The rate of non-adherence to medical treatment in inflammatory bowel disease (IBD) is around 50%, with the consequent negative impact on treatment results, morbidity and cost.
ObjectivesTo determine through an online survey among gastroenterologists with special dedication to IBD, their knowledge about the adherence to treatment of their patients and the methods used to improve it.
MethodsAn email was sent to gastroenterologists from the technical office of the Crohn's disease and ulcerative colitis Spanish working group (GETECCU), with a link to the online survey.
Results760 physicians were invited. One hundred eighty-four surveys were obtained (28.5%). A total of 68% of respondents had indexed IBD publications, 13% of which were on adherence. Although almost 99% considered adherence as very important/important, 25% of physicians did not assess it. Even though 100% considered that improving adherence would imply a better prognosis, 47% did not use any system to improve it. The factors associated with the assessment and improvement of adherence were: university hospital (81.4%), combined treatment with thiopurines and biological drugs (44.6%), physician gender (female) (63.1%), dedicating ≥6h weekly to IBD (71.6%), previous published indexed papers on IBD (68.5%) and on adherence in IBD (12.5%), and considering adherence as important/very important (98.9%).
ConclusionsAlthough knowledge about the relevance of adherence to medical treatment in IBD is widespread, among the gastroenterologists with special dedication to IBD who were surveyed, almost half do not use any objective system to quantify it. An effort must be made to quantify and improve adherence to the treatment of these patients.
La tasa de no adherencia al tratamiento médico en la enfermedad inflamatoria intestinal (EII) está en torno al 50%, empeorando así los resultados de los tratamientos, la morbilidad y el coste.
ObjetivosDeterminar mediante una encuesta online entre gastroenterólogos con especial dedicación a la EII el conocimiento sobre la adherencia al tratamiento de sus pacientes y los métodos utilizados para mejorarla.
MétodosDesde la secretaría técnica de GETECCU se envió un correo a los socios con un enlace a la encuesta a través de un sistema online.
ResultadosSe invitó a 760 socios. Se obtuvieron 184 encuestas (28,5%). El 68% de los encuestados tenía publicaciones sobre EII indexadas, solo el 13% eran sobre adherencia. A pesar de que casi el 99% consideraban la adherencia como muy importante/importante, el 25% de los médicos no la medía. Pese a que el 100% consideraba que mejorar la adherencia implicaría un mejor pronóstico, el 47% no utilizaba sistemas para mejorarla. Los factores asociados con la medición y mejora de la adherencia fueron: hospital universitario (81,4%), que el paciente recibiera tratamiento combinado con tiopurínicos y biológicos (44,6%), médico de sexo femenino (63,1%), dedicar≥6h semanalmente a la EII (71,6%), que el médico tenga publicaciones indexadas sobre EII (68,5%) y sobre adherencia en EII (12,5%) y que el médico considere la adherencia importante o muy importante (98,9%).
ConclusionesAunque el conocimiento sobre la relevancia de la adherencia al tratamiento médico en EII está generalizado, entre los gastroenterólogos con dedicación especial a la EII que fueron encuestados casi la mitad no utiliza ningún sistema objetivo para cuantificarla. Se debe hacer un esfuerzo para cuantificar y mejorar la adherencia al tratamiento de estos pacientes.
Adherence to treatment is defined as the following of medical recommendations by patients. This not only includes taking the prescribed medication at the recommended doses and intervals, but also attending scheduled appointments and/or tests and following advice on lifestyle and diet. Non-adherence can affect the effectiveness of the treatment and worsen the course of the disease, with significant clinical consequences. Good adherence has to be a priority in the treatment of any disease.1 Inflammatory bowel disease (IBD) is a worldwide health problem whose incidence is on the increase in many countries.2 Due to its chronic nature, IBD requires lifelong treatment and follow-up. In view of its high incidence, this means a significant cost for healthcare systems and, among gastrointestinal diseases, IBD is currently one of those commanding the highest level of expenditure.3 In chronic diseases like IBD with few or no symptoms in the periods of remission, patients are more likely to have poor adherence to medical treatment.4,5
It has been suggested that a successful strategy for improving adherence might have greater health benefits than advances in the current treatments.6 Any new drug that improves efficacy would be an advance over the drugs already available, but we forget that lack of adherence to treatment is a serious problem which limits the effectiveness of the current options.
