The goal of this study is to establish a Chinese version of the End-of-Life Decision Making and Associated Staff Stress Questionnaire to assess its reliability and validity.
MethodA sample of 119 Intensive Care Unit physicians and 485 nurses in China completed the questionnaire, along with questionnaires assessing motional exhaustion subscale, Stress Overload Scale, and other variables associated with end-of-life decision.
ResultsSeven factors obtained via exploratory factor analysis could explain 70.61% of the total variance. Confirmatory factor analysis demonstrated an acceptable model fit with Root Mean Square Error of Approximation (RMSEA) being .078 and Standardized Root Mean Square Residual (SRMR) being .066. Validity evidence based on relationships with other variables was provided by positive or negative correlations between the questionnaire subscales and emotional exhaustion, stress overload, and other variables associated with end-of-life decision. The average content validity index was .96. The Cronbach’s α and test–retest reliability was outstanding.
ConclusionsThe Chinese version of the End-of-Life Decision Making and Associated Staff Stress Questionnaire is a reliable and valid instrument for measuring the facilitators and hinders to facilitate the end-of-life decision-making, communication and the associated pressure perceived by relevant Intensive Care Unit medical staff among the Chinese population.
El objetivo de este estudio es obtener una versión china del End-of-Life Decision Making and Associated Staff Stress Questionnaire.
MétodoUna muestra de 119 médicos de la Unidad de Cuidados Intensivos y 485 enfermeras chinas completaron el cuestionario, junto con cuestionarios para evaluar el agotamiento por movimiento, la sobrecarga de estrés y otras variables asociadas con la decisión del final del la vida.
ResultadosSiete factores obtenidos a través del análisis factorial exploratorio explican el 70,61% de la varianza total. El análisis factorial confirmatorio mostró un modelo de cuatro factores con ajuste satisfactorio (RMSEA = .078; SRMR = .066). Las evidencias de validez basadas en las relaciones con otras variables fue demostrada por correlaciones con agotamiento emocional, sobrecarga de estrés y otras variables asociadas con la decisión de fin de la vida. El índice de validez de contenido promedio fue de 0,96. Los coeficientes de fiabilidad de consistencia interna y test-retest fueron buenos.
ConclusionesSe trata de un instrumento que aporta medidas fiables y válidas para la percepción del fin de la vida por el personal médico chino de las unidades de cuidados intensivos.
End-of-life (EOL) decisions, that is, decisions about treatment and care at the end of a patient's life, usually occur before death and are a sign of a shift from active treatment to palliative care. EOL decisions mainly involve do-not-resuscitate order, life-sustaining treatment, death attitude, death location, and the patient self-determination act (Zhou et al., 2016). The Intensive Care Unit (ICU) caters to the centralized treatment of critically ill patients and records the highest mortality rate in hospitals, where ICU medical staffs often have to make decisions about limiting or withdrawing life-sustaining treatment. The internationally recommended EOL decision-making model is decision sharing; namely, doctors and patients jointly develop treatment plans according to the patient’s personal wishes or the reasonable requirements of their families. For patients who are approaching EOL, we should respect their needs, limit or withdraw life-sustaining therapy, save medical resources, and improve EOL quality (Nelson et al., 2011).
In clinical practice, the actual condition of a patient with a severe health problem is difficult to be assessed on the basis of the concept of dying, that is, chance of survival. Each person’s cognition is influenced by his social and professional status, and thus, people’s perspective of dying can vary. Physicians play the main role in or are usually dictators of EOL decision-making, but their decisions are anchored more on the needs of disease treatment and less on the emotional needs of patients and their families (Patel & Ackermann, 2016). By contrast, nurses spend much time around patients and can thus assess firsthand the effectiveness of treatment and sense the actual situation and suffering of patients. EOL decisions in the ICU emphasize the combined role of multidisciplinary teams comprising doctors, nurses, patients and their families. However, physicians rarely seek the opinions of nurses when making decisions due to their different responsibilities, and opinions from nurses are often not valued or are even neglected (Dombrecht et al., 2020). Communication and collaboration between doctors and nurses are obviously lacking (Holms, Milligan, & Kidd, 2014) in real-life practice. Puntillo and McAdam (2006) called this phenomenon “the doctor is from Mars and the nurse is from Mercury.” The presentation of this statement also intuitively reflects the serious barriers to communication and collaboration between health care providers. Burnout is a syndrome of excessive physical and mental exhaustion caused by long-term work stress, which is closely related to the satisfaction of patients, the turnover rate among medical staff, and the quality and safety of medical care (Chuang et al., 2016). In the current complex medical environment, ICU medical staff is under tremendous pressure and faces the risk of burnout. Among the many factors, ethical conflicts that limit or withdraw life-sustaining treatment are most critical because of the resulting emotional exhaustion in the dimension of burnout (Jensen, Ammentorp, Johannessen, & Ording, 2013; Malaquin et al., 2017; Teixeira, Ribeiro, Fonseca, & Carvalho, 2014).
