Viral hepatitis is the most important cause of chronic hepatitis worldwide. Stigmatization is defined as a feeling of rejection and isolation of patients by society due to illness. There are no studies on chronic viral hepatitis in the literature in English, which has its own religious and socio-cultural structure. In our study, we aimed to investigate the presence of social stigmatism and psychosocial effects on patients with different stages of chronic viral hepatitis B and C.
MethodsForty-five patients with chronic hepatitis C and 114 patients with chronic hepatitis B were enrolled in the study. Berger's scale was used for stigmatization, composed of 40 four-point Likert items that have four subscales: personalized stigma, disclosure, negative self-image, and public attitude. Stigma score ranges between one and four. Stigma is accepted as present if the overall score is above two.
ResultsOverall the mean stigma scores were 1.97±0.58 and 2.14±0.57 for chronic hepatitis B and C, respectively. There was stigma in 47.4% of the patients with chronic hepatitis B, and 60% of the patients with chronic hepatitis C. Being male was the risk factor on overall stigma, disclosure and public attitude in chronic hepatitis C. Living in an urban setting was the risk factor on negative self-image in chronic hepatitis C and on personalized stigma and disclosure in chronic hepatitis B.
ConclusionsTo the best of our knowledge, this is the first study that provides qualitative information about chronic hepatitis-related stigma. Stigmatization is a major problem in Turkey and worldwide. We believe that increasing the knowledge of the patients and society by teaching about the transmission routes of the disease and focusing on vaccination studies will prevent stigmatization.
La hepatitis viral es la causa más importante de hepatitis crónica en todo el mundo. La estigmatización se define como un sentimiento de rechazo y aislamiento de los pacientes, por parte de la sociedad debido a su enfermedad. No hay estudios sobre la hepatitis viral crónica en la literatura inglesa, que tiene su propia estructura religiosa y sociocultural. En nuestro estudio, nos propusimos investigar la presencia del estigma social y los efectos psicosociales en los pacientes con diferentes fases de hepatitis viral crónica B y C.
MétodosSe incluyó en el estudio a 45 pacientes con hepatitis crónica C y 114 pacientes con hepatitis crónica B. Se utilizó la escala de Berger para la estigmatización, compuesta por 40 ítems Likert de cuatro puntos, con cuatro subescalas cada uno: estigma personalizado, revelación, imagen negativa de sí mismo y actitud pública. La puntuación del estigma oscila entre uno y cuatro. El estigma se acepta como presente si la puntuación general es superior a dos.
ResultadosEn general, la media de las puntuaciones de estigmatización fue de 1,97 ± 0,58 y 2,14 ± 0,57 para la hepatitis crónica B y C, respectivamente. El 47,4% de los pacientes con hepatitis crónica B y el 60% de los pacientes con hepatitis crónica C sufrieron estigmatización. El hecho de ser varón fue el factor de riesgo del estigma general, la revelación y la actitud pública en la hepatitis crónica C. Vivir en un entorno urbano fue el factor de riesgo de la imagen negativa de sí mismo en la hepatitis crónica C y el estigma personalizado y la revelación en la hepatitis crónica B.
ConclusionesHasta donde sabemos, este es el primer estudio que proporciona información cualitativa sobre el estigma relacionado con la hepatitis crónica. La estigmatización es un problema importante en Turquía y en todo el mundo. Creemos que se puede prevenir la estigmatización informando a los pacientes y a la sociedad sobre las vías de transmisión de la enfermedad y centrándonos en los estudios de vacunación.