Studies have demonstrated that good adherence to treatment improves the prognosis of the disease.7–9 However, IBD is high-risk for poor adherence. This affected by the fact that IBD is a group of chronic disorders, often affecting young patients, with an unpredictable course, with sometimes prolonged remission periods, and that the treatments involve side effects and forms of administration poorly accepted by some patients.10–12
Different studies have estimated the rate of non-adherence to medical treatment in IBD to be around 30–40%.12 Poor adherence in IBD is associated with increased disease activity and higher relapse and morbidity and mortality rates, not to mention increasing healthcare costs and worsening patients’ quality of life.9,13,14
Therefore, any action that increases adherence would mean an improvement in the quality of care provided to patients with IBD and would improve their prognosis. Various attempts have been made to try to determine the predictors of poor adherence and design interventions to improve it. However, these strategies have always been directed at the patient to identify those at risk,10,15,16 with the aim of applying specific measures which, theoretically, would improve adherence.17–19
Very few studies has been done on doctors’ perceptions of this problem and how it is managed in routine clinical practice. Only a few publications have looked at whether or not doctors are measuring adherence and none have analysed what they are doing to improve adherence among their patients.20,21
With this premise, we designed an online survey to determine the extent of knowledge among Spanish gastroenterologists about treatment adherence in their patients with IBD and what methods they were using in routine clinical practice to improve it.
MethodsWe designed a questionnaire for gastroenterologists. The questionnaire was anonymous, with no address, principal investigator or any other identification system. It included two types of items, demographic and related to work experience (Appendix B) and others specifically aimed at determining the doctor's attitude towards adherence (Appendix B). In November 2017, an email was sent from the Technical Secretariat of the Grupo Español de Trabajo en Enfermedad de Crohn y Colitis Ulcerosa (GETECCU) [Spanish Working Group on Crohn's Disease and Ulcerative Colitis] to members with a link to an online survey with said questionnaire, inviting them to take part in the study. The survey, responses and data were recorded through the Survey Monkey online survey system (Menlo Park, CA, USA) (https://www.surveymonkey.com/home). Survey Monkey is an online survey platform. Using this platform, the results can be obtained as databases and exported to statistical spreadsheets. A response time of two months was given, with a second survey sent in January 2018 to those who had not responded and a third in March 2018. In April 2018, the period to answer the questionnaires was considered closed. Unanswered surveys and those in which not all questions were completed were discarded from the analysis.
