The outbreak of COVID-19 and the lack of vaccine made extraordinary actions such as social distancing necessary. While some individuals experience the restrictions on daily life as a heavy burden, others adapt to the situation and try to make the best of it. The present longitudinal study investigated the extent and predictors of the burden induced by the outbreak of COVID-19 in Germany.
MethodData were assessed in October 2019 using the DASS-21 and the PMH-Scale, and in March 2020 adding a six-item measure of burden and a 2-item rating of sense of control.
ResultsIn a sample of 436 participants, about 28% stayed in self-quarantine, 22 persons had relevant symptoms and one person was positively tested for COVID-19. Most participants experienced medium to high levels of burden but tried to make the best of it. Stress symptoms in 2019 predicted a higher level of burden and PMH predicted a lower level of burden in March 2020. Remarkably, depression and anxiety symptoms did not significantly predict burden. The protective effect of PMH and the negative impact of stress symptoms were mediated by perceived sense of control.
ConclusionsThe results emphasize the protective effect of PMH in extraordinary situations such as the current outbreak of COVID-19.
El brote COVID-19 y la falta de vacuna hicieron necesarias acciones extraordinarias como la distancia social. Algunas personas experimentan las restricciones en la vida diaria como sobrecarga emocional y otras se adaptan a la situación, tratando de sacar lo mejor de ella. Se investigó el alcance y predictores de sobrecarga emocional inducida por el COVID-19 en Alemania.
MétodoSe evaluaron niveles de estrés y salud mental positiva en octubre de 2019 con DASS-21 y Escala-PMH, y en marzo de 2020, agregando medidas de sobrecarga emocional y percepción de control.
ResultadosEn una muestra de 436 participantes, el 28% permaneció en cuarentena, 22 personas tuvieron síntomas relevantes y una dio positivo en COVID-19. La mayoría experimentaron niveles de sobrecarga emocional medio-alto, aunque trataron de sobrellevar la situación lo mejor posible. Los síntomas de estrés en octubre 2019 predijeron un nivel de sobrecarga más elevado en marzo 2020 y, contrariamente, los niveles de salud mental positiva en octubre 2019 predijeron un menor nivel de sobrecarga emocional en marzo 2020. Sorprendentemente, los síntomas de depresión y ansiedad no predijeron la sensación de sobrecarga posterior. El efecto protector de la salud mental positiva y el impacto negativo de los síntomas de estrés fueron mediados por la percepción de control.
ConclusionesSe resalta el efecto protector de la salud mental positiva en situaciones extraordinarias como el brote COVID-19.
In December 2019, the outbreak of the coronavirus disease 2019 (COVID-19; severe acute respiratory syndrome coronavirus 2, SRS-CoV-2) was detected in Wuhan (China) (Xu et al., 2020). One month later, it was declared to be a Public Health Emergency of International Concern (World Health Organization, 2020b) and on March 11, 2020, COVID-19 was recognized as a pandemic that spread across over 190 countries within a short period of time (World Health Organization, 2020a). On April 7, 2020, there were over 1.348.000 confirmed cases of COVID-19, over 286.000 recovered cases and over 74.000 deaths globally. With over 367.000 total cases the U.S. was by far the most affected country, followed by Spain (>136.000 cases), Italy (>132.000 cases) and Germany (>103.000 cases; see https://www.worldometers.info/coronavirus/).
COVID-19 symptoms include cough, fever and shortness of breath. A loss of taste and smell is also often noticeable. It mainly spreads by respiratory droplets and by touching contaminated surfaces (Zhou et al., 2020). The time between exposure and symptom onset ranges between two and 14 days. Contagion is possible before the symptom onset (Liu, Gayle, Wilder-Smith, & Rocklöv, 2020). Considering spread and mortality rates, as well as a lack of medication treatments or vaccines, many governments have declared national quarantines. These range from advised self-isolation to travel restrictions and a total ban on leaving home (Sohrabi et al., 2020). The main aim is to slow down the spread of COVID-19 by reducing physical contact within the population.
The restrictions on daily life and the uncertainty about the duration of the extraordinary measures cause different reactions in the population. While some people perceive them as a heavy psychological burden resulting in an enhanced degree of uncertainty, frustration and anxiety – a maladaptive reaction, other individuals try to maintain their daily routine as far as possible and to make the best of the situation by adapting to the current life conditions – an adaptive reaction. The way people perceive and deal with the situation caused by COVID-19 can have an impact on their mental and physical health and on their willingness to actively participate in the much needed action. It is therefore urgent to investigate predictors of adaptive and maladaptive psychological responses to COVID-19.
The present study had the following aims. First, the extent of exposure (including quarantine) and the experienced burden caused by COVID-19 was investigated exploratorily. In Germany, the population is currently advised to reduce physical contacts and to stay at home as far as possible. Public gatherings are limited to a maximum of two individuals. Persons who were tested positive for COVID-19 and are not hospitalized, or who were in contact with positively tested individuals are required to stay in domestic quarantine (i.e., not leaving home) for at least two weeks (Robert Koch Institut, 2020).