Viral hepatitis is the most important cause of chronic hepatitis worldwide. These are Hepatitis B virus (HBV), Hepatitis C virus (HCV), and Hepatitis D Virus (HDV). There are approximately 240 million chronic carriers of hepatitis B virus (HBV) surface antigen in the world.1 The estimated prevalence of HBV carriers varies from 0.1% to 15–20% worldwide.2 Turkey is in the intermediate prevalence area for HBV infection, with a prevalence rate of 4%.3 The spectrum of diseases related to HBV infection varies from inactive carriers and chronic HBV, up to hepatocellular carcinoma (HCC), cirrhosis, and death.4 The natural history of HBV infection varies significantly from person to person between different regions. It is also affected by many factors such as age, gender, acute infection age, HBV genotype, host genomics, and HBV mutations.5,6
Besides 100 million people globally have serologic evidence of HCV exposure and 71 million people have chronic HCV infection worldwide,7 the seroprevalence of anti-HCV is 1% in Turkey.3 After encountering with HCV infection, approximately 50–80% of cases develop chronic hepatitis, and 5–30% of them develop cirrhosis over 20–30 years. HCV causes 30% of chronic liver diseases. Due to the high rate of inveteracy, HCV and HBV infections remain a major public health care problem.
The risk of increasing symptoms of depression and anxiety and social stigmatization by the healthcare professionals and the community is quite high in chronic hepatitis patients. Even though psychosocial problems are significantly high in these patients, the issue of how this relationship develops, how it affects each other, how it persists, and how the clinician should be involved in the process has been studied very little.
Stigmatization is defined as a feeling of rejection and isolation of patients by society due to illness. Stigma is a socially constructed experience, the patient has a sense of embracement and insecurity and does not feel integrated or accepted to the culture and society.8,9 Stigma can cause a barrier for talking to others about his/her illness, screening, treatment of these patients, and the effectiveness of public healthcare programs.10 Stigma can disturb the self-esteem, family relations, quality of life, social and economic status of these patients.11
Although this problem is solved to a certain extent in developed societies, it is a very serious problem in developing societies. Not to know the transmission and protection ways of chronic hepatitis in society is a risk factor for stigmatization. As well as the lack of information about illness can lead to a negative self-image.12 Although there are many studies on stigmatism in chronic infectious diseases such as HIV, there are no studies on chronic viral hepatitis, which has its own religious and socio-cultural structure. In our study, we aimed to investigate the presence of social stigmatism and psychosocial effects on patients with different stages of chronic viral hepatitis B and C.
Materials and methodsEthical issueThe study was approved by Bolu Non-Interventional Clinical Research Ethics Committee (Decision Number: 2014/70-164, Date: 29.08.2014). Informed consent was obtained from all of the patients.
Study population and data collectionThe patients with a diagnosis of chronic HBV and chronic HCV who were followed up and treated in our hepatology outpatient clinic were included in the study. Patients under the age of 18 were excluded from the study. Patients diagnosed with or under treatment of any psychological diseases were not included in the study.
The questionnaires were given to the patients with CHC who were under treatment at the period of the study, in the last part of their treatment (especially in the last 4 weeks of treatment) and these patients were identified as CHC treatment group. The carrier group was defined as patients who had previously recovered, did not require treatment, and had a serological status HCV RNA (−) and Anti HCV (+). All medical background and demographic information of the patients were provided from the patients and their files. The study questionnaire was developed based on the Berger stigma scale which is validated for HIV stigma.13 No referral was made to the patients.
Survey instrumentThe questionnaire was translated into Turkish, then English, and then Turkish again by two people who know both languages at a natural speaking level, and the validation was approved by the survey owner. Stigma scale composed of four-point-Likert type 40 items. It has four subscales named personalized stigma, disclosure, negative self-image, and public attitude. Personalized stigma subscale includes; rejection, loss of work, discrimination, and cessation of socialization. Disclosure subscale includes; anxiety and fears about the disease. Negative self-image subscale includes; fear of stigma, concerns about people's attitudes toward those with the disease, beliefs about disease, and guilt. Public attitude subscale includes; the exclusionary behaviors of the society such as dirty and disgusting against patients with hepatitis. Adding each item value and then dividing the total score by the number of items in scale/subscale measured total scores for the scale and subscales. Stigma score ranges between one and four. Stigma was accepted as present if the overall score is above two.
Statistical analysisAll analyses were performed using SPSS version 20.0 (IBM SPSS statistics, version 20.0 for Windows; SPSS, Inc., Chicago, IL, USA, an IBM Company). The consistency of the questionnaire was evaluated with Cronbach-α and values of 0.80 and above were considered reliable. One-way ANOVA and independent student-t-test were used for the continuous variables, and the chi-square (X2) test was used for categorical variables. The effect of demographic features on stigmatization was evaluated by logistic regression analysis. A p-value of <0.05 was accepted as statistically significant.