Statistical analysisThe results of the qualitative variables were expressed as frequencies and percentages. We used the Chi-square test to analyse the factors, both of the doctor and the patient, related to measuring adherence to treatment in the clinic and those related to using a system to improve adherence. These factors included gender and age of the doctor, type of hospital they were working at (university or not), whether or not they ran a specific IBD clinic, length of time practising in the specialist area, the mean number of IBD patients they saw weekly, weekly time dedicated to IBD, whether or not they saw patients on the wards with IBD, performed endoscopies on patients with IBD, had published work on IBD or on adherence in IBD indexed in Medline or were concerned about their patients’ adherence to treatment, and how important they considered it to be, whether or not they measured their patients’ adherence in the clinic and whether the severity of the disease influenced whether or not they did so and, finally, whether they measured adherence according to the treatment received and in which cases. A value of p<0.05 was considered significant. Statistical analyses were performed with the SPSS statistical package (IBM Corp. Released 2017. IBM SPSS Statistics for Windows, Version 25.0. Armonk, NY, USA).
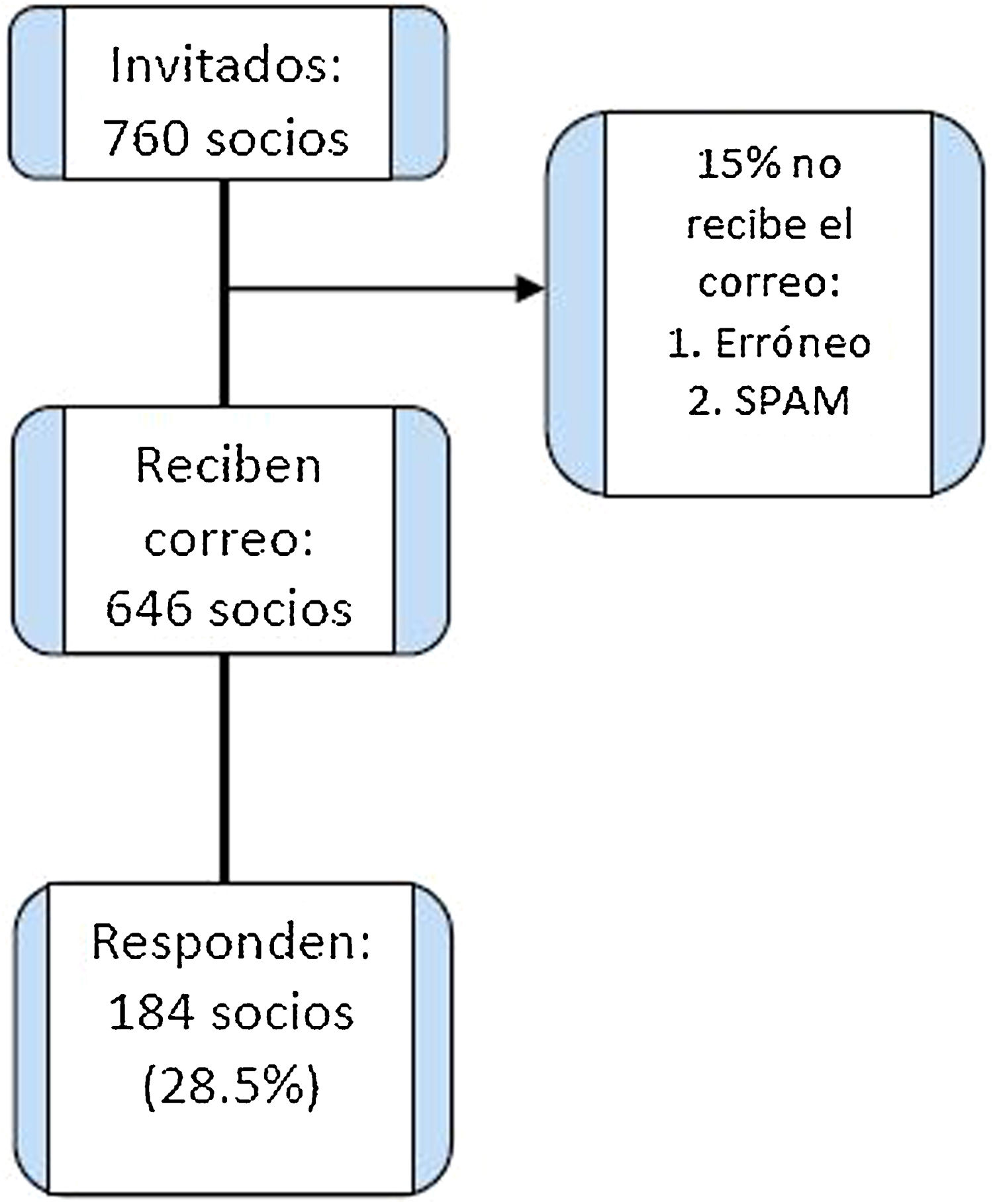
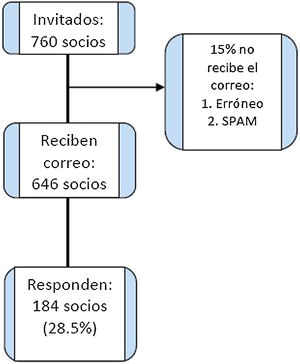
ResultsA total of 760 physicians (all GETECCU members at the time) were invited to take part by email after obtaining their addresses from the GETECCU database. It was estimated that 646 gastroenterologists from all over Spain received the email. We estimated that approximately 15% did not receive it, either because the address was wrong or because it went to SPAM as it was a bulk email.
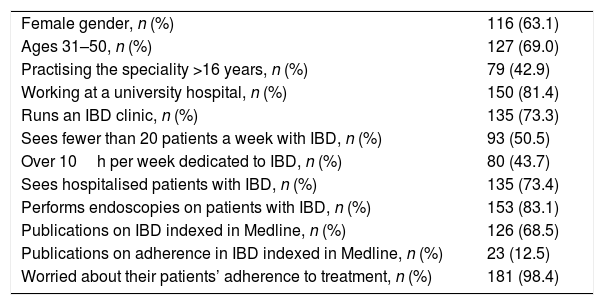
We obtained 184 responses (28.5%). The majority of the respondents were female (116/184; 63.1%), most were ages 31–50 (127/184; 69%) and 81.4% worked in a university hospital (150/184); 73.3% (135/184) ran a specific IBD clinic; 42.9% (79/184) had practised the speciality for over 16 years; 50.5% (93/184) saw more than 20 patients with IBD per week; and 43.5% (80/184) dedicated more than 10h a week to the IBD clinic. Although 68.5% (126/184) of the respondents had publications on IBD indexed in Medline, only 12.5% (23/184) had publications on IBD adherence (Table 1).
