Patients with head and neck cancer (HNC) have some problems such as dysfunction of breathing, eating, and/or speaking. The aim of this study was to examine efficacy of the stress management program for HNC patients (SMAP-HNC) compared with usual care (UC).
MethodWe conducted a pilot study of SMAP-HNC for depressive HNC patients between January 2016 and March 2018. The program contains psychoeducation, stress coping training, and operant reinforcement. The outcome measure was the Hospital Anxiety and Depression Scale (HADS), Functional Assessment of Cancer Therapy (FACT), and Brief Coping Inventory (COPE).
ResultsTwenty patients were randomly assigned to SMAP-HNC and UC group. Although a small sample sizes, there was no significant difference of depression score change between SMAP-HNC and UC group (Hedges’d g -0.83; 95% CI -1.80 to 0.13).
ConclusionsIt was the first study to conduct stress management program for HNC patients. Unfortunately, our trial designed as a randomized controlled trial is underpowered to make conclusion as to the efficacy of SMAP-HNC. However, there are some valuable suggestions to modify the stress management program in future.
Los pacientes con cáncer de cabeza y cuello (CCC) tienen algunos problemas como trastornos de la respiración, la alimentación y/o el habla. El objetivo de este estudio fue examinar la eficacia de un programa de control del estrés para pacientes con CCC (SMAP-HNC) en comparación con la atención habitual (AH).
MétodoLlevamos a cabo un estudio piloto de SMAP-HNC para pacientes depresivos con CCC entre enero de 2016 y marzo de 2018. El programa contiene psicoeducación, entrenamiento para afrontar el estrés y refuerzo operante. Las medidas de los resultado fueron la Hospital Anxiety and Depression Scale (HADS), la Functional Assessment of Cancer Therapy (FACT) y el Brief Coping Inventory (COPE).
ResultadosVeinte pacientes fueron asignados aleatoriamente al grupo SMAP-HNC y AH. Aunque los tamaños de las muestras son pequeños, no hubo diferencias significativas en el cambio en el puntaje de depresión entre el grupo SMAP-HNC y el grupo AH (g de Heges’s -0,83; IC del 95%: -1,80 a 0,13).
ConclusionesEs el primer estudio en emplera un programa de control del estrés para pacientes con CCC. Desafortunadamente, nuestro ensayo diseñado como un ensayo controlado aleatorio tiene poco poder para llegar a una conclusión sobre la eficacia de SMAP-HNC. Sin embargo, hay algunas sugerencias valiosas para modificar el programa de control del estrés en el futuro.
Head and neck cancer (HNC) is a general term for malignancy located around the oral, larynx, pharynx, or maxillofacial areas. The survival rate among patients with HNC has improved moderately with the progress in treatments (Machii & Saika, 2014; Wang et al., 2016). However, patients with HNC may suffer from variable dysfunction or disfigurement, and result in psychological problems with breathing, eating, swallowing, and/or speaking (Smith, Shuman, & Riba, 2017; Wotherspoon, Kanatas, & Rogers, 2018).
Depression is a common psychological problem for HNC patients. In fact, 7-50% of them are diagnosed with major depressive disorder, and it is higher rate of depression than that of any other cancer patients (Krebber et al., 2014; Lydiatt, Moran, & Burke, 2009). About 16% of patients with HNC are suicidal within a year of diagnosis (Henry et al., 2018), and the suicide rate among survivors with HNC is two times higher than the rate in survivors with other cancers (Osazuwa‐Peters et al., 2018). In addition, depression among HNC patients is a risk factor for low quality of life, poor treatment adherence, poor physical function, and a poor survival rate (Barber et al., 2015, 2016).
Psychological intervention has a beneficial effect on depression as well as medication, and several psychological interventions have been developed for patients with HNC (Richardson, Broadbent, & Morton, 2019; Senchak, Fang, & Bauman, 2019). Communication trainings or social skill trainings are related to quality of life among HNC patients (Brunner et al., 2018; Burns et al., 2017; Cousins, MacAulay, Lang, MacGillivray, & Wells, 2013). Cognitive behavioral therapy focused on lifestyle modification or fear of recurrence (Duffy et al., 2006; van der Meulen et al., 2013), and also group therapy based on supportive psychotherapy and psychoeducation have an effect on improvement of psychological distress (Allison et al., 2004; Katz, Irish, & Devins, 2004). However integrated psychotherapy effect is not clearly demonstrated in a systematic review for patients with HNC (Semple et al., 2013).
The following three problems seem to lie in the fact that psychotherapy is provided for patients with HNC. First, previous studies used population approach, and did not conduct the screening of depression (Luckett, Britton, Clover, & Rankin, 2011; Semple, Dunwoody, Kernohan, & McCaughan, 2009). Psychotherapy might have not positive effect on depression score in population approach because participants included not-depressed patients with HNC. Second, previous studies provided high-intensity psychotherapy such as a long-term support group or cognitive behavioral therapy with homework (Duffy et al., 2006; van der Meulen et al., 2013). Therefore, the drop-out rate of these study might be over 50%. Finally, patients with HNC prefer individual therapy rather than group therapy for the reason that many of them are men and problems with communication feature (Semple, Dunwoody, Sullivan, & Kernohan, 2006).