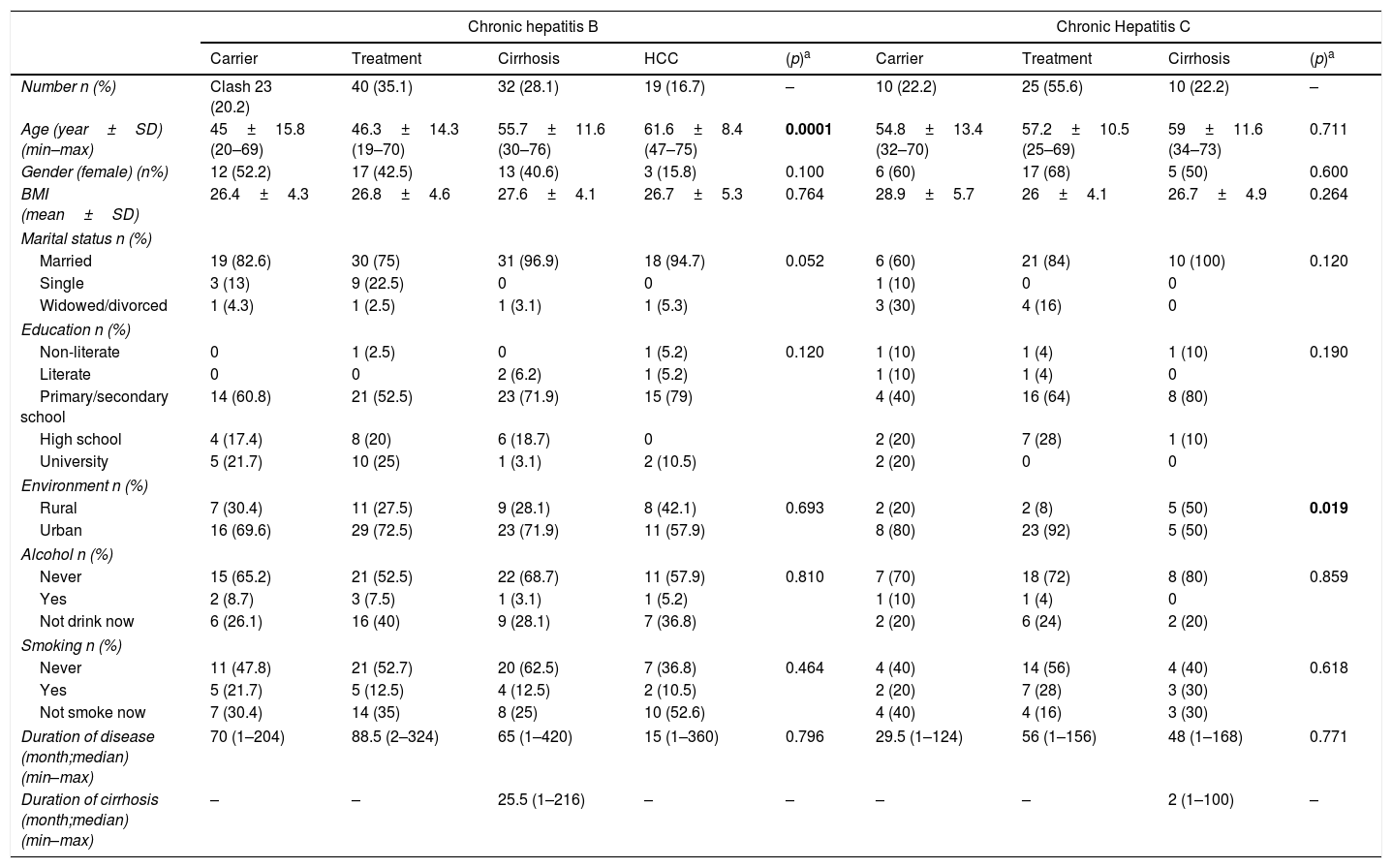
ResultsA total of 166 patients responded to be included in the study. During the study period, four patients gave up participating in the study and three patients could not answer the questions since their educational level was not sufficient to understand and answer the questionnaire. In a total of 159 chronic hepatitis patients were included in the study. The mean ages of patients were 51.2 and 57.0 in the groups of HBV and HCV, respectively. In patients with HBV, cirrhosis was seen as more common in elder patients (p=0.0001). 39.5% of HBV patients and 62.2% of HCV patients were female. The demographic features of the patients are detailed in Table 1.