Second, the study aimed to identify factors that may predict the level of burden caused by COVID-19. Dual-factor models consider mental health to be more than just the absence of mental illness (e.g., Keyes, 2005; Suldo & Shaffer, 2008; World Health Organization, 2014). Mental health consists of two interrelated but relatively separate dimensions: positive and negative (Lukat, Margraf, Lutz, van der Veld, & Becker, 2016). Based on this framework, the study focused both on the negative as well as on the positive factors that can serve as potential predictors of the experience of burden caused by an extraordinary situation. Individuals with enhanced levels of depression, anxiety and stress symptoms are prone to maladaptive response to uncertain new situations. They tend to ruminate and worry and are overwhelmed by situations they experience as uncontrollable. The lack of adequate coping strategies enhances feelings of burden and hopelessness (Bonanno, Brewin, Kaniasty, & La Greca, 2010; Gorday, Rogers, & Joiner, 2018; Misra & McKean, 2000). Furthermore, symptoms of depression, anxiety and stress are associated with the perception of less social support and resilience which enhances the experience of burden by unexpected negative situations (Brailovskaia, Schönfeld, Kochetkov, & Margraf, 2019; Hoorelbeke, Marchetti, De Schryver, & Koster, 2016; Ren, Qin, Zhang, & Zhang, 2018). Moreover, they contribute to somatic symptom burden and negatively impact effectivity of treatments. Their decrease reduces the experienced burden (Katon, Lin, & Kroenke, 2007; Toukhsati et al., 2017).
In contrast, positive mental health (PMH) – social, emotional and psychological well-being (Lukat et al., 2016) – was reported to contribute to positive affect, to confer resilience, to reduce negative consequences of unpleasant experiences and to foster adaptive response to uncertain situations (e.g., Iasiello, van Agteren, Keyes, & Cochrane, 2019; Teismann, Brailovskaia, & Margraf, 2019). For example, PMH positively predicts remission from panic disorder, agoraphobia and specific phobia in outpatients (Teismann, Brailovskaia, Totzeck, Wannemüller, & Margraf, 2018); it reduces adjustment disorder symptoms after the experience of stressful life events (Truskauskaite-Kuneviciene, Kazlauskas, Ostreikaite-Jurevice, Brailovskaia, & Margraf, 2020). Moreover, it buffers the effect of daily stress (Brailovskaia, Teismann, & Margraf, 2020b) and of cyberbullying (Brailovskaia, Teismann, & Margraf, 2018) on suicide ideation and suicide behavior. And it reduces the risk of suicide ideation of individuals with enhanced levels of depression symptoms (Teismann, Forkmann, et al., 2018). Individuals with enhanced PMH typically have a high sense of control and are able to adaptively cope with unexpected situations (Niemeyer, Bieda, Michalak, Schneider, & Margraf, 2019). Note that sense of control can reduce hopelessness and feelings of helplessness, and increase resilience which contributes to the experience of less burden (Assari, 2017; Yu, Ren, Huang, & Wang, 2018). Given these findings, sense of control (Lachman & Weaver, 1998) seems to be an important factor that should reinforce the protective impact of PMH and buffer the experience of burden in individuals with enhanced symptoms of depression, anxiety and stress.
On this background, depression, anxiety and stress symptoms were expected to predict a higher level of experienced burden induced by the current COVID-19 situation (Hypothesis 1); PMH was assumed to predict a lower level of experienced burden (Hypothesis 2). Furthermore, it was hypothesized that sense of control mediates the association between the burden experience and depression, anxiety and stress symptoms (Hypothesis 3), as well as PMH (Hypothesis 4).
MethodParticipants and procedureThe sample comprised of 436 participants (77.30% women; Mage (SDage) = 27.01 (6.41), range: 19–71; occupation: 66.30% students, 32.10% employees, 1.40% unemployed, 0.20% retired; marital status: 44.30% single, 42% with romantic partner, 13.80% married). Data were collected March 20 to March 28, 2020, by an online survey. On March 20, an invitation e-mail that included a link leading to the online survey was sent to a randomly collected group of 500 persons who had participated in an online survey in October 2019 in the frame of the “Bochum Optimism and Mental Health (BOOM)” project (Margraf & Schneider, 2017). All participants are current or former students of a large university in the Ruhr region and had previously agreed to be contacted for research investigations. There were no specific requirements for participation which was voluntary and compensated by course credits for students. The responsible Ethics Committee approved the implementation of the present study. All participants were properly instructed and gave online their informed consent to participate. The survey in October 2019 that served as baseline measurement (BL) included data on PMH, depression, anxiety and stress symptoms. The survey in March 2020 assessing the acute response to the COVID-19 situation served as follow-up measurement (FU). It included data on exposure, quarantine and burden by COVID-19, PMH, sense of control, depression, anxiety and stress symptoms. Power analyses (G*Power program, version 3.1) revealed that the sample size was sufficient for valid results (power > .80, α = .05, effect size: f2 = .15; cf., Mayr, Erdfelder, Buchner, & Faul, 2007).