Evaluation tools for hospice attitudes are widely studied, but no recognized and established tools have been found for EOL decision-making and communication. Some questionnaires are limited to single-dimensional measurements (Beckstrand & Kirchhoff, 2005). Most questionnaires have no rigorous theoretical framework, and lack reliability and validity tests (Jox et al., 2010; Latour, Fulbrook, & Albarran, 2009). Multiple dimensions can be measured by few scales (Hansen, Goodell, DeHaven, & Smith, 2009; Kinoshita & Miyashita, 2011), which can provide some psychometric characteristics; however, these scales focus on hospice care provided by nurses with minimal involvement in EOL decision making or communication. Daniel Schwarzkopf developed the End-of-Life Decision-Making and Staff Stress (EIDECS) questionnaire for effective EOL decision making and communication (Schwarzkopf et al., 2015). A theory-driven approach, which is based on expert opinion on EOL decision making and communication (Nelson et al., 2011) and also theories from the field of work psychology (Frese & Zapf, 1994), was used to select the domains. The theoretical foundation of the questionnaire can be divided into three domains as follows: “domain A: promoting and hindering factors”, “domain B: pressure level” and “domain C: active behavior”. In detail, domain A is comprised of collaboration in the EOL context, role clarity in the EOL context, work-related interruptions of communication with families and emotional support. Domain B includes stress by involvement in EOL decision making and communication with families and stress by work overload. The component “initiative EOL decision making” belongs to domain C. EIDECS has been widely used in some countries because of its good psychometric indicators. As it potentially provide effective and reliable evaluation tools for ICU EOL decision-making research. Therefore, the present study aims to perform cross-cultural adaptation to test the reliability and validity of the Chinese version of the EIDECS (C-EIDECS) questionnaire. It also seeks to provide an effective assessment tool for ICU managers to evaluate the barriers and facilitators to EOL decision-making. The results are expected to provide a reference for further intervention measures and process development.
In 2014, the European Commission issued the Guidelines for EOL Medical Decision Procedures to provide principled advice and assistance to people who are struggling with medical decisions for dying patients from a legal and ethical perspective. EOL medical treatment is a worldwide problem in terms of various moral and legal issues (Bossaert et al., 2015).
A recent study found that most doctors and nurses are satisfied with the conduct of medical treatment but that they are quite unsatisfied with the communication and collaboration between them (Bluemel, Traweger, Kinzl, Baubin, & Lederer, 2011). An ideal hospice environment requires nurses to spend much time with patients and their families. Such a situation requires effective communication among health care providers, patients, and patients’ families. A large number of previous studies (Flannery, Ramjan, & Peters, 2016; Gallagher et al., 2015; Paganini & Bousso, 2015) have confirmed the important role of ICU nurses in EOL decision- making.
Although the roles and responsibilities of nurses may vary among different cultural backgrounds, they should actively participate in EOL decisions. Particularly, nurses with rich clinical experience pay attention to the needs and pain of patients and their families and prompt physicians to initiate EOL decisions in a timely manner so as to create a standardized approach and provide optimal EOL care (Bucher et al., 2018). However, nurses also could have different attitudes toward EOL decision-making. Some nurses are willing to participate in this process, whereas others are reluctant to do so because of the emotional burden involved and prefer to leave the decision-making to physicians (Velarde-García, Pullido-Mendoza, Moro-Tejedor, Cachón-Pérez, & Palacios-Ceña, 2016). No structured policy dictates who should participate in hospice care, and this deficiency leads to a lack of unity and the ambiguity of the roles of nurses in EOL decision making.
For family members, a lack of communication and cooperation leads to misunderstanding of treatment plans and distrust of doctors, resulting in guilt, anxiety, depression, and other negative emotions. For medical staff, a lack of communication and cooperation leads to increased occupational stress, frustration, resentment, and dissatisfaction, all of which affect the quality of medical treatment. The research by Schwarzkopf et al. (2017) revealed that ineffective medical care perceived by ICU medical staff is positively correlated with burnout, resulting in increased anxiety to leave. Poor work conditions, the amount of workload and collaboration with other departments are considered as predictors of perceived ineffective care, emotional exhaustion, and turnover intentions. Therefore, we should take active measures to improve communication and cooperation between ICU hospice patients and health care providers. Moreover, EOL decisions should be smoothly implemented, the quality of hospice care should be improved. The cooperation awareness of medical staff also requires enhancement, along with the strengthening of multidisciplinary cooperation and reduction of medical staff stress and burnout. These measures will alleviate the gap between medical resources and social needs and reduce the uneven and unreasonable distribution of resources.
MethodTranslation and cross-cultural adaptationThe adaptation of the EIDECS questionnaire was authorized by the author of the original English version. The process of translation and cross-cultural adaptation followed the recommended procedures for questionnaire translation (Beaton, Bombardier, Guillemin, & Ferranz, 2000).
Step 1: Initial translation. The original English version of EIDECS was translated into Chinese independently by two bilingual native Chinese-speaking translators with different educational and job profiles.
Step 2: Synthesis of translations. Their translations were then synthesized to form a questionnaire by a third translator after all the discrepancies between the two were addressed.
Step 3: Back translation. The initial Chinese version was back translated by two bilingual professors whose first language is English. Notably, the back translators had never seen the original version of the questionnaire before.