Socio-demographic and clinical characteristics of the patients with chronic hepatitis B and C.
| Chronic hepatitis B | Chronic Hepatitis C | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Carrier | Treatment | Cirrhosis | HCC | (p)a | Carrier | Treatment | Cirrhosis | (p)a | |
| Number n (%) | Clash 23 (20.2) | 40 (35.1) | 32 (28.1) | 19 (16.7) | – | 10 (22.2) | 25 (55.6) | 10 (22.2) | – |
| Age (year±SD) (min–max) | 45±15.8 (20–69) | 46.3±14.3 (19–70) | 55.7±11.6 (30–76) | 61.6±8.4 (47–75) | 0.0001 | 54.8±13.4 (32–70) | 57.2±10.5 (25–69) | 59±11.6 (34–73) | 0.711 |
| Gender (female) (n%) | 12 (52.2) | 17 (42.5) | 13 (40.6) | 3 (15.8) | 0.100 | 6 (60) | 17 (68) | 5 (50) | 0.600 |
| BMI (mean±SD) | 26.4±4.3 | 26.8±4.6 | 27.6±4.1 | 26.7±5.3 | 0.764 | 28.9±5.7 | 26±4.1 | 26.7±4.9 | 0.264 |
| Marital status n (%) | |||||||||
| Married | 19 (82.6) | 30 (75) | 31 (96.9) | 18 (94.7) | 0.052 | 6 (60) | 21 (84) | 10 (100) | 0.120 |
| Single | 3 (13) | 9 (22.5) | 0 | 0 | 1 (10) | 0 | 0 | ||
| Widowed/divorced | 1 (4.3) | 1 (2.5) | 1 (3.1) | 1 (5.3) | 3 (30) | 4 (16) | 0 | ||
| Education n (%) | |||||||||
| Non-literate | 0 | 1 (2.5) | 0 | 1 (5.2) | 0.120 | 1 (10) | 1 (4) | 1 (10) | 0.190 |
| Literate | 0 | 0 | 2 (6.2) | 1 (5.2) | 1 (10) | 1 (4) | 0 | ||
| Primary/secondary school | 14 (60.8) | 21 (52.5) | 23 (71.9) | 15 (79) | 4 (40) | 16 (64) | 8 (80) | ||
| High school | 4 (17.4) | 8 (20) | 6 (18.7) | 0 | 2 (20) | 7 (28) | 1 (10) | ||
| University | 5 (21.7) | 10 (25) | 1 (3.1) | 2 (10.5) | 2 (20) | 0 | 0 | ||
| Environment n (%) | |||||||||
| Rural | 7 (30.4) | 11 (27.5) | 9 (28.1) | 8 (42.1) | 0.693 | 2 (20) | 2 (8) | 5 (50) | 0.019 |
| Urban | 16 (69.6) | 29 (72.5) | 23 (71.9) | 11 (57.9) | 8 (80) | 23 (92) | 5 (50) | ||
| Alcohol n (%) | |||||||||
| Never | 15 (65.2) | 21 (52.5) | 22 (68.7) | 11 (57.9) | 0.810 | 7 (70) | 18 (72) | 8 (80) | 0.859 |
| Yes | 2 (8.7) | 3 (7.5) | 1 (3.1) | 1 (5.2) | 1 (10) | 1 (4) | 0 | ||
| Not drink now | 6 (26.1) | 16 (40) | 9 (28.1) | 7 (36.8) | 2 (20) | 6 (24) | 2 (20) | ||
| Smoking n (%) | |||||||||
| Never | 11 (47.8) | 21 (52.7) | 20 (62.5) | 7 (36.8) | 0.464 | 4 (40) | 14 (56) | 4 (40) | 0.618 |
| Yes | 5 (21.7) | 5 (12.5) | 4 (12.5) | 2 (10.5) | 2 (20) | 7 (28) | 3 (30) | ||
| Not smoke now | 7 (30.4) | 14 (35) | 8 (25) | 10 (52.6) | 4 (40) | 4 (16) | 3 (30) | ||
| Duration of disease (month;median)(min–max) | 70 (1–204) | 88.5 (2–324) | 65 (1–420) | 15 (1–360) | 0.796 | 29.5 (1–124) | 56 (1–156) | 48 (1–168) | 0.771 |
| Duration of cirrhosis (month;median)(min–max) | – | – | 25.5 (1–216) | – | – | – | – | 2 (1–100) | – |
SD: Standard deviation, HCC: Hepatocellular carcinoma, BMI: Body mass index.