InstrumentsCurrent exposure, quarantine and burden by COVID-19. Participants were asked to rate (1) to what extent they are currently affected by COVID-19 (multiple choices possible; e.g., “I have been tested positive myself”); (2) how useful they currently consider quarantine to be (rated on a visual analogue scale ranging from 0 (not useful at all) to 100 (extremely useful)); (3) whether they are currently in quarantine (0 = no, 1 = yes); (3a) if they are in quarantine, what is the reason for the quarantine (e.g., “I was advised to”); (3b) if they are in quarantine, for how long they had been in quarantine (in days); (3c) if they are in quarantine, how they spend their time (multiple choices possible: e.g., “I pursue my professional activity from home”); 4) to what extent they are burdened by COVID-19 (six items rated on a 7-point Likert scale (1 = I do not agree, 7 = I totally agree), e.g., “I am afraid of the current situation”; scale reliability: Cronbach’s αT2 = .75). The higher the sum scores, the higher the burden caused by COVID-19.
Depression, Anxiety and Stress Symptoms. The Depression Anxiety Stress Scales 21 (DASS-21; Lovibond & Lovibond, 1995) measured symptoms of depression, anxiety and stress with respectively seven items per subscale (e.g., depression subscale: “I couldn’t seem to experience any positive feeling at all”, anxiety subscale: “I felt scared without any good reason”, stress subscale: “I tended to over-react to situations”). The items are rated on a 4-point Likert scale (0 = did not apply to me at all; 3 = applied to me very much or most of the time; scale reliability: depression subscale: αT1 = .90, αT2 = .89; anxiety subscale: αT1 = .81, αT2 = .74; stress subscale: αT1 = .87, αT2 = .87). The higher the sum scores, the higher the levels of depression, anxiety and stress symptoms.
Positive Mental Health (PMH). PMH was assessed with the unidimensional Positive Mental Health Scale (PMH-Scale; Lukat et al., 2016). This instrument includes nine items rated on a 4-point Likert scale (e.g., “I enjoy my life”; 0 = do not agree, 3 = agree; scale reliability: αT1 = .92, αT2 = .93). Higher sum scores indicate higher levels of PMH.
Sense of Control. Following Niemeyer et al. (2019) sense of control was assessed with the two items “Do you experience important areas of your life (i.e., work, free-time, family, etc.) to be uncontrollable, meaning that you cannot, or barely can, influence them?” and “Do you experience these important areas of your life as unpredictable or inscrutable?”. Both items are rated on a 5-point Likert sale (0 = not at all, 4 = very strong; scale reliability: αT2 = .82). The higher the sum scores, the lower the sense of control.
Statistical analysesStatistical analyses were conducted using SPSS 24 and the macro Process version 2.16.1 (www.processmacro.org/index.html; Hayes, 2013). After descriptive analyses, the relationship between burden caused by the COVID-19 outbreak and the other investigated variables was assessed by zero-order bivariate correlations. Next, the predictors of the burden were assessed. First, a four-step hierarchical regression analysis was calculated that included burden as outcome. Step 1 included age (FU) and gender (FU; coded: 0 = woman, 1 = man) as control variables; PMH (BL) was included in Step 2; sense of control (FU) was added in Step 3; and depression, anxiety and stress symptoms (BL) were added in Step 4. There was no violation of the multi-collinearity assumption (all values of tolerance > .25, all variance inflation factor values < 50; Urban & Mayerl, 2006). Second, considering the results of the regression analysis, two mediation models were calculated (Process: model 4). Both models included burden caused by the COVID-19 outbreak (FU) as outcome and sense of control (FU) as mediator; age (FU) and gender (FU) were included as covariates. PMH (BL) and stress symptoms (BL) were respectively included as predictors. The basic relationship between PMH (BL) or stress symptoms (BL) and burden (FU) was denoted by c (the total effect). The relationship between PMH (BL) or stress symptoms (BL) and sense of control (FU) was denoted by path a; path b denoted the association between sense of control (FU) and burden (FU). The combined effect of path a and path b represented the indirect effect (ab). The association between PMH (BL) or stress symptoms (BL) and burden (FU) after the inclusion of sense of control (FU) in the model was denoted by path c’ (the direct effect). The bootstrapping procedure (10.000 samples) that provides accelerated confidence intervals (CI 95%) assessed the mediation effect. PM (the ratio of indirect effect to total effect) served as the mediation effect measure.