Step 4: Expert committee review. All materials in the translation process were submitted to the expert committee, which suggested solutions to the problems in the translation process, reviewed the guidance of the questionnaire, and unified differences in the translation process. The expert committee consisted of six members, including one ICU doctor, two critical care managers, one clinical nurse (with over 10 years of ICU experience), and one psychologist. The prefinal Chinese version with conceptual equivalence to the original version was developed.
Step 5: Test of the prefinal version. The prefinal version was field tested using a convenience sample of 20 ICU nurses and 20 ICU physicians to determine the comprehensiveness of the Chinese version, none of whom identified any necessary modification. After field testing, all questions were discussed by the researchers and group of experts as mentioned above. No special concepts or semantic differences were found during the process. The finalized version renamed as C-EIDECS was then subjected to psychometric testing among medical staff.
ParticipantsWe recruited six comprehensive tertiary hospitals in Southern China from June to July in 2019 according to the convenience principle. The inclusion criteria for nurses and physicians were as follows: (1) registered ICU nurses and physicians who have specializations in medical, surgical, emergency, or other relevant fields; (2) one-year work experience in a department; and (3) gave informed consent to participate in this study. Exclusion criteria: nurses or physicians who are internships, under advanced studies, and taking rotations in the surveyed departments.
A total of 620 questionnaires were collected, 16 out of them were considered invalid with all items having the same answer and were thus eliminated. Hence, 604 subjects, including 119 physicians and 485 nurses, were retained for an analysis, which corresponds to a response rate of 97.40%. Among the types of ICUs surveyed, comprehensive ICUs accounted for more than half (56%). The majority of the respondents were under 30 years old. The nurses were more often female (p < .001) and had more years of job experience (p < .05) than the physicians. Only a small minority (6.50%) of the participants had more than 15 years of ICU experience.
InstrumentsGeneral Information Collection Form. The form was supplemented by the researchers according to the study objectives. It included ICU type, gender, age, occupation, years of experience in ICU, participation in EOL decision making during last 7 days, satisfaction with EOL decisions and satisfaction with EOL communication (Jox et al., 2010). Satisfaction is rated on a 4-point scale (1 = very dissatisfied, 2 = dissatisfied, 3 = satisfied, and 4 = very satisfied). There is a hypothesis that respondents who have participated in EOL decision making and were satisfied with decision making and communication will give better scores in all areas of the investigation. An item indicating participation in an EOL decision was used to measure whether staff members actually showed a tendency to involve themselves in EOL decisions.
Pilot survey of C-EIDECS questionnaire. This questionnaire contains 26 items and seven factors: collaboration in the EOL context (6 items), role clarity in the EOL context (6 items), work-related interruptions of communication with families (2 items), emotional support (3 items), stress by involvement in EOL decision making and communication with families (5 items), stress by work overload (2 items), and taking initiative toward EOL decision making (2 items). Each item was measured using a five-point Likert scale ranging from “strongly disagree” to “strongly agree” or from “not stressful” to “very stressful.” The questionnaire measured the relevant situation for nearly a week.
Chinese version of Stress Overload Scale (SOS; Amirkhan, 2012; Su & Guo, 2014). The SOS is a 22-item tool consisting of two dimensions, namely, event load (10 items) and individual vulnerability (12 items). The scale reflects the stress perception of the past month. It uses a five-point Likert scale to indicate respondents’ stress. A high total score indicates a high stress load. The internal consistency (Cronbach’s α ranged from .89 to .93) was good. The total variance explained was 54.05%. Split-half reliability was .85, test–retest reliability was .71-.80, and overall content validity index was .86. The scale was used to verify the structural validity of the questionnaire.
Emotional Exhaustion subscale. The subscale was taken from the Maslach Burnout Inventory (MBI; Hua, 2007). It consists of nine items that assess emotional responses to work stress. With a total score of 54, a higher value indicates higher degree of burnout. Each item was scored on a seven-point Likert scale (from 0 = never happened to 6 = every day). Cronbach’s α was .77 and test–retest reliability was .80. This subscale was used to examine the correlation with the C-EIDECS questionnaire.
ProcedureWe conducted a multicenter joint research through the WeChat platform. First, with the permission of the ethics committee of six hospitals, the uniformly trained data collection personnel detailed the purpose of the survey, method of questionnaire filling, and confidentiality of the survey. Then, they issued a two-dimensional code of the questionnaire after obtaining the informed consent of the participants. The duration of filling in the questionnaire was approximately 10-15 min, and the questionnaire was submitted immediately after completion. The questionnaire was deemed ineffective if the filling in process was interrupted, repeated, or omitted.