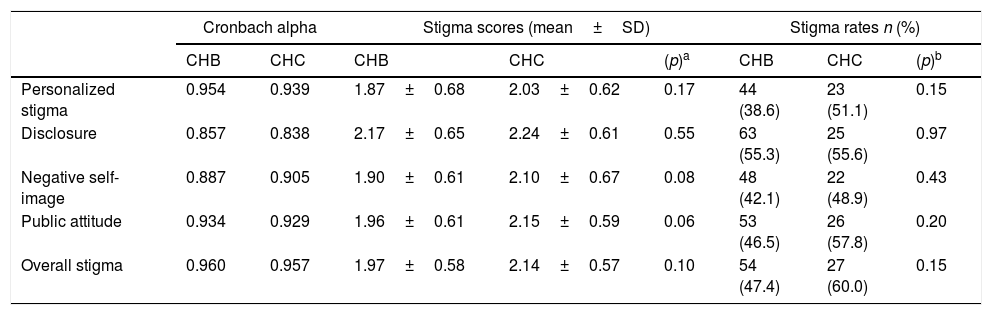
In the internal consistency analysis of the stigma scale, Cronbach's alpha values were 0.95 for chronic hepatitis C and 0.96 for chronic hepatitis B. Overall mean stigma scores were 1.97±0.58 and 2.14±0.57 for chronic hepatitis B and C, respectively (p=0.10). There were stigmas in 47.4% of patients with chronic hepatitis B, 60% of the patients with chronic hepatitis C (p=0.15). Stigma scores according to stigma subscales are shown in Table 2.
The comparison of the stigma rates and scores in the chronic hepatitis B and C patients.
| Cronbach alpha | Stigma scores (mean±SD) | Stigma rates n (%) | ||||||
|---|---|---|---|---|---|---|---|---|
| CHB | CHC | CHB | CHC | (p)a | CHB | CHC | (p)b | |
| Personalized stigma | 0.954 | 0.939 | 1.87±0.68 | 2.03±0.62 | 0.17 | 44 (38.6) | 23 (51.1) | 0.15 |
| Disclosure | 0.857 | 0.838 | 2.17±0.65 | 2.24±0.61 | 0.55 | 63 (55.3) | 25 (55.6) | 0.97 |
| Negative self-image | 0.887 | 0.905 | 1.90±0.61 | 2.10±0.67 | 0.08 | 48 (42.1) | 22 (48.9) | 0.43 |
| Public attitude | 0.934 | 0.929 | 1.96±0.61 | 2.15±0.59 | 0.06 | 53 (46.5) | 26 (57.8) | 0.20 |
| Overall stigma | 0.960 | 0.957 | 1.97±0.58 | 2.14±0.57 | 0.10 | 54 (47.4) | 27 (60.0) | 0.15 |
SD: standard deviation, CHB: chronic hepatitis B, CHC: chronic hepatitis C.