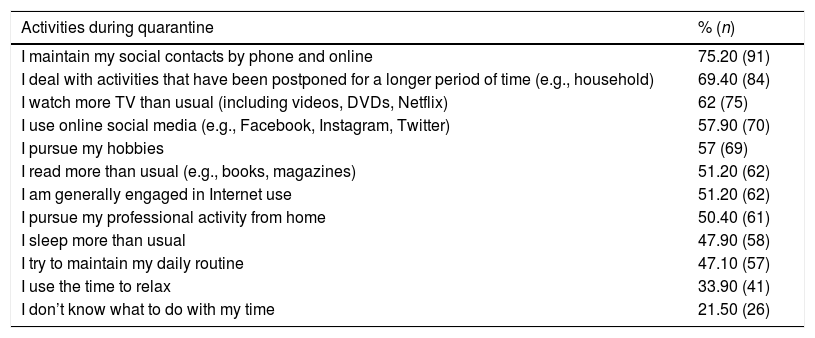
ResultsIn late March 2020, 27.80% (n = 121) of the participants were in self-quarantine on average for 5.82 days (SD = 3.91; range: 0–35). Of them 76% (n = 92) did not meet the relevant criteria (e.g., had symptoms themselves or were previously in direct contact with individuals with symptoms), but would like to reduce the risk of infection, 15.70% (n = 19) were not officially advised to quarantine, but met the relevant criteria, and 8.30% (n = 10) were officially advised to quarantine. A total of 11% (n = 48) of all participants had someone in their immediate social environment who had symptoms of COVID-19, but had not yet been tested, and 3.70% (n = 16) had someone in their immediate social environment who had been positively tested; 5% (n = 22) had symptoms of the virus themselves, but had not yet been tested, and 0.20% (n = 1) of the participants had been positively tested for COVID-19. Furthermore, 1.10% (n = 5) had someone in their immediate social environment who had been positively tested and had recovered. The mean rated usefulness of quarantine was M (SD) = 85.19 (20.08), range: 0–100. Table 1 shows the frequency of activities during the quarantine (n = 121). The most frequently indicated activity was the maintenance of social contacts by phone and online (75.20%, n = 91), followed by dealing with postponed activities (69.40%, n = 84), watching TV (62%, n = 75) and using online social media such as Facebook and Instagram (57.90%, n = 70).
Frequency of activities during quarantine (only participants in quarantine).
| Activities during quarantine | % (n) |
|---|---|
| I maintain my social contacts by phone and online | 75.20 (91) |
| I deal with activities that have been postponed for a longer period of time (e.g., household) | 69.40 (84) |
| I watch more TV than usual (including videos, DVDs, Netflix) | 62 (75) |
| I use online social media (e.g., Facebook, Instagram, Twitter) | 57.90 (70) |
| I pursue my hobbies | 57 (69) |
| I read more than usual (e.g., books, magazines) | 51.20 (62) |
| I am generally engaged in Internet use | 51.20 (62) |
| I pursue my professional activity from home | 50.40 (61) |
| I sleep more than usual | 47.90 (58) |
| I try to maintain my daily routine | 47.10 (57) |
| I use the time to relax | 33.90 (41) |
| I don’t know what to do with my time | 21.50 (26) |
Notes. n =121; multiple choices were possible.
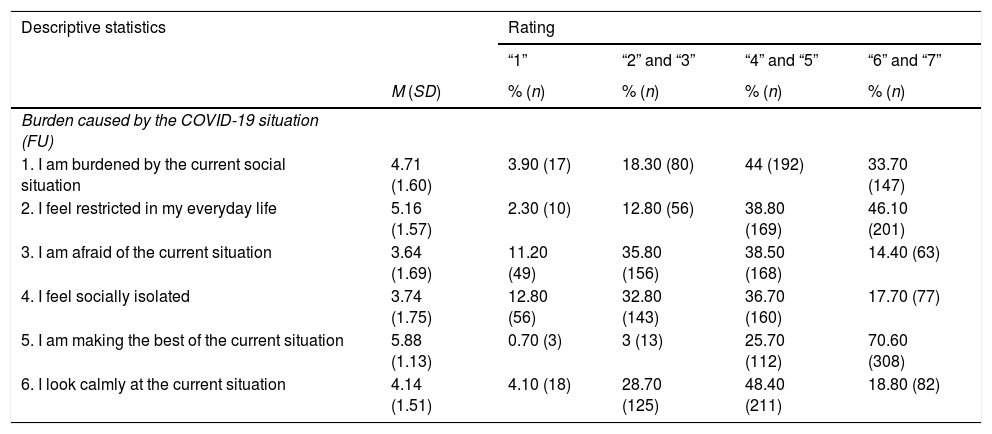
Table 2 provides an overview of the descriptive results of the single items of burden caused by the COVID-19 situation. The items “I am making the best of the current situation” and “I feel restricted in my everyday life” reached the highest means (see Table 2). The highest possible ranges (“6” and “7”) of these two items were chosen by 70.60% (n = 308; “I am making the best of the current situation”) and by 46.10% (n = 201; “I feel restricted in my everyday life”) of the participants.