Characteristics of the physicians who answered the survey.
| Female gender, n (%) | 116 (63.1) |
| Ages 31–50, n (%) | 127 (69.0) |
| Practising the speciality >16 years, n (%) | 79 (42.9) |
| Working at a university hospital, n (%) | 150 (81.4) |
| Runs an IBD clinic, n (%) | 135 (73.3) |
| Sees fewer than 20 patients a week with IBD, n (%) | 93 (50.5) |
| Over 10h per week dedicated to IBD, n (%) | 80 (43.7) |
| Sees hospitalised patients with IBD, n (%) | 135 (73.4) |
| Performs endoscopies on patients with IBD, n (%) | 153 (83.1) |
| Publications on IBD indexed in Medline, n (%) | 126 (68.5) |
| Publications on adherence in IBD indexed in Medline, n (%) | 23 (12.5) |
| Worried about their patients’ adherence to treatment, n (%) | 181 (98.4) |
IBD: Inflammatory bowel disease.
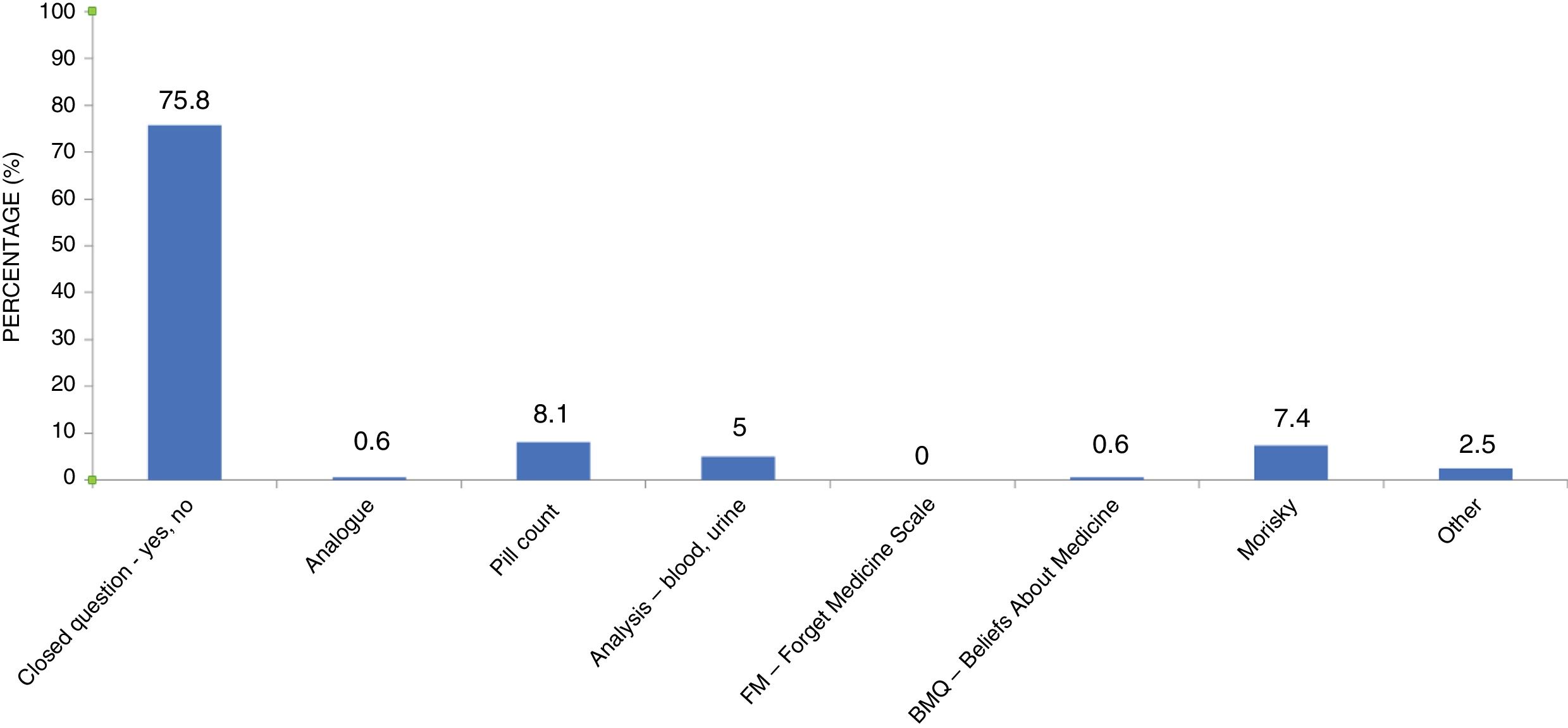
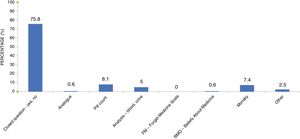
Despite the fact that almost 99% of the respondents considered that adherence to treatment was very important or important, almost one in four doctors did not measure adherence in their clinics. Of the 76.6% of the doctors who did, the most common method (used in 3/4 of cases) was with a closed question (yes/no) in a personal interview. Only slightly less than 25% used any objective method of measuring adherence (closed question-yes/no, analogue scale, tablet count, blood/urine test, FM-Forget Medicine Scale, BMQ-Beliefs About Medicine, Morisky, others) (Fig. 1).