Recent studies have confirmed that stress coping was independent risk factor for depression in HNC patients (Ichikura, Yamashita, Sugimoto, Kishimoto, & Matsushima, 2018; Morris, Moghaddam, Tickle, & Biswas, 2018). Individual psychotherapy focused on problem-solving and stress management can contribute to depression reduction for survivors of HNC in practice (Kilbourn et al., 2013; Semple et al., 2009). However, these psychological programs are also high-intensity psychotherapy, and have methodological problem such as not a randomized controlled trial. We should conduct a short-term and low-intensity psychological program with problem-solving and stress management strategy for patients with HNC. The aim of this study was to examine the efficacy of stress management program for depressive patients with advanced head and neck cancer using an open-label randomized controlled trial. However, we reported our research as a pilot study due to early termination of our randomized controlled trial of stress management program for HNC patients.
MethodDesign and participantsThis was a pilot controlled study design of stress management program for patients with advanced HNC (SMAP-HNC study) from January 2016 through March 2018. Participants were not reached enough to calculated sample size, though the study was originally designed as a parallel, randomized, open-label study. Patients were recruited from hospitalized patients of the department of head and neck surgery, Medical Hospital, Tokyo Medical and Dental University in Tokyo (TMDU), Japan. TMDU is located at metropolitan area and have good access to public transportation. We included patients who (1) had a larynx, pharynx, or oral cancer, (2) had a pathological diagnosis of squamous cell carcinoma (SCC), (3) suspected to have advanced cancer (stage III to IV), (4) were after initial curative treatment, (5) were older than 20 years and younger than 79 years, and (6) had clinical depressive symptoms (Hospital Anxiety and Depression Scale score ≥ 11). The following patients were excluded from the study: those who were judged by their attending physicians not to participate in this trial because of severe physical, mental or cognitive problems (e.g., serious adverse event, delirium, or dementia) or those who has insufficient Japanese literacy skills.
The sample size calculation was based on previous meta-analysis, which was no significant change in levels of depression following psychotherapy for patients with head and neck cancer (Standardized mean differences = −.00) (Semple et al., 2013). Using the above information as our reference effect size and estimating intervention effect of SMAP-HNC at .20, and that of UC at .00, we needed 126 participants for 80% power and 5% significant level using a two-tailed test. Seventy patients per group were deemed sufficient, even if 10% of patients did not agree to participate or did not complete the questionnaire. However, actual percentage of patients declined to participate for this study was 56.50%.
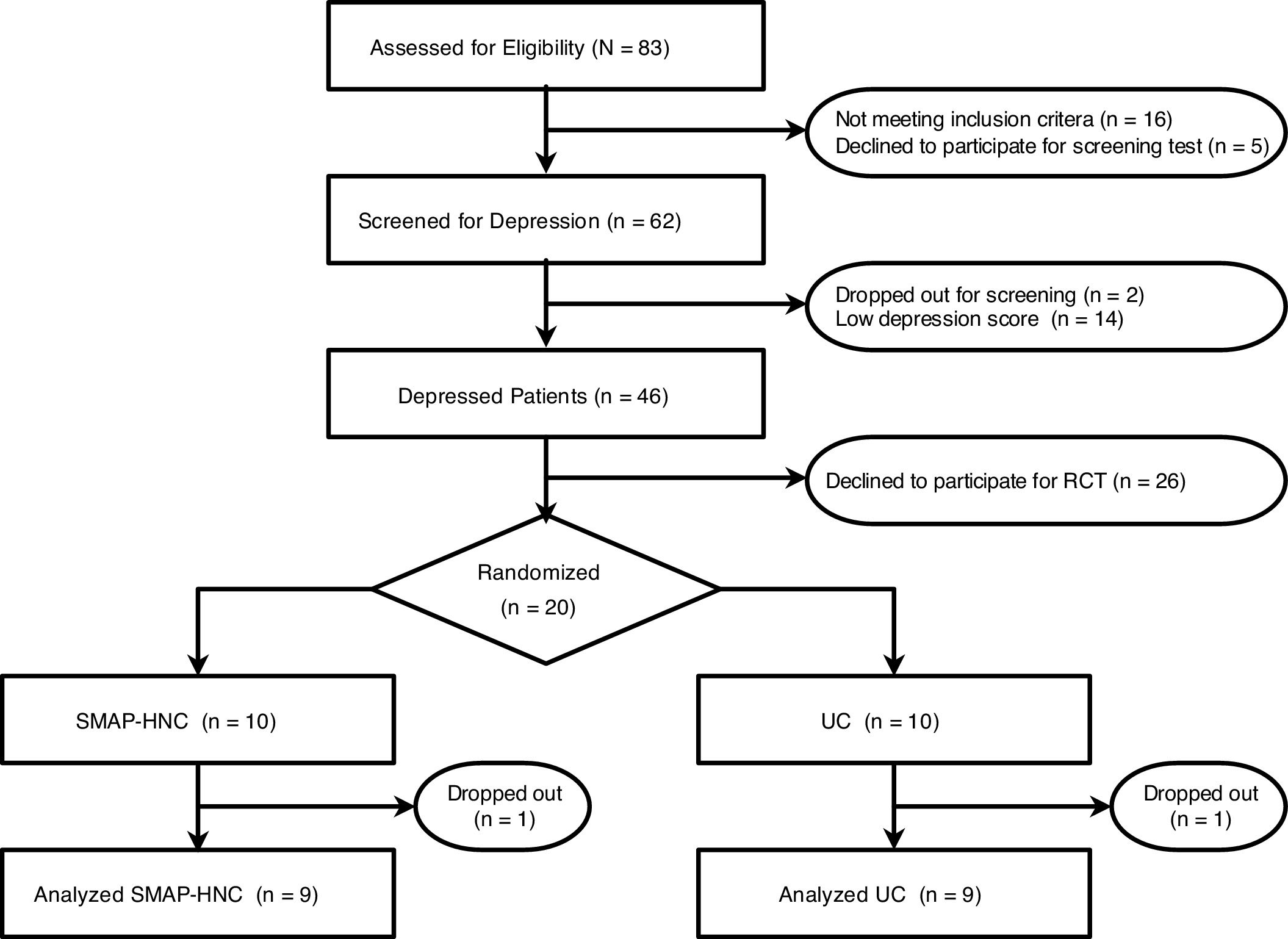
ProcedurePatients with meeting inclusion criteria and providing consent were screened for depression with Hospital Anxiety and Depression Scale (HADs). Patients with HADs ≥ 11 received direct contact from researchers, and provided another consent on the randomized controlled trial. They had completed the baseline assessment, and were randomly assigned to the following two groups. All outcomes were evaluated at three points, baseline, post-intervention, and three months after the intervention. This RCT was conducted with technical support from University Research Administration Center in TMDU, and reported according to the principles outlined in the CONSORT statement and checklist (Pandis, Chung, Scherer, Elbourne, & Altman, 2017). Informed consent was obtained from all participants in writing after verbal explanation. Participants answered anonymous questionnaires, and were managed by code number. The trial was approved by the independent Institutional Review Board (IRB) at Tokyo Medical and Dental University (R2015-026-01). The protocol of this trial was registered on UMIN Clinical Trials Registry (http://www.umin.ac.jp/ctr/index.htm), #UMIN000018900.