Descriptive statistics of single items of burden caused by COVID-19.
| Descriptive statistics | Rating | ||||
|---|---|---|---|---|---|
| “1” | “2” and “3” | “4” and “5” | “6” and “7” | ||
| M (SD) | % (n) | % (n) | % (n) | % (n) | |
| Burden caused by the COVID-19 situation (FU) | |||||
| 1. I am burdened by the current social situation | 4.71 (1.60) | 3.90 (17) | 18.30 (80) | 44 (192) | 33.70 (147) |
| 2. I feel restricted in my everyday life | 5.16 (1.57) | 2.30 (10) | 12.80 (56) | 38.80 (169) | 46.10 (201) |
| 3. I am afraid of the current situation | 3.64 (1.69) | 11.20 (49) | 35.80 (156) | 38.50 (168) | 14.40 (63) |
| 4. I feel socially isolated | 3.74 (1.75) | 12.80 (56) | 32.80 (143) | 36.70 (160) | 17.70 (77) |
| 5. I am making the best of the current situation | 5.88 (1.13) | 0.70 (3) | 3 (13) | 25.70 (112) | 70.60 (308) |
| 6. I look calmly at the current situation | 4.14 (1.51) | 4.10 (18) | 28.70 (125) | 48.40 (211) | 18.80 (82) |
Notes. N = 436; M = Mean; SD = Standard Deviation; FU = Follow-up; Rating: “1” = I do not agree, “7” = I totally agree; COVID-19 = coronavirus disease 2019. Items 5 and 6 are reversed in the total burden score.
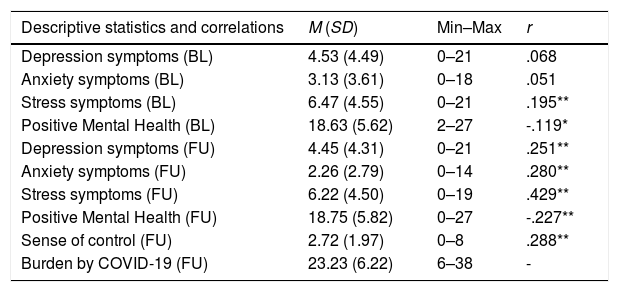
Table 3 shows the descriptive statistics of the investigated variables at both measurement time points. In addition, it presents the correlations between burden caused by the COVID-19 outbreak and the other investigated variables. Higher burden (FU) was significantly positively linked to stress symptoms at BL and FU as well as depression symptoms (FU), anxiety symptoms (FU), and sense of control (FU) (see Table 3). In contrast, PMH at both time points (BL, FU) correlated significantly negatively with burden (FU).
Descriptive statistics, correlations of burden by COVID-19 (FU) and the other investigated variables, and hierarchical regression analysis (outcome: burden by COVID-19 (FU)).
| Descriptive statistics and correlations | M (SD) | Min–Max | r |
|---|---|---|---|
| Depression symptoms (BL) | 4.53 (4.49) | 0–21 | .068 |
| Anxiety symptoms (BL) | 3.13 (3.61) | 0–18 | .051 |
| Stress symptoms (BL) | 6.47 (4.55) | 0–21 | .195** |
| Positive Mental Health (BL) | 18.63 (5.62) | 2–27 | -.119* |
| Depression symptoms (FU) | 4.45 (4.31) | 0–21 | .251** |
| Anxiety symptoms (FU) | 2.26 (2.79) | 0–14 | .280** |
| Stress symptoms (FU) | 6.22 (4.50) | 0–19 | .429** |
| Positive Mental Health (FU) | 18.75 (5.82) | 0–27 | -.227** |
| Sense of control (FU) | 2.72 (1.97) | 0–8 | .288** |
| Burden by COVID-19 (FU) | 23.23 (6.22) | 6–38 | - |
| Regression | ß | 95% CI | t | Adjusted R2 | Changes in R2 |
|---|---|---|---|---|---|
| Step 1, F (2, 433) = 5.188, p = .006 | .019 | .023 | |||
| Age (FU) | .048 | [-.044, .137] | 1.004 | ||
| Gender (FU) | -.149** | [-3.605, -.827] | -3.135 | ||
| Step 2, F (3, 432) = 6.022, p = .001 | .033 | .017 | |||
| Positive Mental Health (BL) | -.130** | [-.246, -.041] | -2.745 | ||
| Step 3, F (4, 431) = 13.435, p < .001 | .103 | .071 | |||
| Sense of control (FU) | .292** | [.613, 1.232] | 5.855 | ||
| Step 4, F (7, 428) = 9.815, p < .001 | .124 | .021 | |||
| Depression symptoms (BL) | -.108 | [-.350, .051] | -1.462 | ||
| Anxiety symptoms (BL) | -.105 | [-.391, .028] | -1.700 | ||
| Stress symptoms (BL) | .248** | [.154, .524] | 3.596 | ||
Notes. N = 436; M = Mean; SD = Standard Deviation; Min = Minimum; Max = Maximum; r = correlation; COVID-19 = coronavirus disease 2019; ß = standardized coefficient beta; CI = Confidence Interval; BL = Baseline; FU = Follow-up; in each step of the regression analysis, only new included variables are presented. **p < .01, *p < .05.