Of the 76.6% of the physicians who assessed adherence, three quarters (77.7%) did so in all patients (regardless of the severity of the disease). However, the measurement of adherence was influenced by the type of treatment used; 45.6% of physicians measured adherence according to the treatment, being more common in patients on combined treatment with thiopurines and biological agents (44.6%), compared to salicylates (30.7%), thiopurines (18.8%) or biological agents (5.9%) alone.
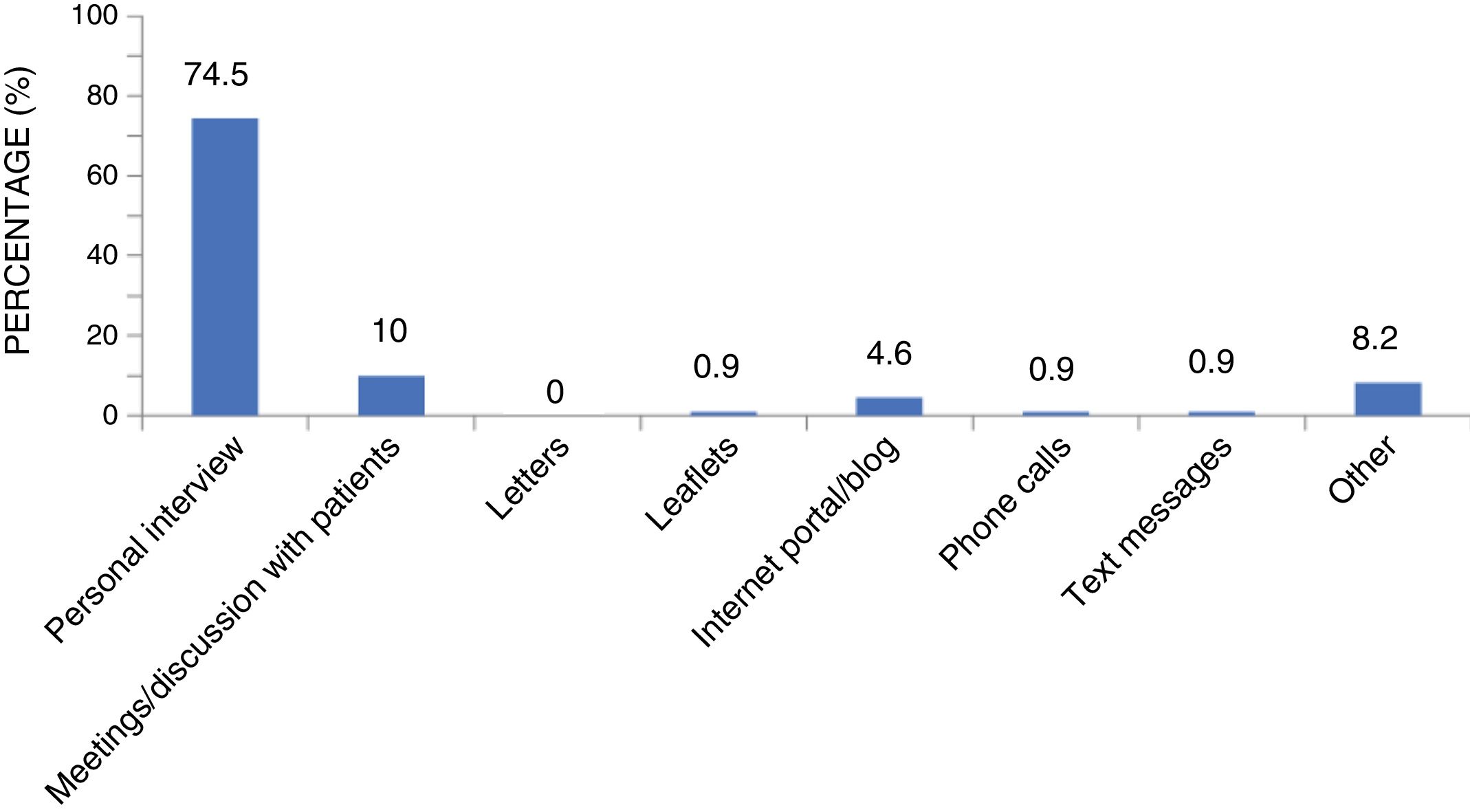
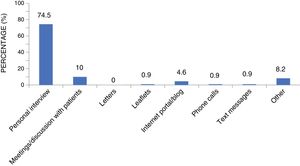
46.8% of the doctors did not use any system to improve adherence, despite the fact that 100% considered that doing so would mean a better prognosis for the patient. Among the doctors who did use some method to improve adherence, 74.5% did so through a personal interview during the same consultation with the patient, 10% had regular meetings with patients and 4.6% used websites or blogs (Fig. 2).