InterventionsStress Management Program. The program, which was based on a problem-solving training for head and neck cancer patients and stress coping training for HIV patients, was developed by three clinical psychologists and a psychiatrist. The developed program got clinical advice from three head and neck surgeons and two certified nurses in palliative care. We named this program as “Stress Management Program for Patients with Advanced Head and Neck Cancer (SMAP-HNC)”. SMAP-HNC is conducted by five clinical psychologists with more than three year experiences in hospital setting. The post-treatment session takes around 60 minutes at the time of hospital discharge, and the follow-up session takes around 30 minutes at the first visit. The main purpose of the SMAP-HNC is to (1) enhance the knowledge of stress coping skill, and (2) expand repertoire of stress coping skill. The themes of the post-treatment session are (a) psychoeducation about stress coping for head and neck cancer patients, (b) discussion about present stressors, stress responses, and stress coping, and (c) goal setting related alternative stress coping. Participants got homework between two sessions to do (d) self-monitoring, and (e) recording achievement rate of the goal. Finally, the themes of the follow-up session are (f) confirming the efficacy of alternative coping behavior, and (g) overview.
Usual Care (UC). All patients were treated with usual care by physicians, nurses, and other medical providers. Patients assigned to UC group were banned from receiving psychotherapy or counseling from clinical psychologists during the study period.
RandomizationParticipants who gave informed consent were randomly assigned in a 1:1 ratio to SMAP-HNC or UC by a computer-generated allocation sequence designed by HOPE eACReSS, a web-based randomized program, Fujitsu, Tokyo, Japan. Randomization was carried out with a fixed block size of 6 stratified for age (20-44 years, 45-64 years, or 65-79 years) and sex (men or women) using minimization method. After randomization, allocation result was informed patients face to face before intervention. This study was an open-labeled trial because of the difficulty of using blind experiment in psychotherapy.
InstrumentsDemographic and Clinical Characteristics. We collected demographic and clinical information from the case report form by attending physicians. We included the following data: age, sex, family, employment, primary cancer site, diagnosis cancer stage, ECOG performance status (ECOG-PS), history of cancer treatment, and other clinical problems (e.g. history of smoking).
Depression. Depression was evaluated using the Japanese version of the Hospital Anxiety & Depression Scale (HADS; Kugaya, Akechi, Okuyama, Okamura, & Uchitomi, 1998; Zigmond & Snaith, 1983), which is a 14-item self-related scale. It is a 4-point Likert-type scale ranging from 0 to 3 (overall score range: 0–42). The scale has two factors: anxiety and depression. We used an optimal cut-off point of 10/11 to screen for adjustment disorder or major depressive disorder in first screening for depression in Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR). This cut-off point gave high enough sensitivity (91.50%) and specificity (65.40%) among Japanese version of HADs.