The hierarchical regression analysis revealed significant results (see Table 3). Each step provided a significant contribution to the model. Gender (FU; independent predictive variance: 2.30%), PMH (BL; independent predictive variance: 1.70%), sense of control (FU; independent predictive variance: 7.10%) and stress symptoms (BL; independent predictive variance: 2.10%) significantly predicted burden caused by the COVID-19 situation. In contrast, depression and anxiety symptoms at BL did not significantly predict burden at FU.
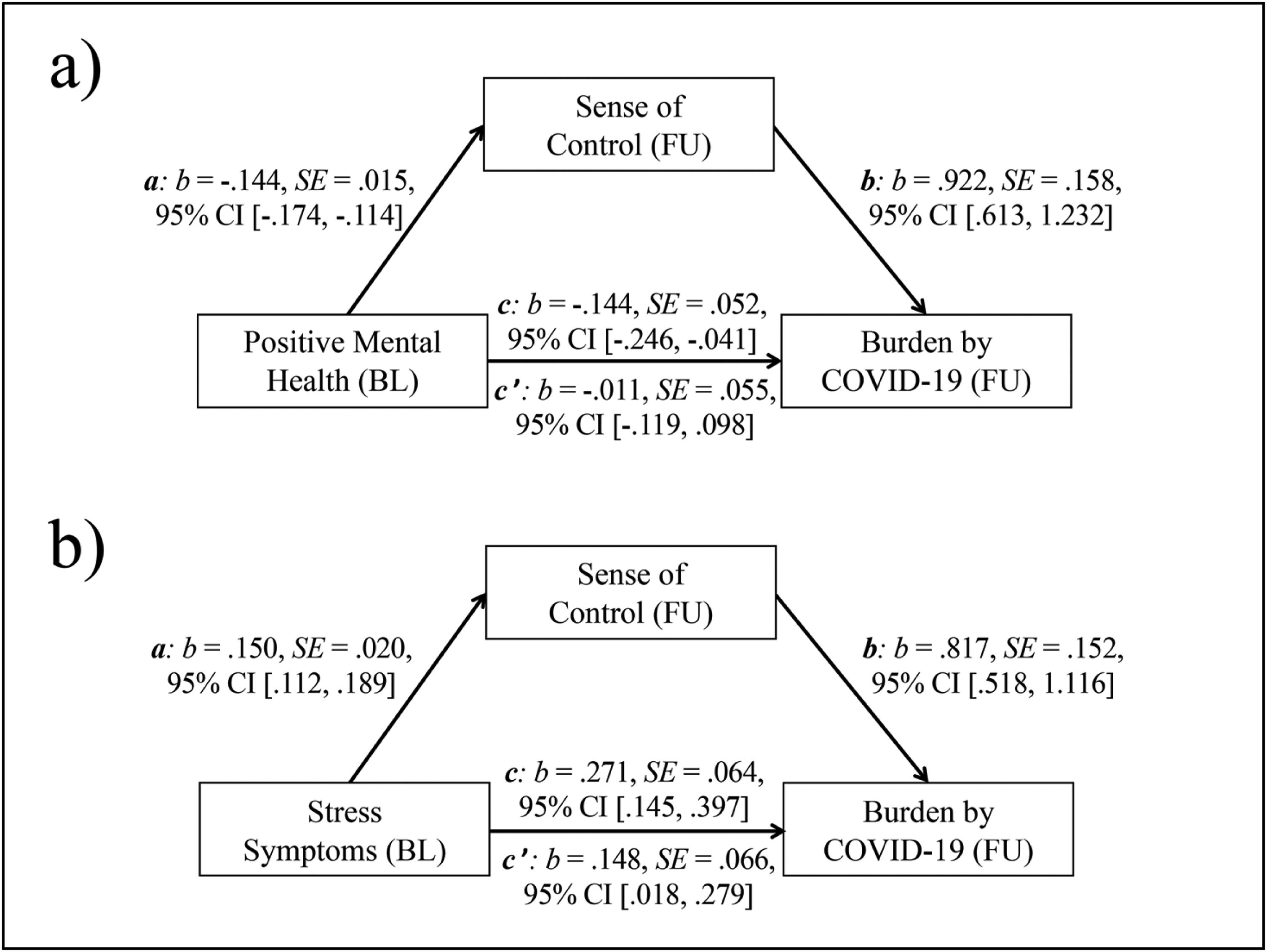
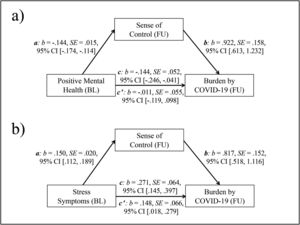
Fig. 1 presents the results of both bootstrapped mediation analyses. The results shown in Fig. 1a indicate that sense of control (FU) mediated the negative relationship between PMH (BL) and burden caused by the COVID-19 situation (FU). The basic relationship between PMH (BL) and burden (FU) was significant (total effect, c: p = .006). The link between PMH (BL) and sense of control (FU, mediator) (a: p < .001), as well as the relationship between sense of control (FU) and burden (FU) (b: p < .001) were also significant. In contrast, the relationship between PMH (BL) and burden (FU) was not significant after the inclusion of sense of control (FU) in the model (direct effect, c’: p = .848). The indirect effect (ab) was significant, b = -.133, SE = .028, 95% CI [-.193, -.083]; PM: b = .926, SE = 12.465, 95% CI [.461, 3.065].
