simple, inexpensive screening tool for suspicion of PC in patients with ABP. Effective PC screening could lower costs and shorten the delay in performing less accessible imaging tests.31 Moreover, effective screening could obviate the performance of complementary invasive tests (EUS and ERCP) and the associated risks for the patient. However, prospective multicenter studies are needed to validate these results.
Conflict of interestNone declared.