Data analysisIBM SPSS 23.0 and AMOS 23.0 software were used for the statistical analyses of the data. Descriptive statistics were generated for each item score and the demographic data. The Exploratory Factor Analysis (EFA) was performed using unweighted least Squares (ULS) and Direct Oblimin rotation enforcing seven-factor solution. Confirmatory Factor Analysis (CFA) was conducted by Maximum Likelihood (ML). Since each index provides information about different aspects of model fit, a number of statistics are used to evaluate the model fit: chi-square–degree of freedom ratio (χ2/df), Root Mean Square Error of Approximation (RMSEA), Tucker-Lewis Index (TLI), Comparative Fit Index (CFI) and Standardized Root Mean Square Residual (SRMR). Acceptable model fit (Hu & Bentler, 1999; Wu, 2010) was defined as χ2/df < 3, RMSEA < .08, TLI > .90, CFI > .95 and SRMR < .08. Validity evidence based on relationships with other variables was obtained by calculating correlations between scores on the subscales of C-EIDECS and occupation, participation in EOL decision making, satisfaction in EOL decision-making and communication, emotional exhaustion and SOS. The scale content validity index (S-CVI) and item content validity index (I-CVI) were used to evaluate the content validity of the questionnaire. Reliability was measured using internal consistency reliability (Cronbach's alpha) and test-retest reliability (intra-class correlation coefficient, ICC). The values of ICC between .75 and .90 are indicative of good reliability (Koo & Li, 2016). An item analysis was also performed by calculating corrected item-total correlation coefficients.
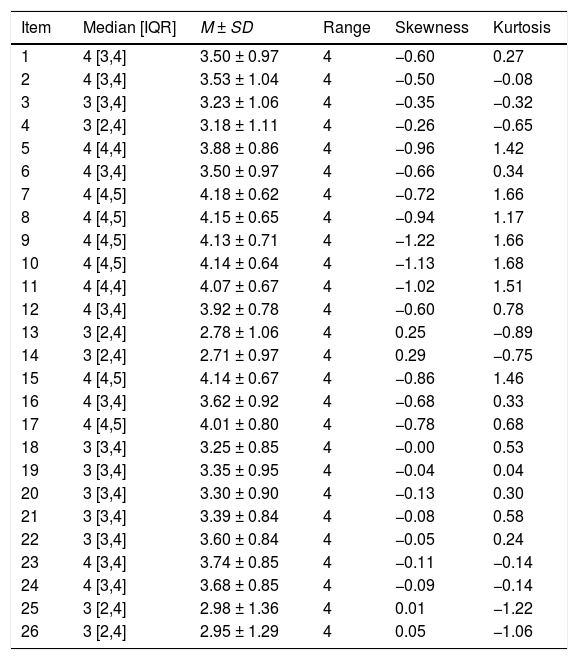
ResultsDescriptive analyses of the items on the C-EIDECS questionnaireThe items were checked for skewness and kurtosis that are shown in Table 1, together with the median [interquartile range, IQR], mean scores (M) and standard deviations (SD). We concluded that the C-EIDECS item distributions had a skewness range between −1.22 and 0.29 and a kurtosis range between −1.22 and 1.68. Based on the result of Kolmogorov-Smirnov test (p < .001) and Q-Q plot, a small number of items score exhibited a non-normal distribution.
Descriptive statistics of C-EIDECS questionnaire items.
| Item | Median [IQR] | M ± SD | Range | Skewness | Kurtosis |
|---|---|---|---|---|---|
| 1 | 4 [3,4] | 3.50 ± 0.97 | 4 | −0.60 | 0.27 |
| 2 | 4 [3,4] | 3.53 ± 1.04 | 4 | −0.50 | −0.08 |
| 3 | 3 [3,4] | 3.23 ± 1.06 | 4 | −0.35 | −0.32 |
| 4 | 3 [2,4] | 3.18 ± 1.11 | 4 | −0.26 | −0.65 |