We analysed both the physician and patient factors related to whether or not treatment adherence was measured in the clinic and those related to using a system to improve adherence to treatment.
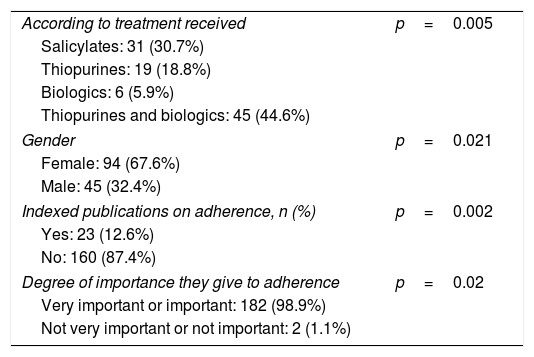
Statistically significant factors related to the measurement of adherence were the type of treatment received by the patient (salicylates: 31 [30.7%], thiopurines: 19 [18.8%], biologics: 6 [5.9%], thiopurines and biologics: 45 [44.6%], p=0.005); the gender of the doctor (female: 94 [67.6%], male: 45 [32.4%], p=0.021); having indexed publications in Medline about adherence in IBD (yes: 23 [12.6%], no: 160 [87.4%], p=0.002); and the degree of importance given to adherence by the doctor (very important or important: 182 [98.9%], not very important or not important: 2 [1.1%], p=0.02) (Table 2).
Factors related to the measurement of adherence.
| According to treatment received | p=0.005 |
| Salicylates: 31 (30.7%) | |
| Thiopurines: 19 (18.8%) | |
| Biologics: 6 (5.9%) | |
| Thiopurines and biologics: 45 (44.6%) | |
| Gender | p=0.021 |
| Female: 94 (67.6%) | |
| Male: 45 (32.4%) | |
| Indexed publications on adherence, n (%) | p=0.002 |
| Yes: 23 (12.6%) | |
| No: 160 (87.4%) | |
| Degree of importance they give to adherence | p=0.02 |
| Very important or important: 182 (98.9%) | |
| Not very important or not important: 2 (1.1%) | |
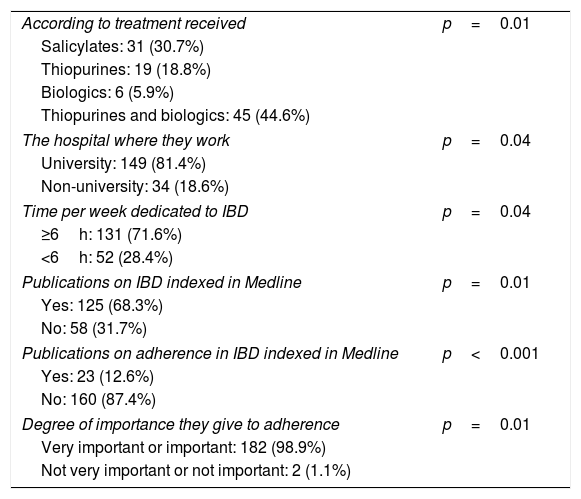
The factors related to the use of some system to improve adherence which had a statistically significant influence were the type of treatment received by the patient (salicylates: 31 [30.7%], thiopurines: 19 [18.8%], biologics: 6 [5.9%], thiopurines and biologics: 45 [44.6%], p=0.01); the type of hospital in which the doctor practised the speciality (university: 149 [81.4%], non-university: 34 [18.6%], p=0.04); the time per week the doctor dedicated to IBD (≥6h: 131 [71.6%], <6h: 52 [28.4%], p=0.04); whether or not the doctor had indexed publications in Medline about IBD (yes: 125 [68.3%], no: 58 [31.7%], p=0.01) and about adherence in IBD (yes: 23 [12.6%], no: 160 [87.4%], p<0.001); and the degree of importance given to adherence by the doctor (very important or important: 182 [98.9%], not very important or not important: 2 [1.1%], p=0.01) (Table 3).