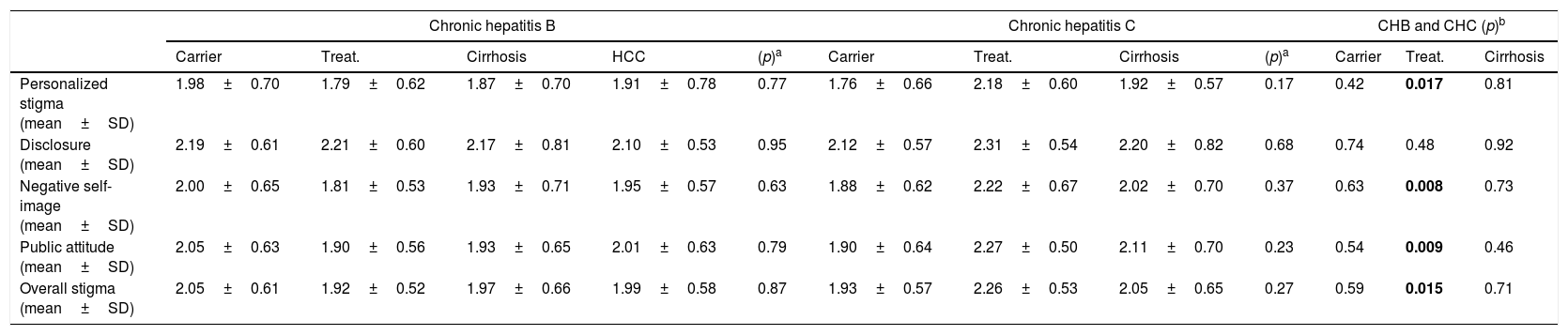
Although stigma was higher in the inactive carrier group of chronic hepatitis B and in the treatment and cirrhosis groups of chronic hepatitis C, there was no significant association among the different stages of both diseases (p=0.87 and p=0.27, respectively). The scores of the same stages of both diseases were compared with each other. Although in the inactive carrier groups of both diseases, the stigma of the patients with chronic hepatitis B was higher (p=0.59), and in the cirrhosis groups, the stigma of the patients with chronic hepatitis C was higher (p=0.71), there were no significant associations in the inactive carrier groups and cirrhosis groups. In the treatment groups, stigma was significantly higher in chronic hepatitis C at an overall stigma scale (p:0.015) and all subscales except for disclosure (Table 3). Also, stigma rates compared between different stages of disease in patients with HBV and HCV separately, and between the same stages of both diseases (Table 4).
The comparison of the stigma scores between same stages of both diseases, and among different stages of one disease in chronic hepatitis B and C.
| Chronic hepatitis B | Chronic hepatitis C | CHB and CHC (p)b | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Carrier | Treat. | Cirrhosis | HCC | (p)a | Carrier | Treat. | Cirrhosis | (p)a | Carrier | Treat. | Cirrhosis | |
| Personalized stigma (mean±SD) | 1.98±0.70 | 1.79±0.62 | 1.87±0.70 | 1.91±0.78 | 0.77 | 1.76±0.66 | 2.18±0.60 | 1.92±0.57 | 0.17 | 0.42 | 0.017 | 0.81 |
| Disclosure (mean±SD) | 2.19±0.61 | 2.21±0.60 | 2.17±0.81 | 2.10±0.53 | 0.95 | 2.12±0.57 | 2.31±0.54 | 2.20±0.82 | 0.68 | 0.74 | 0.48 | 0.92 |
| Negative self-image (mean±SD) | 2.00±0.65 | 1.81±0.53 | 1.93±0.71 | 1.95±0.57 | 0.63 | 1.88±0.62 | 2.22±0.67 | 2.02±0.70 | 0.37 | 0.63 | 0.008 | 0.73 |
| Public attitude (mean±SD) | 2.05±0.63 | 1.90±0.56 | 1.93±0.65 | 2.01±0.63 | 0.79 | 1.90±0.64 | 2.27±0.50 | 2.11±0.70 | 0.23 | 0.54 | 0.009 | 0.46 |
| Overall stigma (mean±SD) | 2.05±0.61 | 1.92±0.52 | 1.97±0.66 | 1.99±0.58 | 0.87 | 1.93±0.57 | 2.26±0.53 | 2.05±0.65 | 0.27 | 0.59 | 0.015 | 0.71 |
SD: Standard deviation, CHB: Chronic hepatitis B, CHC: Chronic hepatitis C, HCC: Hepatocellular carcinoma, Treat: Treatment.