Quality of Life (QOL). Quality of Life (QOL) were evaluated using the Functional Assessment of Cancer Therapy-Head and Neck Scale (FACT-H&N; List et al., 1996). It is a 38-item self-related scale used to measure function or well-being in cancer patients. The scale has five factors: Physical well-being (7 items), Social/family well-being (7 items), Emotional well-being (6 items), Functional well-being (7 items), and Head and neck cancer subscale (11 items). The reliability and validity of this measure were sufficiently supported in an earlier study (List et al., 1996).
Stress coping strategies were evaluated using the brief COPE, which is a Japanese abbreviated version of the COPE inventory (Carver, 1997; Otsuka, 2008). It consists of 28-items, 14 lower factors, and is a 4-point Likert-type scale ranging from 1 to 4. The reliability and validity of this measure were confirmed in an earlier study (Otsuka, 2008), and the Cronbach's alpha for each factor were .46 (Self-distraction), .47 (Active coping), .69 (Denial), .91 (Substance use), .72 (Use of emotional support), .80 (Use of instrumental support), .73 (Behavioral disengagement), .63 (Venting), .70 (Positive reframing), .67 (Planning), .70 (Humor), .63 (Acceptance), 64 (Religion), and .74 (Self-blame). It has been widely used in studies about cancer patients, especially HNC patients (Richardson, Morton, & Broadbent, 2016).
Insomnia. Insomnia were evaluated using the Japanese version of Athens Insomnia Scale (Okajima, Nakajima, Kobayashi, & Inoue, 2013; Soldatos, Dikeos, & Paparrigopoulos, 2000). It is an 8-item and 4-point Likert-type scale ranging from 0 to 3. It has been developed to assess the subjective sleep difficulty according to diagnostic criteria given in the International Classification of Diseases, 10th Revision. The reliability, validity, and also diagnostic accuracy of this measure were sufficiently supported in an earlier study (Soldatos, Dikeos, & Paparrigopoulos, 2003).
Statistical analysisPrimary outcome was amount of change in HADs depression score from baseline to post-intervention. Amount of change in HADs depression score were compared between groups using the independent t test and estimated the Hedges’s g and 95% confidence intervals (CIs). In addition, we show only descriptive statistics, and we did not perform any statistical tests to compare the difference between two groups in FACT, Brief COPE, and AIS score as secondary outcome.
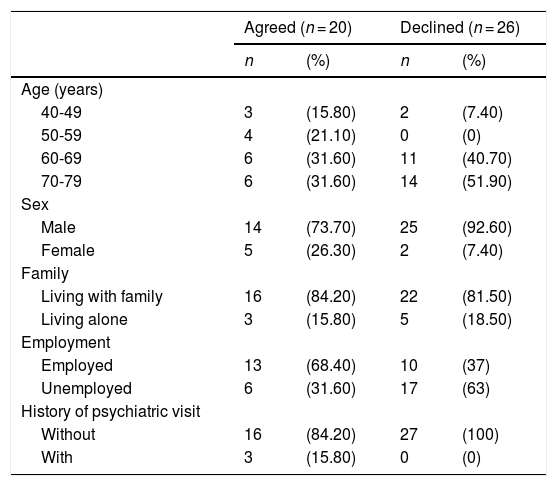
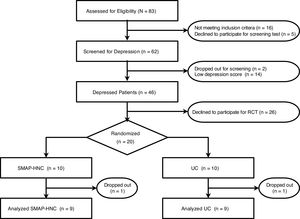
ResultsBaseline characteristicsFig. 1 is a flow diagram showing the number of participants at each stage of the study. Of the 83 patients with HNC, data from 46 participants with depression were considered potentially eligible. Twenty patients who agree to participation were enrolled, of whom 10 were randomly assigned to receive SMAP-HNC and 10 were assigned to receive UC. In addition, it has a higher percentage of patients with immediate pain following the treatments and refusal to participate than initially envisioned. Table1 shows the characteristics of patients declined to participate the study. Non-consent rate was 58.70%. The frequency of elderly (≥ 70 years old) patients and men was higher in the patients with declined (Table 1).
Characteristics of patients by agreement/decline for intervention (N = 46).
