Pancreatic cysts have a large differential diagnosis including neoplastic and nonneoplastic lesions. Serous cystadenoma (SCA) comprises 10–15% of cystic lesions and 1–2% of pancreatic neoplasms.1,2 They are composed by several cysts lined by cells with eosinophilic cytoplasm, occur more commonly in mid-age women and are usually benign. Solid serous cystadenoma (SSCA) is a rare variant that usually presents as a solid pancreatic nodule leading to difficult assessment and common preoperative misdiagnosis with malignant neoplasia.2 The authors describe two cases of SSCA that underwent diagnostic sampling through endoscopic ultrasound fine needle aspiration/biopsy (EUS-FNA/FNB) performed by the same operator (Fig. 1).
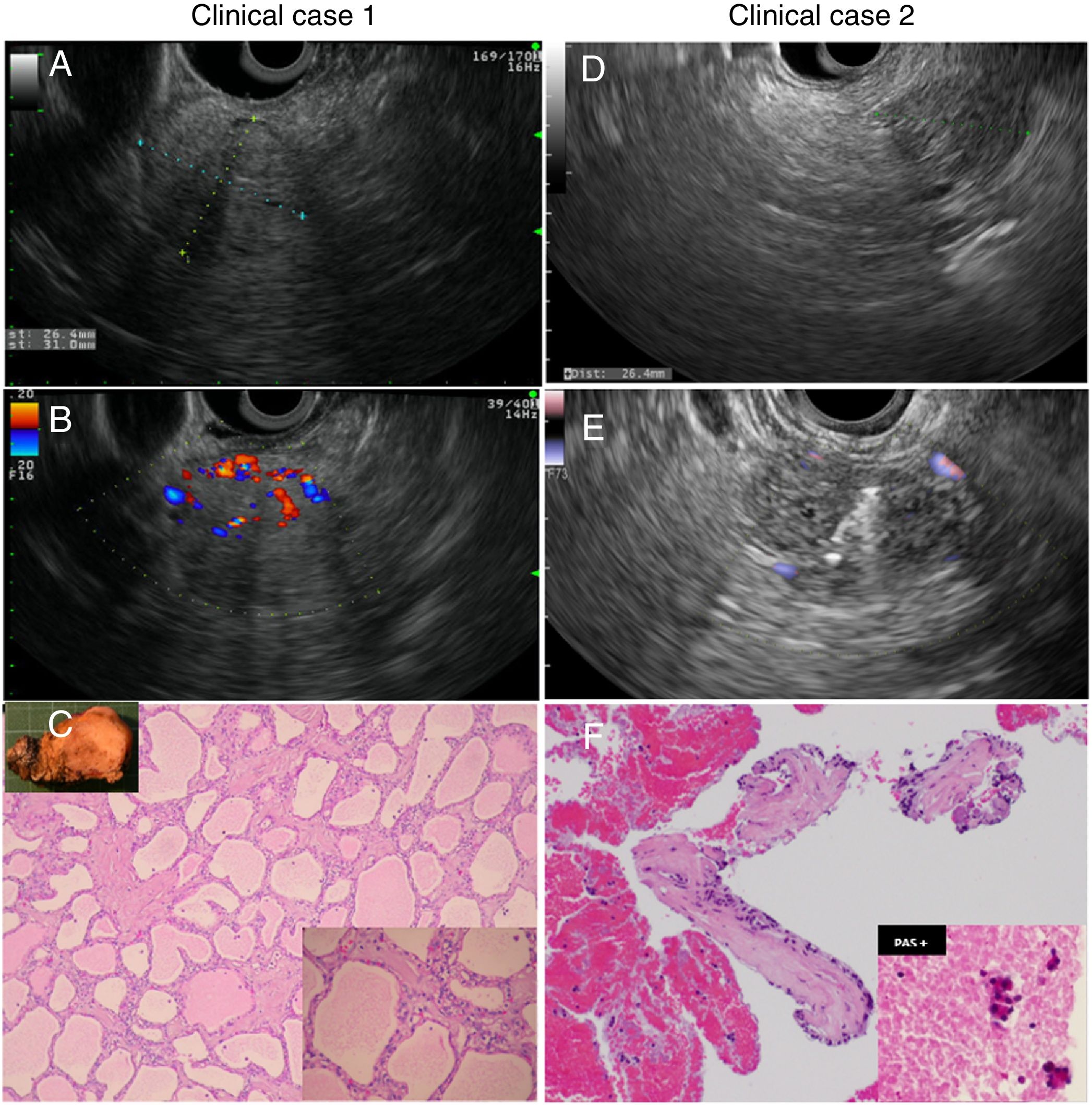
Iconographic features of both clinical cases. (A and B) EUS showing the pancreatic solid head mass with positive Doppler flow in case 1. (C) Surgical pathology after resection which confirms the diagnosis of SSCA. (D and E) EUS showing the pancreatic solid head mass before and during FNB in case 2. (F) Cellblock confirming the diagnosis of SSCA in case 2.