The comparison of the stigma rates between same stages of both diseases, and among different stages of one disease in chronic hepatitis B and C.
| Chronic hepatitis B n (%) | Chronic hepatitis C n (%) | CHB and CHC (p)b | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Carrier | Treat. | Cirrhosis | HCC | (p)a | Carrier | Treat. | Cirrhosis | (p)a | Carrier | Treat. | Cirrhosis | |
| Personalized stigma | 9 (39.1) | 13 (32.5) | 15 (46.8) | 7 (36.8) | 0.66 | 4 (40) | 15 (60) | 4 (40) | 0.41 | 0.96 | 0.029 | 0.70 |
| Disclosure | 13 (56.5) | 23 (57.5) | 16 (50) | 11 (57.9) | 0.92 | 4 (40) | 17 (68) | 4 (40) | 0.17 | 0.38 | 0.400 | 0.58 |
| Negative self-image | 13 (56.5) | 12 (30) | 14 (43.7) | 9 (47.3) | 0.20 | 4 (40) | 14 (56) | 4 (40) | 0.57 | 0.38 | 0.037 | 0.83 |
| Public attitude | 12 (52.2) | 14 (35) | 17 (53.1) | 10 (52.7) | 0.35 | 4 (40) | 17 (68) | 5 (50) | 0.27 | 0.52 | 0.010 | 0.86 |
| Overall stigma | 13 (56.5) | 17 (42.5) | 16 (50) | 8 (42.1) | 0.69 | 4 (40) | 17 (68) | 6 (60) | 0.31 | 0.38 | 0.045 | 0.58 |
CHB: Chronic hepatitis B, CHC: Chronic hepatitis C, HCC: Hepatocellular carcinoma, Treat: Treatment.
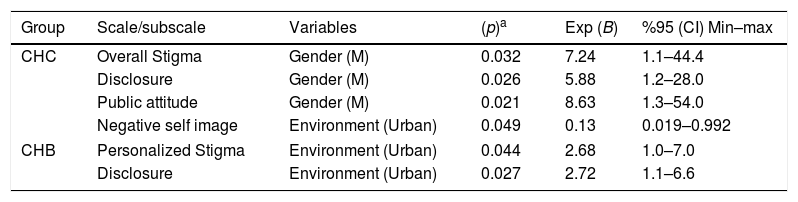
The effects of gender, age, marital status, education, and environment on stigma were evaluated with multivariate logistic regression analysis. Being male was the risk factor on overall stigma, disclosure, and public attitude in chronic hepatitis C (p=0.03 OR: 7.3, p=0.026 OR: 5.9, p=0.02 OR: 8.6, respectively). Living in the urban area was the risk factor on negative self-image in chronic hepatitis C (p=0.049 OR: 0.14), on personalized stigma and disclosure in the chronic hepatitis B (p=0.04 OR: 2.7, p=0.02 OR: 2.7, respectively) (Table 5).
Associated factors with stigmatization and subscales.
| Group | Scale/subscale | Variables | (p)a | Exp (B) | %95 (CI) Min–max |
|---|---|---|---|---|---|
| CHC | Overall Stigma | Gender (M) | 0.032 | 7.24 | 1.1–44.4 |
| Disclosure | Gender (M) | 0.026 | 5.88 | 1.2–28.0 | |
| Public attitude | Gender (M) | 0.021 | 8.63 | 1.3–54.0 | |
| Negative self image | Environment (Urban) | 0.049 | 0.13 | 0.019–0.992 | |
| CHB | Personalized Stigma | Environment (Urban) | 0.044 | 2.68 | 1.0–7.0 |
| Disclosure | Environment (Urban) | 0.027 | 2.72 | 1.1–6.6 | |
CHB: Chronic hepatitis B, CHC: Chronic hepatitis C, M: Male.
