A 73 years old female patient, with multiple co-morbidities (bedridden, dementia, hypertension, diabetes mellitus, cardiac insufficiency, previous stroke), presented in a Gastroenterology department with mild abdominal pain and distended abdomen.
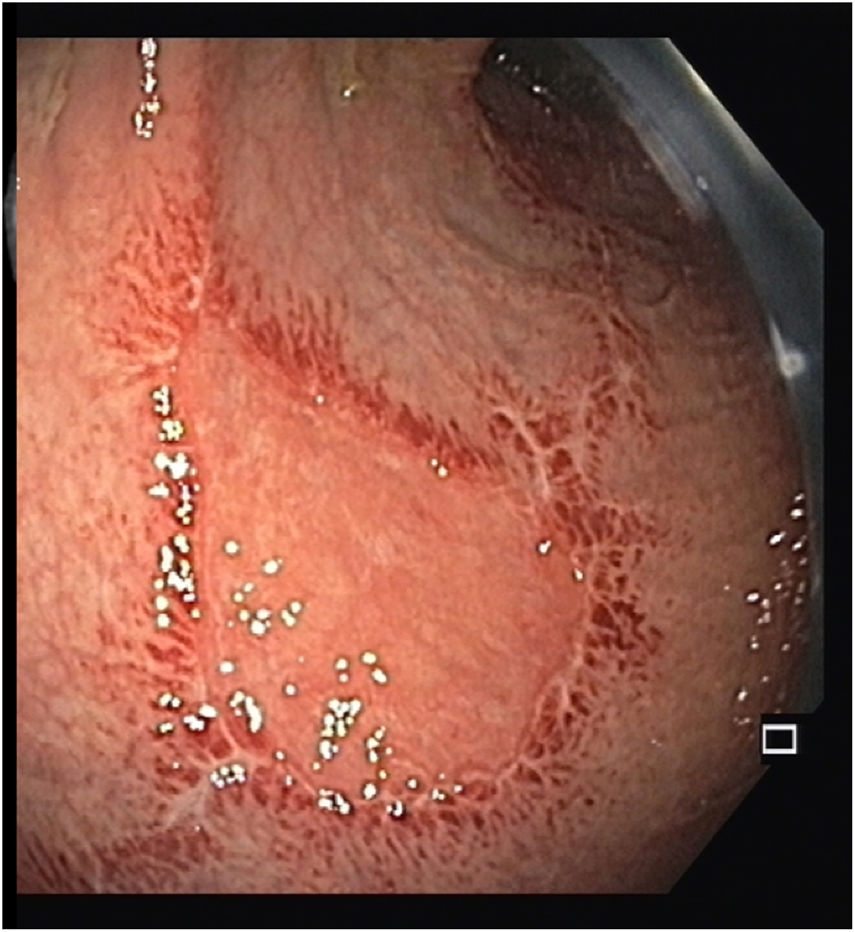
Other than abdominal distension, physical examination was normal showing normal vital signs and no skin lesions. Laboratory tests did not show significant findings. The patient performed a plain abdominal film that showed megacolon and a computed tomography scan that revealed marked distension of the sigmoid colon and rectum without any identified anatomic lesion, compatible with pseudo-obstruction (Fig. 1). A sigmoidoscopy with enema preparation was performed revealing 2 triangular-shaped ulcers with approximately 20mm (Fig. 2). Histopathological analysis showed edema, vascular congestion and lymphoplasmocytic infiltrate of the chorion with fibrin-leukocyte exudate and granulation tissue. The results of PCR testing were positive for varicella-zoster virus (VZV).
Patient started on acyclovir with clinical improvement and resolution of the lesions on follow-up sigmoidoscopy.
VZV-induced Ogilvie's syndrome is a rare condition that usually occurs in immunocompromised patients and in association with skin lesions.1–3 However, these lesions may appear several days/weeks before or after colonic involvement, which may have led to their non-identification in a bedridden patient with dementia.
In conclusion, despite the rarity of VZV-induced Ogilvie's syndrome, it should be included in the differential diagnosis even in immunocompetent patients with no skin lesions on the time of the diagnosis.
Informed consentAn informed patient consent was obtained for publication of the case details.
FundingNo financial support.
Conflicts of interestThe authors declare no conflict of interest.