| 5 | 4 [4,4] | 3.88 ± 0.86 | 4 | −0.96 | 1.42 |
| 6 | 4 [3,4] | 3.50 ± 0.97 | 4 | −0.66 | 0.34 |
| 7 | 4 [4,5] | 4.18 ± 0.62 | 4 | −0.72 | 1.66 |
| 8 | 4 [4,5] | 4.15 ± 0.65 | 4 | −0.94 | 1.17 |
| 9 | 4 [4,5] | 4.13 ± 0.71 | 4 | −1.22 | 1.66 |
| 10 | 4 [4,5] | 4.14 ± 0.64 | 4 | −1.13 | 1.68 |
| 11 | 4 [4,4] | 4.07 ± 0.67 | 4 | −1.02 | 1.51 |
| 12 | 4 [3,4] | 3.92 ± 0.78 | 4 | −0.60 | 0.78 |
| 13 | 3 [2,4] | 2.78 ± 1.06 | 4 | 0.25 | −0.89 |
| 14 | 3 [2,4] | 2.71 ± 0.97 | 4 | 0.29 | −0.75 |
| 15 | 4 [4,5] | 4.14 ± 0.67 | 4 | −0.86 | 1.46 |
| 16 | 4 [3,4] | 3.62 ± 0.92 | 4 | −0.68 | 0.33 |
| 17 | 4 [4,5] | 4.01 ± 0.80 | 4 | −0.78 | 0.68 |
| 18 | 3 [3,4] | 3.25 ± 0.85 | 4 | −0.00 | 0.53 |
| 19 | 3 [3,4] | 3.35 ± 0.95 | 4 | −0.04 | 0.04 |
| 20 | 3 [3,4] | 3.30 ± 0.90 | 4 | −0.13 | 0.30 |
| 21 | 3 [3,4] | 3.39 ± 0.84 | 4 | −0.08 | 0.58 |
| 22 | 3 [3,4] | 3.60 ± 0.84 | 4 | −0.05 | 0.24 |
| 23 | 4 [3,4] | 3.74 ± 0.85 | 4 | −0.11 | −0.14 |
| 24 | 4 [3,4] | 3.68 ± 0.85 | 4 | −0.09 | −0.14 |
| 25 | 3 [2,4] | 2.98 ± 1.36 | 4 | 0.01 | −1.22 |
| 26 | 3 [2,4] | 2.95 ± 1.29 | 4 | 0.05 | −1.06 |
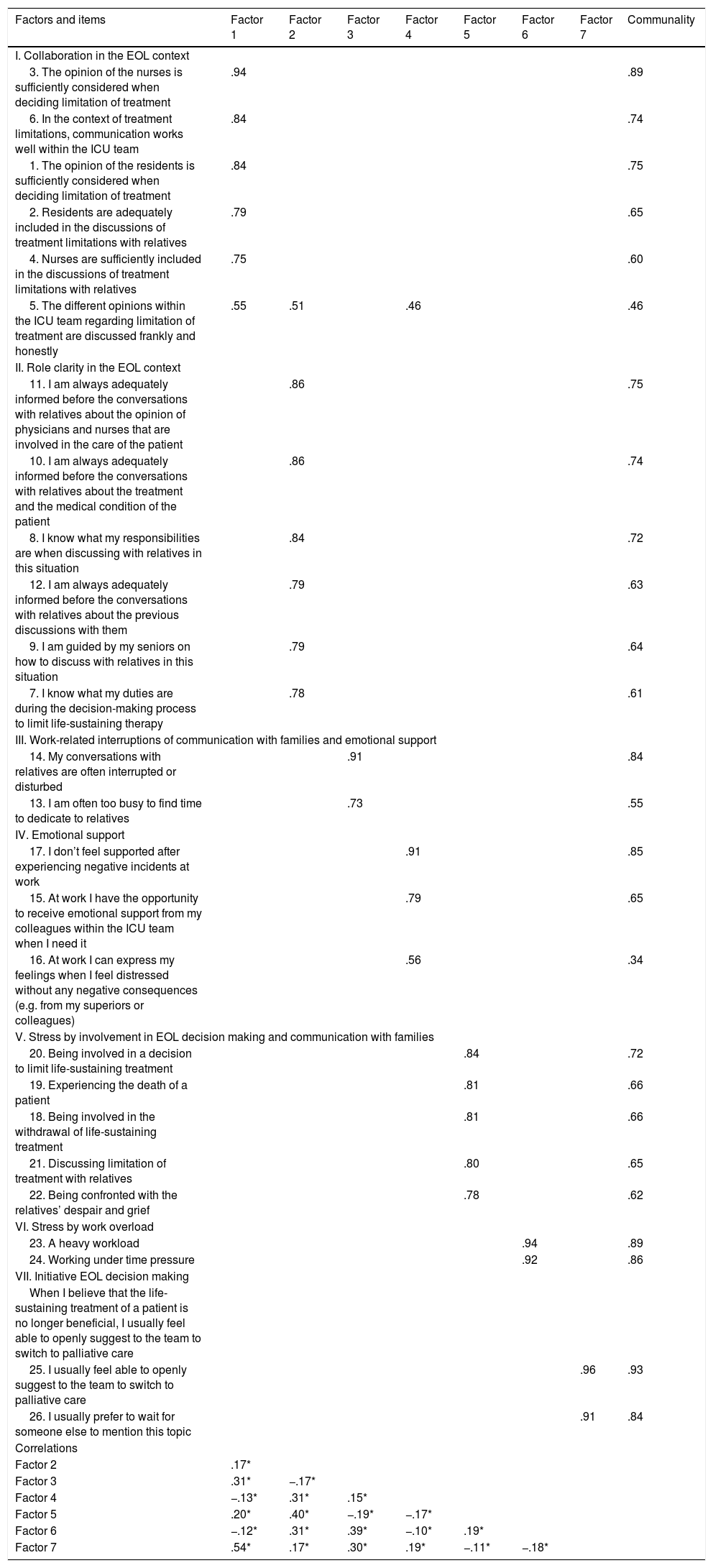
In order to keep the potential structure of the revised questionnaire to be the same or similar to that of the original questionnaire, so as to conform to the original theoretical framework of the questionnaire, the original seven-factor model found in Schwarzkopf et al. (2015) was tested first to see if the results hold for the Chinese sample. We conducted the EFA using a priori criterion with the whole sample (N = 604). Results of the Kaiser-Meyer-Olkin Measure of Sampling Adequacy test and the Bartlett test of sphericity indicated that the data was suitable for factor analysis (KMO = .84; Bartlett = 11266.062, p < .001) (Wu, 2010). Additionally, a scree plot of the eigenvalues and Parallel analysis both recommended a seven-factor solution. Table 2 shows the factor loading of each item ranged between .55 and .94 (>.40), and the communality ranged between .34 and .93 (>.30), indicating adequately value of the factor extraction. All items loaded on their expected factors excepted for item 5, which had co-loadings on factor 1, factor 2 and factor 4. Furthermore, the difference of loading value was less than .20. Nevertheless, according to the practical significance and experts' opinions, the attribution of item 5 to factor 1 was consistent with the theoretical foundation of the original questionnaire. Consequently, the original factor names were kept unchanged. The factors correlation coefficients vary from −.19∼.54.