| Agreed (n = 20) | Declined (n = 26) | |||
|---|---|---|---|---|
| n | (%) | n | (%) | |
| Age (years) | ||||
| 40-49 | 3 | (15.80) | 2 | (7.40) |
| 50-59 | 4 | (21.10) | 0 | (0) |
| 60-69 | 6 | (31.60) | 11 | (40.70) |
| 70-79 | 6 | (31.60) | 14 | (51.90) |
| Sex | ||||
| Male | 14 | (73.70) | 25 | (92.60) |
| Female | 5 | (26.30) | 2 | (7.40) |
| Family | ||||
| Living with family | 16 | (84.20) | 22 | (81.50) |
| Living alone | 3 | (15.80) | 5 | (18.50) |
| Employment | ||||
| Employed | 13 | (68.40) | 10 | (37) |
| Unemployed | 6 | (31.60) | 17 | (63) |
| History of psychiatric visit | ||||
| Without | 16 | (84.20) | 27 | (100) |
| With | 3 | (15.80) | 0 | (0) |
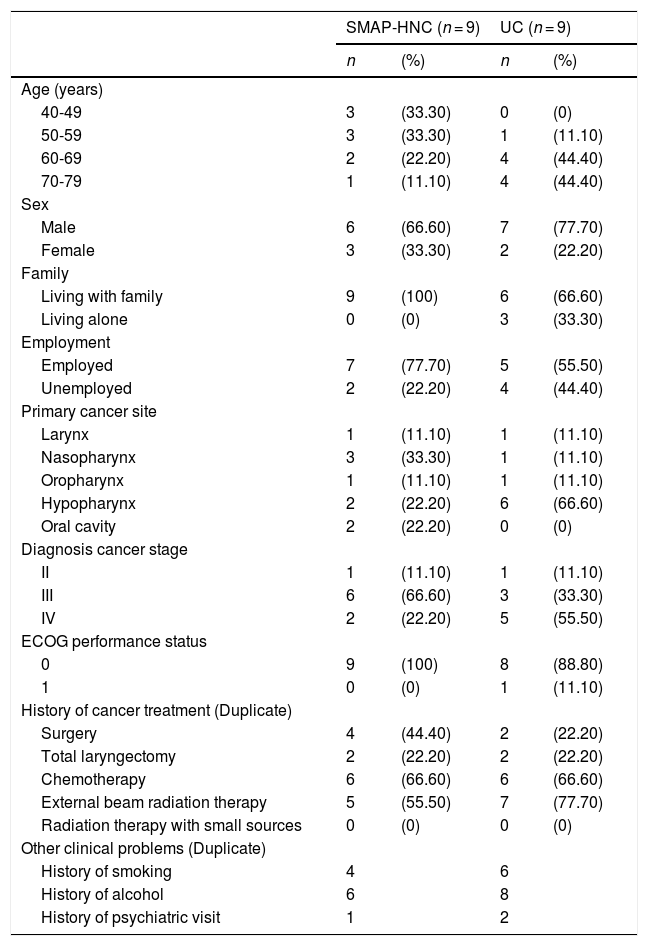
The baseline demographic and clinical characteristics of each group participants are shown in Table 2. Of the all 20 randomized patients, 18 patients who completed all the questionnaires items were included in this study.
Characteristics of the study participants (N = 18).
| SMAP-HNC (n = 9) | UC (n = 9) | |||
|---|---|---|---|---|
| n | (%) | n | (%) | |
| Age (years) | ||||
| 40-49 | 3 | (33.30) | 0 | (0) |
| 50-59 | 3 | (33.30) | 1 | (11.10) |
| 60-69 | 2 | (22.20) | 4 | (44.40) |
| 70-79 | 1 | (11.10) | 4 | (44.40) |
| Sex | ||||
| Male | 6 | (66.60) | 7 | (77.70) |
| Female | 3 | (33.30) | 2 | (22.20) |
| Family | ||||
| Living with family | 9 | (100) | 6 | (66.60) |
| Living alone | 0 | (0) | 3 | (33.30) |
| Employment | ||||
| Employed | 7 | (77.70) | 5 | (55.50) |
| Unemployed | 2 | (22.20) | 4 | (44.40) |
| Primary cancer site | ||||
| Larynx | 1 | (11.10) | 1 | (11.10) |