a) Mediation model with Positive Mental Health (BL, predictor), Sense of Control (FU, mediator), and burden caused by COVID-19 (FU, outcome); b) Mediation model with Stress Symptoms (BL, predictor), Sense of Control (FU, mediator), and burden caused by COVID-19 (FU, outcome).
Note. c = total effect, c’ = direct effect; b = standardized regression coefficient; SE = Standard Error; CI = Confidence Interval; BL = Baseline; FU = Follow-up.
As shown in Fig. 1b sense of control (FU) partly mediated the positive relationship between stress symptoms (BL) and burden caused by the COVID-19 situation (FU). The basic relationship between stress symptoms (BL) and burden (FU) was significant (total effect, c: p < .001). The relationship between stress symptoms (BL) and sense of control (FU, mediator) (a: p < .001), as well as the relationship between sense of control (FU) and burden (FU) (b: p < .001) were also significant. The association between stress symptoms (BL) and burden (FU) remained significant after the inclusion of sense of control (FU) in the model (direct effect, c’: p = .026). The indirect effect (ab) was significant, b = .123, SE = .030, 95% CI [.071, .188]; PM: b = .453, SE = .177, 95% CI [.239, .866].
DiscussionSince the past several months, COVID-19 is spreading across the world. The actions taken to slow down the spread that restrict direct interpersonal contacts are reinforced almost daily. In the current absence of effective medical treatments or vaccinations, behavioral responses are particularly important and need to be understood better. The present longitudinal study provides the first findings from Germany on predictors of COVID-19 related burden.
About 20% of our participants had relevant symptoms of COVID-19 and/or someone in their immediate social environment was tested positive or had symptoms, but only one individual was tested positive for the virus. Most participants were strongly convinced that quarantine is a useful step in dealing with the spread of the virus and about one third of them was in quarantine during our data collection. To overcome the effects of physical distancing, most of the individuals who were in quarantine engaged in social interactions by phone and online. About half maintained their daily routine, pursued professional activities and caught up with postponed activities. About a fifth of the participants in quarantine seemed to be overwhelmed by the situation and did not know what to do with their time.
Descriptive analyses revealed that most participants experienced medium to high levels of burden by the current social situation (range “4” to “7”: 77.80%, n = 339) and felt restricted in their everyday lives (range “4” to “7”: 84.90%, n = 370). About a half was afraid of the current situation (range “4” to “7”: 53%, n = 231) and felt isolated (range “4” to “7”: 54.50%, n = 237). However, most participants tried to make the best of the situation (range “4” to “7”: 96.30%, n = 420) and typically looked calmly upon the crisis (range “4” to “7”: 67.20%, n = 293). Thus, it can be concluded that despite the negative experiences/emotions caused by the current COVID-19 situation, for the majority of the sample there was no enhanced tendency to excessive anxiety and hopelessness.
The investigation of the relationships of burden caused by the COVID-19 situation confirmed the necessity to consider negative as well as positive factors (e.g., Keyes, 2005; Lukat et al., 2016; Suldo & Shaffer, 2008). Positive factors seem to be of specific importance for an adaptive response (Galatzer-Levy, Huang, & Bonanno, 2018).