Exploratory Factorial Analysis of Structure matrix (N = 604).
| Factors and items | Factor 1 | Factor 2 | Factor 3 | Factor 4 | Factor 5 | Factor 6 | Factor 7 | Communality |
|---|---|---|---|---|---|---|---|---|
| I. Collaboration in the EOL context | ||||||||
| 3. The opinion of the nurses is sufficiently considered when deciding limitation of treatment | .94 | .89 | ||||||
| 6. In the context of treatment limitations, communication works well within the ICU team | .84 | .74 | ||||||
| 1. The opinion of the residents is sufficiently considered when deciding limitation of treatment | .84 | .75 | ||||||
| 2. Residents are adequately included in the discussions of treatment limitations with relatives | .79 | .65 | ||||||
| 4. Nurses are sufficiently included in the discussions of treatment limitations with relatives | .75 | .60 | ||||||
| 5. The different opinions within the ICU team regarding limitation of treatment are discussed frankly and honestly | .55 | .51 | .46 | .46 | ||||
| II. Role clarity in the EOL context | ||||||||
| 11. I am always adequately informed before the conversations with relatives about the opinion of physicians and nurses that are involved in the care of the patient | .86 | .75 | ||||||
| 10. I am always adequately informed before the conversations with relatives about the treatment and the medical condition of the patient | .86 | .74 | ||||||
| 8. I know what my responsibilities are when discussing with relatives in this situation | .84 | .72 | ||||||
| 12. I am always adequately informed before the conversations with relatives about the previous discussions with them | .79 | .63 | ||||||
| 9. I am guided by my seniors on how to discuss with relatives in this situation | .79 | .64 | ||||||
| 7. I know what my duties are during the decision-making process to limit life-sustaining therapy | .78 | .61 | ||||||
| III. Work-related interruptions of communication with families and emotional support | ||||||||
| 14. My conversations with relatives are often interrupted or disturbed | .91 | .84 | ||||||
| 13. I am often too busy to find time to dedicate to relatives | .73 | .55 | ||||||
| IV. Emotional support | ||||||||
| 17. I don’t feel supported after experiencing negative incidents at work | .91 | .85 | ||||||
| 15. At work I have the opportunity to receive emotional support from my colleagues within the ICU team when I need it | .79 | .65 | ||||||
| 16. At work I can express my feelings when I feel distressed without any negative consequences (e.g. from my superiors or colleagues) | .56 | .34 | ||||||
| V. Stress by involvement in EOL decision making and communication with families | ||||||||
| 20. Being involved in a decision to limit life-sustaining treatment | .84 | .72 | ||||||
| 19. Experiencing the death of a patient | .81 | .66 | ||||||
| 18. Being involved in the withdrawal of life-sustaining treatment | .81 | .66 | ||||||
| 21. Discussing limitation of treatment with relatives | .80 | .65 | ||||||
| 22. Being confronted with the relatives’ despair and grief | .78 | .62 | ||||||
| VI. Stress by work overload | ||||||||
| 23. A heavy workload | .94 | .89 | ||||||
| 24. Working under time pressure | .92 | .86 | ||||||
| VII. Initiative EOL decision making | ||||||||
| When I believe that the life-sustaining treatment of a patient is no longer beneficial, I usually feel able to openly suggest to the team to switch to palliative care | ||||||||
| 25. I usually feel able to openly suggest to the team to switch to palliative care | .96 | .93 | ||||||
| 26. I usually prefer to wait for someone else to mention this topic | .91 | .84 | ||||||
| Correlations | ||||||||
| Factor 2 | .17* | |||||||
| Factor 3 | .31* | −.17* | ||||||
| Factor 4 | −.13* | .31* | .15* | |||||
| Factor 5 | .20* | .40* | −.19* | −.17* | ||||
| Factor 6 | −.12* | .31* | .39* | −.10* | .19* | |||
| Factor 7 | .54* | .17* | .30* | .19* | −.11* | −.18* | ||
Note: Factor loadings |.40| were omitted.