| Nasopharynx | 3 | (33.30) | 1 | (11.10) |
| Oropharynx | 1 | (11.10) | 1 | (11.10) |
| Hypopharynx | 2 | (22.20) | 6 | (66.60) |
| Oral cavity | 2 | (22.20) | 0 | (0) |
| Diagnosis cancer stage | ||||
| II | 1 | (11.10) | 1 | (11.10) |
| III | 6 | (66.60) | 3 | (33.30) |
| IV | 2 | (22.20) | 5 | (55.50) |
| ECOG performance status | ||||
| 0 | 9 | (100) | 8 | (88.80) |
| 1 | 0 | (0) | 1 | (11.10) |
| History of cancer treatment (Duplicate) | ||||
| Surgery | 4 | (44.40) | 2 | (22.20) |
| Total laryngectomy | 2 | (22.20) | 2 | (22.20) |
| Chemotherapy | 6 | (66.60) | 6 | (66.60) |
| External beam radiation therapy | 5 | (55.50) | 7 | (77.70) |
| Radiation therapy with small sources | 0 | (0) | 0 | (0) |
| Other clinical problems (Duplicate) | ||||
| History of smoking | 4 | 6 | ||
| History of alcohol | 6 | 8 | ||
| History of psychiatric visit | 1 | 2 | ||
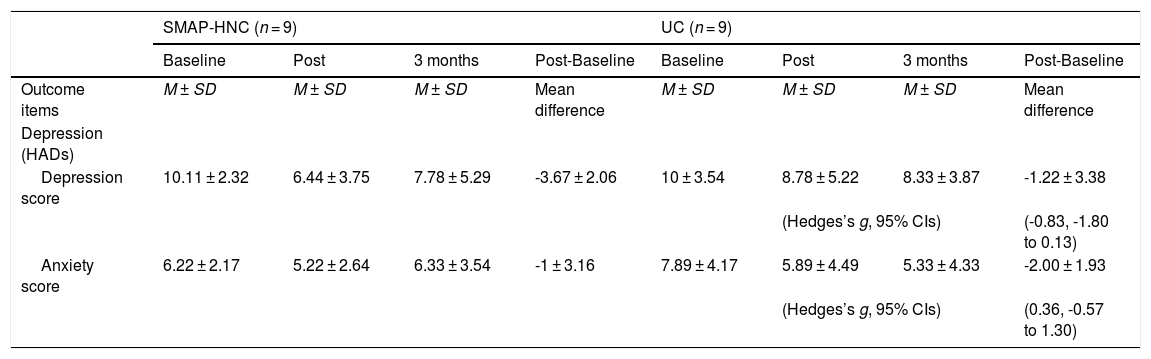
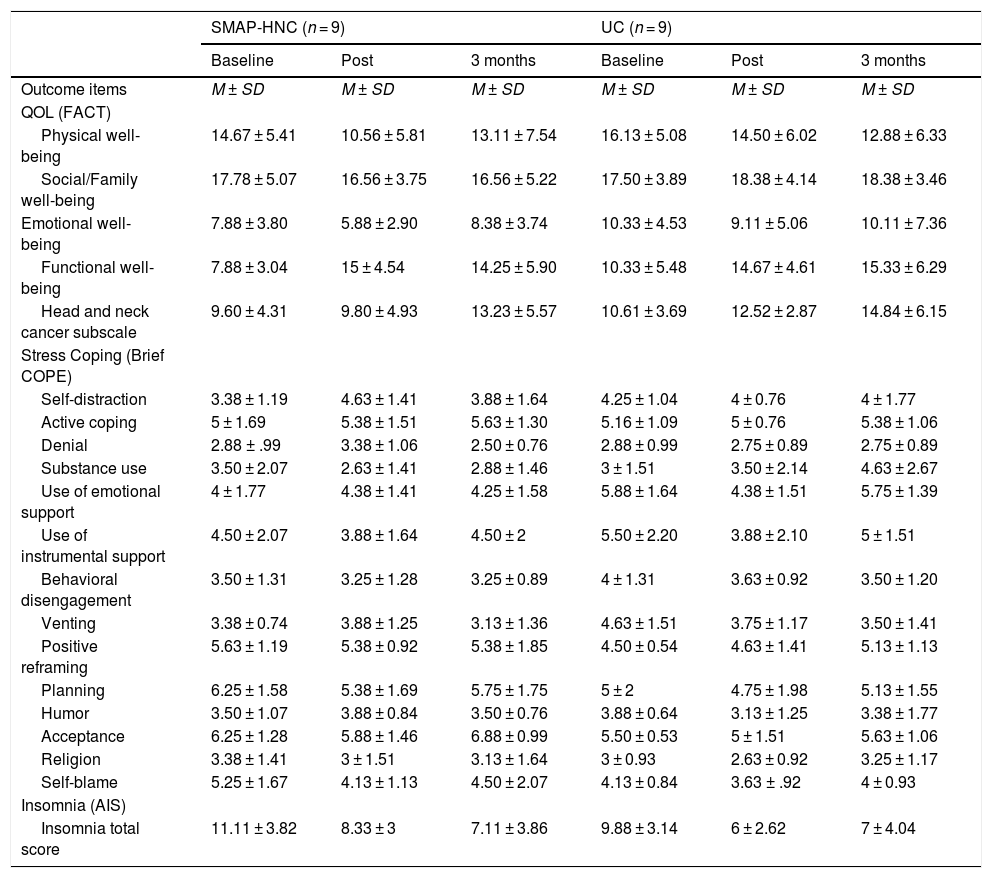
The primary outcome change among study participants are shown in Table 3. The independent t test revealed that there was no significant difference of HADs depression (Hedges’d g -0.83; 95% CI -1.80 to 0.13) and anxiety (Hedges’d g 0.36; 95% CI -0.57 to 1.30) between two groups. However, this clinical trial is underpowered to perform some statistical test and compare the differences between two intervention groups. According to the descriptive data, post-baseline mean difference of depression score of SMAP-HNC is higher than that score of UC. Descriptive data of secondary outcome are shown in Table 4. We did not carry out the relevant statistical analysis for secondary outcome.