Factors related to the use of adherence improvement systems.
| According to treatment received | p=0.01 |
| Salicylates: 31 (30.7%) | |
| Thiopurines: 19 (18.8%) | |
| Biologics: 6 (5.9%) | |
| Thiopurines and biologics: 45 (44.6%) | |
| The hospital where they work | p=0.04 |
| University: 149 (81.4%) | |
| Non-university: 34 (18.6%) | |
| Time per week dedicated to IBD | p=0.04 |
| ≥6h: 131 (71.6%) | |
| <6h: 52 (28.4%) | |
| Publications on IBD indexed in Medline | p=0.01 |
| Yes: 125 (68.3%) | |
| No: 58 (31.7%) | |
| Publications on adherence in IBD indexed in Medline | p<0.001 |
| Yes: 23 (12.6%) | |
| No: 160 (87.4%) | |
| Degree of importance they give to adherence | p=0.01 |
| Very important or important: 182 (98.9%) | |
| Not very important or not important: 2 (1.1%) | |
IBD: inflammatory bowel disease.
Our results show that although Spanish gastroenterologists attach great importance to adherence in the management of IBD, a quarter of doctors do not measure adherence in routine clinical practice. Among those who do, the most common method is the closed question (yes/no), with only 24.2% of the doctors who measured adherence using an objective method. Another important finding in our study was that 46.8% of the doctors did not use any system to improve adherence, despite the fact that 100% considered that doing so would mean a better prognosis for the patient. Once again, the most common method for improving adherence was the simple personal interview with the patient. Adherence was more likely to be assessed and promoted in patients receiving thiopurines or biologics.
Lack of adherence to treatment for diseases is a significant health problem, as it leads to worsening of the disease prognosis and an increase in healthcare costs. Adequate adherence has to be a priority in the treatment of any disease.1 The WHO believes that increasing the effectiveness of adherence interventions could have a much greater impact on the population's health than any improvement in a specific medical treatment.22 Therefore, before considering the lack of response to a treatment, good adherence to said treatment should be assessed and optimised, particularly in chronic diseases and those at risk of poor compliance.23 This is especially relevant in IBD, where non-adherence worsens the prognosis of the disease and increases morbidity and mortality rates and the cost of medical care.14,24,25 To optimise any treatment for IBD, all available strategies should therefore be used to monitor and improve adherence.
Such strategies have traditionally tended to focus on the patient, aiming to identify the factors involved in worse adherence, such as age or type of treatment. However, results have been inconclusive.10–13 Consequently, alternatives have been proposed and some studies have tried to focus on a change of model, aiming to discern the specific risk factors in each individual patient.26
Once the at-risk patient has been identified, an objective method needs to be used to measure adherence, but there are no universally accepted systems. Various means have been used, from simple personal interview to the measurement of drug metabolites, pill counting, collection of the drug from the pharmacy, electronic monitoring or the use of scales (Morisky questionnaire for IBD, visual analogue scale).27,28 Once the lack of adherence has been identified, different interventions need to be designed and used with the patient in order to improve adherence.29
Despite the widespread recognition of the problem of non-adherence, there has been virtually no study of how the doctor perceives this issue and what actions they take to improve it.20,21
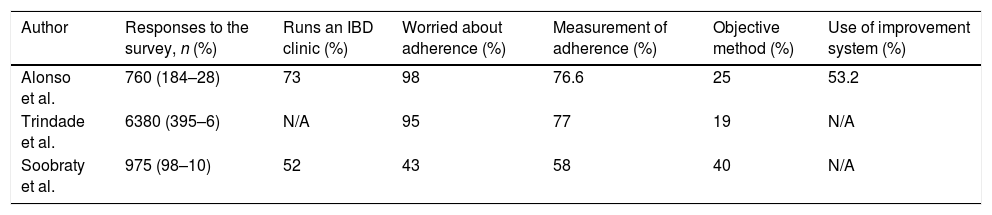
An English study by Soobraty et al.20 obtained a response rate of 10%. Only 52% were specialists, the rest being mainly resident physicians in training and even dietitians and biologists. This makes the sample very unrepresentative of routine medical practice, at least here in Spain. Significantly, non-adherence was perceived as a common problem by only 43%, which could be related to the low number of IBD specialists among those who responded to the survey. Despite that, 99% believed that improving adherence would improve the prognosis of patients with IBD and 80% believed that measuring adherence in the clinic is important. Once again, only 58% assessed adherence during the consultation and only 25% did so regularly. Only 40% used validated methods to do so while the other 60% asked the patient a closed question. However, 99% of the respondents thought that improving adherence would improve the prognosis of IBD and 80% thought measuring adherence was important.
The study by Trindade et al.21 obtained 402 responses for a gross response rate of 6%. Around 77% of the responding doctors assessed adherence to medication, but less than 20% of those used objective measurements. The rest assessed adherence through the interview with the patient.