A 44-year-old woman underwent an abdominal ultrasound for dyspeptic symptoms after a normal esophagogastroduodenoscopy. A pancreatic solid head mass was noted and the compute tomography (CT) showed a 3cm solid lesion with mild contrast enhancement. Serum CA 19.9 and chromogranin A were normal and the somatostatin receptor scintigraphy was negative. EUS showed a 2.5×3.0cm well circumscribed isoechoic pancreatic solid head mass with positive Doppler flow and no cystic spaces. No evidence for vascular invasion was observed. FNA was performed using an Olympus® 22 gauge needle (6 passes, 5cc negative pressure) but cytology was non diagnostic. The patient underwent a pylorus preserving pancreatoduodenectomy. Gross pathology of the resected specimen demonstrated a 2cm, well demarcated, encapsulated solid mass. Light microscopy showed a tumor composed of tubules, formed by cuboidal cells with clear cytoplasm and round nuclei, surrounded by bands of fibrous tissue. No pleomorphism, necrosis or mitotic activity was identified. Although small acini with glandular spaces were present within the nests, cystic spaces were absent. Tumor cells were reactive for PAS, CA19.9 and CKCAM 5.2, being negative for CEA, MelanA and epithelial membrane antigen. These findings were suggestive of SSCA. After 8 months the patient was fully recovered although started on insulin therapy. Clinical surveillance was maintained with good clinical outcome.
Clinical case 2A 60-year-old woman was referred due to persistent unspecific abdominal pain and underwent a CT that revealed a 3cm solid hypervascular pancreatic lesion. Serum CA 19.9, CEA and chromogranin A were normal. EUS was performed showing a 2×3cm well-defined isoechoic mass in the pancreatic head with few diminutive cystic areas, positive Doppler flow and no wirsung dilation or vascular invasion. FNB using an Acquire™ 22 gauge franseen type histology needle (transgastric, 3 passes) was accomplished. Cytopathology revealed a short tissue fragment with small cuboid PAS positive cells lining a hyaline stroma without chromogranin or synaptophysin expression. Although no further immunohistochemistry (IHC) markers could be performed given the low cellularity of the sample, the combination of EUS and cytological features were consistent with the diagnosis of SSCA. The patient maintained clinical surveillance with good clinical outcome. No additional intervention was performed.
Pancreatic SCA is a neoplastic lesion composed by cuboidal cells arising from the pancreatic ductal epithelium with glycogen-rich cytoplasm and small central nuclei. SCA can be classified into 4 morphologic patterns: microcystic (which comprises more than half of the cases), macrocystic (30%), mixed (11%), and solid variant resulting from the coalescence of multiple 1–2-mm cysts (7%).3
SSCA, first described in 1996, is an extremely rare condition with approximately 24 cases reported in literature.2,4 The cytological and architectural features are similar to the other subtypes of SCA but it lacks the fluid filled cysts, potentially due to absence of cell secretory capacity. The differential diagnosis includes other solid pancreatic neoplasms namely neuroendocrine tumors, solid pseudopapillary tumor, ductal adenocarcinoma, acinar cell carcinoma and pancreatic metastasis. IHC analysis may help to differentiate SSCA from these lesions as expression of the common SCA markers like PAS and low-molecular weight cytokeratins is typical. Furthermore, absence of chromogranin and synaptophysin expression usually rules out a neuroendocrine origin.4,5
SSCA are often asymptomatic and mostly present as an incidental finding on cross sectional imaging studies. Although EUS-FNA/FNB plays a well-established role in the assessment of pancreatic cystic lesions, it was rarely applied in patients with SSCA, and in most cases it was non-diagnostic. Elastography and contrast-enhanced EUS can also contribute for the differential diagnosis in selected patients.2–5 The authors report two cases that exemplify the diagnostic challenge of pancreatic SSCA and the potential role of EUS-FNA/FNB, describing one of the few reports of successful preoperative cytopathological diagnosis using this technique.
Financial supportNot applicable.
Conflicts of interestThere are no financial or other conflicts of interest regarding this article.
There are no acknowledgements to perform.