Primary outcome among study participants (N = 18).
| SMAP-HNC (n = 9) | UC (n = 9) | |||||||
|---|---|---|---|---|---|---|---|---|
| Baseline | Post | 3 months | Post-Baseline | Baseline | Post | 3 months | Post-Baseline | |
| Outcome items | M ± SD | M ± SD | M ± SD | Mean difference | M ± SD | M ± SD | M ± SD | Mean difference |
| Depression (HADs) | ||||||||
| Depression score | 10.11 ± 2.32 | 6.44 ± 3.75 | 7.78 ± 5.29 | -3.67 ± 2.06 | 10 ± 3.54 | 8.78 ± 5.22 | 8.33 ± 3.87 | -1.22 ± 3.38 |
| (Hedges’s g, 95% CIs) | (-0.83, -1.80 to 0.13) | |||||||
| Anxiety score | 6.22 ± 2.17 | 5.22 ± 2.64 | 6.33 ± 3.54 | -1 ± 3.16 | 7.89 ± 4.17 | 5.89 ± 4.49 | 5.33 ± 4.33 | -2.00 ± 1.93 |
| (Hedges’s g, 95% CIs) | (0.36, -0.57 to 1.30) | |||||||
Note. p < .05*. 95%CIs = Confidence Intervals.
Descriptive data of secondary outcome (N = 18).
| SMAP-HNC (n = 9) | UC (n = 9) | |||||
|---|---|---|---|---|---|---|
| Baseline | Post | 3 months | Baseline | Post | 3 months | |
| Outcome items | M ± SD | M ± SD | M ± SD | M ± SD | M ± SD | M ± SD |
| QOL (FACT) | ||||||
| Physical well-being | 14.67 ± 5.41 | 10.56 ± 5.81 | 13.11 ± 7.54 | 16.13 ± 5.08 | 14.50 ± 6.02 | 12.88 ± 6.33 |
| Social/Family well-being | 17.78 ± 5.07 | 16.56 ± 3.75 | 16.56 ± 5.22 | 17.50 ± 3.89 | 18.38 ± 4.14 | 18.38 ± 3.46 |
| Emotional well-being | 7.88 ± 3.80 | 5.88 ± 2.90 | 8.38 ± 3.74 | 10.33 ± 4.53 | 9.11 ± 5.06 | 10.11 ± 7.36 |
| Functional well-being | 7.88 ± 3.04 | 15 ± 4.54 | 14.25 ± 5.90 | 10.33 ± 5.48 | 14.67 ± 4.61 | 15.33 ± 6.29 |
| Head and neck cancer subscale | 9.60 ± 4.31 | 9.80 ± 4.93 | 13.23 ± 5.57 | 10.61 ± 3.69 | 12.52 ± 2.87 | 14.84 ± 6.15 |
| Stress Coping (Brief COPE) | ||||||
| Self-distraction | 3.38 ± 1.19 | 4.63 ± 1.41 | 3.88 ± 1.64 | 4.25 ± 1.04 | 4 ± 0.76 | 4 ± 1.77 |
| Active coping | 5 ± 1.69 | 5.38 ± 1.51 | 5.63 ± 1.30 | 5.16 ± 1.09 | 5 ± 0.76 | 5.38 ± 1.06 |
| Denial | 2.88 ± .99 | 3.38 ± 1.06 | 2.50 ± 0.76 | 2.88 ± 0.99 | 2.75 ± 0.89 | 2.75 ± 0.89 |
| Substance use | 3.50 ± 2.07 | 2.63 ± 1.41 | 2.88 ± 1.46 | 3 ± 1.51 | 3.50 ± 2.14 | 4.63 ± 2.67 |
| Use of emotional support | 4 ± 1.77 | 4.38 ± 1.41 | 4.25 ± 1.58 | 5.88 ± 1.64 | 4.38 ± 1.51 | 5.75 ± 1.39 |
| Use of instrumental support | 4.50 ± 2.07 | 3.88 ± 1.64 | 4.50 ± 2 | 5.50 ± 2.20 | 3.88 ± 2.10 | 5 ± 1.51 |
| Behavioral disengagement | 3.50 ± 1.31 | 3.25 ± 1.28 | 3.25 ± 0.89 | 4 ± 1.31 | 3.63 ± 0.92 | 3.50 ± 1.20 |
| Venting | 3.38 ± 0.74 | 3.88 ± 1.25 | 3.13 ± 1.36 | 4.63 ± 1.51 | 3.75 ± 1.17 | 3.50 ± 1.41 |
| Positive reframing | 5.63 ± 1.19 | 5.38 ± 0.92 | 5.38 ± 1.85 | 4.50 ± 0.54 | 4.63 ± 1.41 | 5.13 ± 1.13 |
| Planning | 6.25 ± 1.58 | 5.38 ± 1.69 | 5.75 ± 1.75 | 5 ± 2 | 4.75 ± 1.98 | 5.13 ± 1.55 |
| Humor | 3.50 ± 1.07 | 3.88 ± 0.84 | 3.50 ± 0.76 | 3.88 ± 0.64 | 3.13 ± 1.25 | 3.38 ± 1.77 |
| Acceptance | 6.25 ± 1.28 | 5.88 ± 1.46 | 6.88 ± 0.99 | 5.50 ± 0.53 | 5 ± 1.51 | 5.63 ± 1.06 |
| Religion | 3.38 ± 1.41 | 3 ± 1.51 | 3.13 ± 1.64 | 3 ± 0.93 | 2.63 ± 0.92 | 3.25 ± 1.17 |
| Self-blame | 5.25 ± 1.67 | 4.13 ± 1.13 | 4.50 ± 2.07 | 4.13 ± 0.84 | 3.63 ± .92 | 4 ± 0.93 |
| Insomnia (AIS) | ||||||
| Insomnia total score | 11.11 ± 3.82 | 8.33 ± 3 | 7.11 ± 3.86 | 9.88 ± 3.14 | 6 ± 2.62 | 7 ± 4.04 |
The primary aim of our study was to evaluate the efficacy of SMAP-HNC for depressive patients with advanced HNC. It was the most important thing that this was a valuable first research which attempted randomized controlled trial of the psychological intervention better suited for HNC patients. Unfortunately, the findings of this study revealed that SMAP-HNC have no effect on depression. It disagrees with some previous studies, which showed that psychotherapy including stress management intervention is effective for psychological distress among advanced cancer patients (de la Torre-Luque, Gambara, López, & Cruzado, 2016; Okuyama, Akechi, Mackenzie, & Furukawa, 2017; Tang, Liu, Wu, & Shi, 2020). We suggest that the contents of SMAP-HNC might not have suited for patients with HNC in terms of the following three points. First, participants of this study could not improve their motivation for acquisition of stress coping skill during this program, though many HNC patients desire face to face sessions, providing coping strategies (Richardson, Morton, & Broadbent, 2015). Our past study indicated that HNC patients commonly use the dependent coping strategy including smoking, drinking, seeking support, or engaging self-distraction (Ichikura et