The response rate of our study was significantly higher than in the two previous studies published to date. As found by Trindade et al., most of our respondents considered adherence to be very important but a significant percentage did not measure it in routine clinical practice. Moreover, those who did used an essentially non-objective method such as personal interview. The results of the English study and the survey carried out on North American doctors differ markedly from ours. This may be due to the heterogeneity of those surveyed in the other studies, with a low percentage of IBD specialists. As with previous studies, adherence was measured significantly more in patients using thiopurines or biologics, perhaps due to a greater concern on the part of the doctor about the disease prognosis.20,21
One result of our study that coincides with those published previously is the use of a closed question (yes/no) as the usual method of assessing non-adherence, despite it being well known that many patients can be reluctant to provide this information and even give imprecise estimates.30 Although there are other more objective methods such as direct measurement of the drug or its metabolites in blood or urine, counting the drugs picked up by the patient or adherence scales, only a quarter of the doctors who measured adherence used any objective method beyond the closed question. The percentages were also very low in the two previous studies (Table 4).
Comparison with previous publications (surveys carried out on doctors).
| Author | Responses to the survey, n (%) | Runs an IBD clinic (%) | Worried about adherence (%) | Measurement of adherence (%) | Objective method (%) | Use of improvement system (%) |
|---|---|---|---|---|---|---|
| Alonso et al. | 760 (184–28) | 73 | 98 | 76.6 | 25 | 53.2 |
| Trindade et al. | 6380 (395–6) | N/A | 95 | 77 | 19 | N/A |
| Soobraty et al. | 975 (98–10) | 52 | 43 | 58 | 40 | N/A |
N/A: not applicable.
Another important finding in our study, which had not previously been assessed, was that 46.8% of the doctors did not use any system to improve adherence, despite the fact that 100% considered that doing so would mean a better prognosis for the patient. Once again, the most common method for improving adherence was a simple personal interview with the patient, although more objective methods have shown better efficacy.31,32
Our study has several limitations. As in any study carried out using a survey, selection bias is inevitable, although we believe that the sample is probably representative of IBD physicians here in Spain. Nevertheless, the opinion of the respondents may not coincide with the routine practice of general gastroenterologists. It could be considered a bias that the doctors who responded would be the most interested in the subject of adherence, and that they therefore give it more consideration when consulting patients. Meanwhile, those who did not respond would be not as interested in the subject. Therefore, the study could have magnified the results (“100% consider adherence important”). It is also impossible to determine whether or not those who did not respond to the survey have the same views as those who did. One limitation to consider is that we did not survey the patients of the doctors who responded to the questionnaire, to correlate whether the opinion of the gastroenterologists included in this study was the same as that perceived by their patients with regard to clinic management of adherence; social desirability when responding to our survey may have overestimated the adherence data the doctors provided. In addition, as with any survey, those who responded may have been more involved in the management of IBD, or they may have given the answers they thought were expected of them or that they thought the researchers wanted. The limited response rate is inherent in these studies and involves a significant selection bias.
We should highlight our 28% response rate, which was significantly higher than the 6% and 10% of the only two previous studies on this subject.20,21 Ours is the first European study on gastroenterologists’ attitudes to adherence in patients with IBD. It is also the first to assess whether doctors use any system to improve adherence.
Determining adherence through an interview with the patient is the least valid method used, as it tends to overestimate adherence in a significant percentage of cases.28,30 It might be argued that measuring adherence takes time, a commodity not available in generally overworked clinics. There are objective methods, however, such as visual analogue scales, which do not need extra time.28 Moreover, there are other ways of improving adherence rates, such as online methods, which also do not require additional work during consultations.29,31 What does seem clear is that increasing adherence helps improve the prognosis of patients with IBD.7–9 Any strategy aimed at detecting and correcting poor adherence would therefore help improve the effectiveness of the drugs currently available.
ConclusionsIn the management of IBD, low levels of adherence to treatment are associated with significant clinical and financial repercussions. Traditionally, the emphasis has been on patient-related aspects, with little attention given to what the doctor is doing to assess and improve poor adherence. Our data show that although almost 100% of the respondents consider adherence to medical treatment to be important or very important, the majority (>75%) do not use objective methods to either measure or improve adherence in routine clinical practice. Future studies should examine whether or not a change in the attitude to adherence among doctors could lead to an improvement in the prognosis of patients with IBD.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Alonso-Abreu I, Alarcón-Fernández O, Carrillo-Palau M, Ramos-López L, Pérez Gisbert J, Chaparro M, et al. Encuesta de adherencia al tratamiento en enfermedad inflamatoria intestinal. Estudio ENADEII. Gastroenterol Hepatol. 2020;43:285–292.