This study provides qualitative information about chronic hepatitis-related stigma in a group of patients in the Turkish population. Approximately half of the patients with HBV had a total stigma, while this rate was slightly higher in patients with HCV; this is not statistically significant (p>0.05). In a study conducted in Vietnam with patients with HBV, a 48.5% stigma was observed in patients.12 In one study, stigma rates in patients with HIV ranged from 4.9% to 94.4%. In countries with a higher number of patients living with HIV/AIDS, stigma rates were lower.14 This explains the negative association between HIV knowledge and stigma rates.15 The greater the number of people suffering from the disease in the society in all of the infectious diseases associated with stigma, the higher the knowledge level of the society, and the stigmatization rates decrease such as leprosy,16 and HCV.17 Despite the low level of personalized stigma rates, HBV patients felt high levels of anxiety and fears about disclosure. This shows that when they are exposed, they think they won’t be well thought about by society. Therefore, it is important to educate society and patients about the disease and to increase their knowledge. While improving knowledge about HBV leads a better attitude toward HBV patients in a study conducted in Japan, it has been shown that increasing the knowledge in society may lead to higher stigma in a study conducted in Vietnam.18,19 This shows that knowledge can have different effects on understanding the disease in different societies.
Similarly, personalized stigma was seen at the lowest rate in the group of HCV, while the stigma associated with public attitude was the highest. Since HCV transmission routes are not well known by society and connected to only sexual transmission and intravenous drug use leads to some qualifications like disgusting and dirty against these patients. The stigmatization against HCV patients is degrading and powerful, silences and marginalizes the patients, and poisoning their social life.20
When diseases are evaluated at the group level, the treatment and cirrhosis groups of HCV and the inactive carrier group of HBV were having high stigmatism. Although there is no significant difference between the stages of the disease in terms of stigma, hepatitis B carriers and hepatitis C patients those under treatment experience higher stigmatism. This may be due to the low chance of getting rid of the disease in hepatitis B patients and for the inactive carrier patients knowing that they will carry this disease for life. In hepatitis C, this may be due to the serious side effects of the treatment and the absence of alternative therapies in case of unresponsiveness.
We revealed that being a male is a risk factor up to 7–8 times in general stigma, disclosure, and public attitude in our HCV patients. This may depend on the role of men, being extrovert and providing earning, in Turkish society and family. Male is an extroverted member of the family, especially in less developed and patriarchal societies. This stigmatization may also depend on the instinct to protect the patient's self and the family from society. In studies with HIV patients, although stigmatization appears to negatively affect a person's self-esteem, this is less common in patients with chronic hepatitis as in our study.21,22
Living in the urban area plays a protective role in the negative-self image in patients with hepatitis C (p=0.049 OR: 0.14), it may be due to the city being more crowded and the patient feeling more free there. On the contrary, living in the urban area in patients with hepatitis B is a risk factor for stigmatism (personalized stigma and disclosure (p=0.04 OR: 2.7, p=0.02 OR: 2.7, respectively)). This difference may be related to the level of knowledge about the disease, the effect of the disease on the mood of the individual, and the belief and sociocultural structure of Turkish society.
Stigmatization prevents patients’ diagnosis of disease, efforts to seek solutions, and their compliance with the treatment, and affects public health, psychology, and general well-being of the patients. A multidisciplinary approach with informing the patient correctly and the organization of socio-psychological support programs in chronic viral hepatitis will not only increase the success of the treatment but also bring back the individuals to the society. As stated in a review, it is necessary to determine the main cause of stigmatization and to terminate the mistrust for the treatment of HCV patients. Developing genuine partnerships with HCV patients, consulting on the design and operation of the health service, and reshaping the health service is important for the treatment of these patients.23
There are some limitations of our study. This study conducted in only a region and does not reflect the whole of Turkey. It is also a limitation that the therapies given to hepatitis C patients were not recorded. Changing the course of hepatitis C disease with new treatments would also cause positive changes in patients’ stigmatization.
In conclusion, this is the first study that provides qualitative information about chronic viral hepatitis-related stigma in Turkey. We believe that, to increase the knowledge of the patients and society by teaching the transmission routes of the disease and to focus on vaccination studies would prevent the stigmatization.
Conflict of interestsThe authors declare that they have no conflict of interest.