al., 2018). The HNC patients in our study also may depend on someone or something, and may not take the initiative in dealing with stress coping strategies. Second, participants of this study might have feelings of resistance toward psychotherapy. Japanese cancer patients have trouble talking about themselves and feel uncomfortable receive psychological interventions (Endo et al., 2008). Non-consent rate especially in elderly or male patients was actually high in this study. Third, physical treatments status might have led to difficult to participate this program. HNC patients may reject to participate SMAP-HNC because they are in bad physical condition from the side effects of chemotherapy or radiation therapy. Therefore, we will make a suggestion for the development of modified stress management program for HNC patients in the future. We should deliver psychoeducation or motivational interviewing at the beginning of SMAP-HNC program, or take advantage of some specialist team to remove barriers to psychotherapy. In addition, the program intervention would be conducted better during a stable period of patients’ life, though SMAP-HNC was conducted in conjunction with clinic appointment directly after hospital discharge due to short-handed in our study. However, our trial is obviously underpowered to make conclusion as to the efficacy of SMAP-HNC because of early terminated before sufficient sample size were available. Short-term problem-solving approach is one of the effective treatment for depression among patients with HNC (Semple et al., 2009). SMAP-HNC also have a potential impact on depression for HNC patients, if there is sufficient sample size. Additionally, this study might have set a short assessment period to determine the efficacy of the intervention. Positive psychotherapy focused on stress coping style for cancer patients promote patients’ post traumatic growth and behavior modification (Ochoa, Casellas-Grau, Vives, Font, & Borràs, 2017). Therefore, the SMAP-HNC might have need longer time period to take effect.
Our study has two limitations. First, we did not perform all planned statistical tests because of the small sample size. Participants of the intervention group were actually older and more advanced clinical stage than those of control group. We could not compare the difference due not to match background data between two groups. Second, this early termination may be a peculiarly Japanese problem due to implementing a single-center study in Japan. In clinical situation, we should customize stress management program or any other psychotherapy to patients’ need or characteristic.
Our study cannot clarify the efficacy of the stress management program for depressive patients with HNC due to small sample size of this study. However, the results of this study offer some suggestions to modify the stress management program for patients with HNC in the future. Patients with HNC have the potential to frequently decline or drop out early from high-intensity psychological interventions including stress management program. Motivation for psychotherapy is the important factor in the introduction and continuance of psychological interventions by psychiatrists or clinical psychologists. In addition, the data of this study are valid and ought to be included in any future meta-analyses or systematic reviews of this topic.
FundingThis study was supported by SPS KAKENHI Grant Number JP15K08900, and scholarship donations from Astellas Pharma Inc., Mitsubishi Tanabe Pharma Corporation, MSD K.K., Otsuka Pharmaceutical, Pfizer Inc., and Takeda Pharmaceutical Company Limited. However, the funders did not have a directly financial relationship with us, and had no role in the study design, data collection and analysis, decision to publish, or the preparation of the manuscript.
We are grateful to Aya Yamashita (Clinical Psychologist), Yuko Motomatsu (Certified Nurse in Palliative Care), Shigeyo Uzawa (Certified Nurse in Palliative Care) for providing many comments about SMAP-HNC program contents. Additionally, we would like to thank Satoko Ogi (Clinical Nurse), Tomoko Sugano (Clinical Psychologist), and all collaborators in Medical Hospital, Tokyo Medical and Dental University for assisting in recruiting participants. We are also grateful to Research University Promotion Organization URA Room, Tokyo Medical and Dental University for assisting us with the statistical analyses.