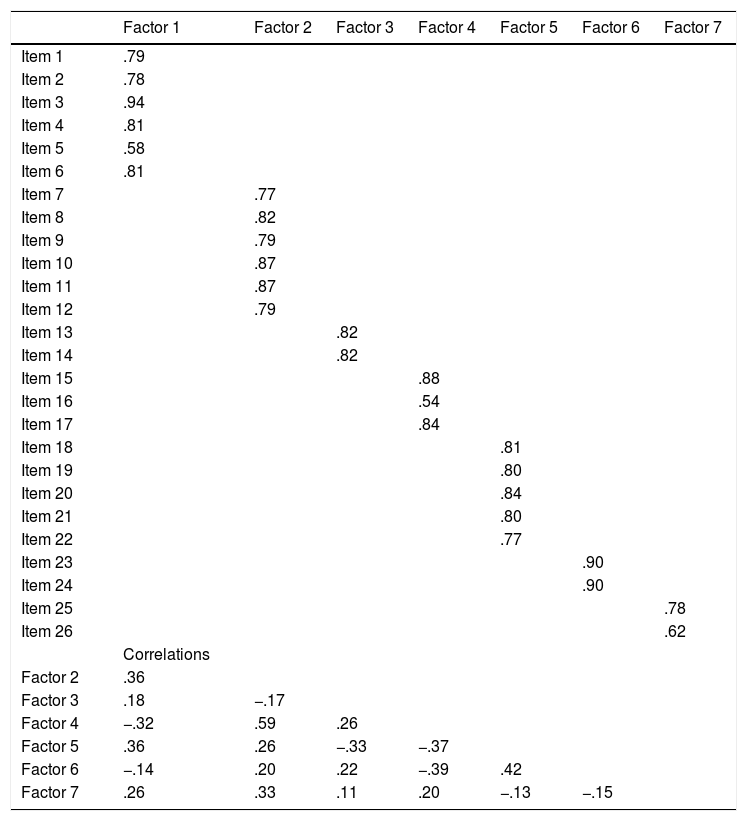
ML estimation was recommended when the variables do not deviate too much from normality (Kline, 2011; Senín-Calderón, Perona-Garcelán, Ruiz-Veguilla, & Rodríguez-Testal, 2017). The values for skewness and kurtosis were deemed to be within the range for ML. To further verify the rationality of the seven-factor structure, we performed CFA with ML method (N = 604). The results demonstrated that the model had fair fit (χ2/df = 4.715, RMSEA = .078, TLI = .891, CFI = .907, and SRMR = .066). The factor loadings between the items and their latent variables were .540∼.945 (Table 3). The correlations between factors varied from −.39 to .59.
Standardized factor loadings and factor correlations of confirmatory factor analysis.
| Factor 1 | Factor 2 | Factor 3 | Factor 4 | Factor 5 | Factor 6 | Factor 7 | |
|---|---|---|---|---|---|---|---|
| Item 1 | .79 | ||||||
| Item 2 | .78 | ||||||
| Item 3 | .94 | ||||||
| Item 4 | .81 | ||||||
| Item 5 | .58 | ||||||
| Item 6 | .81 | ||||||
| Item 7 | .77 | ||||||
| Item 8 | .82 | ||||||
| Item 9 | .79 | ||||||
| Item 10 | .87 | ||||||
| Item 11 | .87 | ||||||
| Item 12 | .79 | ||||||
| Item 13 | .82 | ||||||
| Item 14 | .82 | ||||||
| Item 15 | .88 | ||||||
| Item 16 | .54 | ||||||
| Item 17 | .84 | ||||||
| Item 18 | .81 | ||||||
| Item 19 | .80 | ||||||
| Item 20 | .84 | ||||||
| Item 21 | .80 | ||||||
| Item 22 | .77 | ||||||
| Item 23 | .90 | ||||||
| Item 24 | .90 | ||||||
| Item 25 | .78 | ||||||
| Item 26 | .62 | ||||||
| Correlations | |||||||
| Factor 2 | .36 | ||||||
| Factor 3 | .18 | −.17 | |||||
| Factor 4 | −.32 | .59 | .26 | ||||
| Factor 5 | .36 | .26 | −.33 | −.37 | |||
| Factor 6 | −.14 | .20 | .22 | −.39 | .42 | ||
| Factor 7 | .26 | .33 | .11 | .20 | −.13 | −.15 |
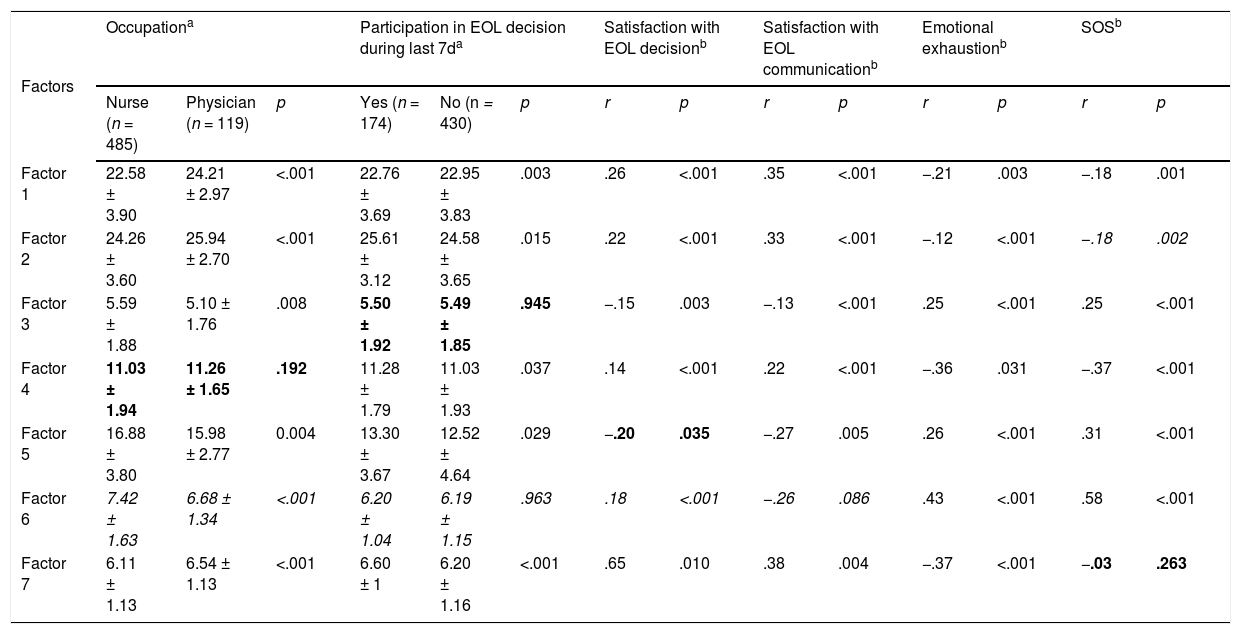
Results of analysis to determine the construct validity of the C-EIDECS questionnaire were shown in Table 4. It reveals that the nurses performed a more negative evaluation of almost all subscales than physicians as expected. Staff who recently participated in EOL decision making and were satisfied with EOL decision and communication gave a more positive rating. Overall, in addition to five variables of no hypothesis theory (marked as italics in table), only four of the 37 hypothetical relationships failed to reach statistical significance (marked as bold in table).
Correlation between factors of C-EIDECS and other variables.
| Factors | Occupationa | Participation in EOL decision during last 7da | Satisfaction with EOL decisionb | Satisfaction with EOL communicationb | Emotional exhaustionb | SOSb | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Nurse (n = 485) | Physician (n = 119) | p | Yes (n = 174) | No (n = 430) | p | r | p | r | p | r | p | r | p | |