Stress symptoms assessed in October 2019 were a significant predictor of higher burden in March 2020 (partial confirmation of Hypothesis 1). This complements previous findings emphasizing the negative impact of stress symptoms on the reaction to uncertain situations, health and well-being (Watson & Pennebaker, 1989). Despite their cross-sectional association with burden, depression and anxiety assessed in October 2019 did not predict the level of burden longitudinally (partial rejection of Hypothesis 1). This seems to contradict earlier findings that people with higher levels of depression and anxiety tend to have stronger stress reactions in exceptionally unsafe situations (e.g., Andrews & Wilding, 2004). However, in contrast to the present work, most of the earlier studies lacked PMH, and stress symptoms were not always assessed independently of depression and anxiety. In addition, the present finding could be partly explained by the fact that the pressure for social interaction that some people with depression and anxiety experience is currently lower due to the rules on spatial distance. Those affected may thus experience at least some temporary relief (Spasojević & Alloy, 2001). Avoidance of social contact, however, is a dysfunctional strategy that yields only short-term relief, but enhances longer-term symptoms of depression and anxiety (Manz, Junge, & Margraf, 2001; Michael, Zetsche, & Margraf, 2007). Finally, the non-significant association of depression and anxiety symptoms (BL) with burden (FU) might point to a potential overestimation of the impact of negative factors on the response to uncertainty.
As expected, PMH assessed in October 2019 was identified as a predictor of lower COVID-19 related burden in March 2020 (confirmation of Hypothesis 2). This confirms earlier research showing PMH to be an important protective factor that among others reduces risk of depression, insomnia and suicide-related outcomes (Brailovskaia, Rohmann, Bierhoff, Margraf, & Köllner, 2019; Brailovskaia, Teismann, & Margraf, 2020a), moderates the association between depression symptoms and suicide ideation/behavior (Siegmann et al., 2018; Teismann, Forkmann, et al., 2018), buffers the negative impact of daily stress and fosters adaptive coping strategies (Brailovskaia et al., 2020b). Individuals with high levels of PMH perceive uncertain situations as less stressful, adjust fast to new life conditions and typically try to make the best of it (Lukat, Becker, Lavallee, van der Veld, & Margraf, 2017; Teismann, Brailovskaia, et al., 2018). PMH fosters positive emotions that contribute to the individual’s ability to bounce back from negative experiences and adversities (Fredrickson, 2013; Teismann et al., 2019). This seems to be the response to the COVID-19 situation that can be currently seen in individuals with higher levels of PMH. In contrast to depression and anxiety symptoms, PMH assessed in October 2019 was a predictor of burden in March 2020. This supports the notion that positive factors are of specific importance when predicting the response to extraordinary situations (see Galatzer-Levy et al., 2018).
Sense of control is an important factor that contributes to the positive impact of PMH and is typically missing in individuals with enhanced levels of depression, anxiety and stress (Misra & McKean, 2000; Niemeyer et al., 2019). Our results expand previous research by showing that sense of control mediates the association between stress symptoms (partly confirmation of Hypothesis 3), PMH and COVID-19 related burden (confirmation of Hypothesis 4). Thus, sense of control might foster a calmer handling of the current challenges, reduce maladaptive reactions and potential long-term negative consequences for mental health.
Despite the timeliness of the present study, the following limitations need to be considered. First, due to the highly dynamic circumstances, our findings are a snapshot of the German situation in March 2020. At this time point the exposure to the actions to slow down the spread of the virus in Germany could have been too short to produce significant levels of negative emotions and stress, particularly in mentally healthy individuals. Studies in other countries and at later time points after the outbreak of COVID-19 are necessary to assess the generalizability of our results. Second, the current data collection took place ad-hoc in order to elucidate the acute response. Therefore, it was not possible to assess all variables at both measurement time points. The measurement of sense of control at baseline would improve the predictive power of the mediation models. Third, despite the given variance of age and occupation, the mostly female, on average rather young and well-educated composition of the investigated sample does not represent the general population. This limits the generalizability of current findings. Thus, replication in a more representative sample is desirable. Moreover, while in the present study, mentally healthy individuals were investigated, future studies are suggested to specially focus on clinical patients who might be at elevated risk for the experience of burden caused by COVID-19 outbreak. Fourth, PMH is only one of many positive factors that may confer resilience (Bonanno et al., 2010). Therefore, future studies should include additional positive factors such as life satisfaction (e.g., Diener & Diener, 1995), subjective happiness (e.g., Lyubomirsky & Lepper, 1999), and positive well-being (e.g., Ryff, 1989). Fifth, the effect sizes of the present results are rather small and therefore should be considered with caution.
To sum up, the present study reveals first findings of the psychological impact of the extraordinary situation caused by COVID-19 in Germany. Although our participants show a significant degree of burden, many of them try to make the best of the situation without becoming anxious and hopeless. Remarkably, the response to the current situation is predicted by PMH and stress symptoms, but not by depression and anxiety symptoms. Finally, sense of control seems to contribute to an adequate response.
FundingThe DFG Open Access Publication Funds of the Ruhr-Universität Bochum provided financial support for the publication of the present study.
We acknowledge support by the DFG Open Access Publication Funds of the Ruhr-Universität Bochum. We thank Dr. Mar Rus-Calafell for supporting us with the preparation of the Spanish language version of the paper.