| Factor 1 | 22.58 ± 3.90 | 24.21 ± 2.97 | <.001 | 22.76 ± 3.69 | 22.95 ± 3.83 | .003 | .26 | <.001 | .35 | <.001 | −.21 | .003 | −.18 | .001 |
| Factor 2 | 24.26 ± 3.60 | 25.94 ± 2.70 | <.001 | 25.61 ± 3.12 | 24.58 ± 3.65 | .015 | .22 | <.001 | .33 | <.001 | −.12 | <.001 | −.18 | .002 |
| Factor 3 | 5.59 ± 1.88 | 5.10 ± 1.76 | .008 | 5.50 ± 1.92 | 5.49 ± 1.85 | .945 | −.15 | .003 | −.13 | <.001 | .25 | <.001 | .25 | <.001 |
| Factor 4 | 11.03 ± 1.94 | 11.26 ± 1.65 | .192 | 11.28 ± 1.79 | 11.03 ± 1.93 | .037 | .14 | <.001 | .22 | <.001 | −.36 | .031 | −.37 | <.001 |
| Factor 5 | 16.88 ± 3.80 | 15.98 ± 2.77 | 0.004 | 13.30 ± 3.67 | 12.52 ± 4.64 | .029 | −.20 | .035 | −.27 | .005 | .26 | <.001 | .31 | <.001 |
| Factor 6 | 7.42 ± 1.63 | 6.68 ± 1.34 | <.001 | 6.20 ± 1.04 | 6.19 ± 1.15 | .963 | .18 | <.001 | −.26 | .086 | .43 | <.001 | .58 | <.001 |
| Factor 7 | 6.11 ± 1.13 | 6.54 ± 1.13 | <.001 | 6.60 ± 1 | 6.20 ± 1.16 | <.001 | .65 | .010 | .38 | .004 | −.37 | <.001 | −.03 | .263 |
Note: Bold text indicated there is no correlation expected by theory; italic text represented no specific assumption existed.
Six experts from the expert committee evaluated the questionnaire on the basis of the relevance of each item to the concept being measured. Content validity was based on the four-point method (Shi, Mo, & Sun, 2012), that is, 1 = very relevant, 2 = relevant, 3 = irrelevant, and 4 = very irrelevant. If “very relevant” or “relevant” was filled in, then 1 point was given; 0 point was given to the other two choices. The range of I-CVI was .83–1.00, and the mean CVI (S-CVI/Ave) was .96. Both of which reached a good level.
Reliability and item analysisThe corrected item-total correlation coefficients ranged from .40∼.55. The Cronbach's α of the subscales were satisfactory and ranged between .77∼.93. Forty field-tested subjects were selected and retested after two weeks. The ICC for the total scale was .87 and for the seven factors: .82, .80, .84, .75, .85, .80, and .78, respectively.
DiscussionThe purpose of the present research was to analysis the psychometric properties of C-EIDECS in a sample of Chinese ICU medical staff. EFA was conducted with Oblique rotation and enforcing seven-factor solution. The structure obtained was the same as the one found by the authors of the original questionnaire. This solution explained 70.61% of the total variance. The value was higher than the 52% obtained by the original questionnaire. Furthermore, the correlation between the factors implied that increasing the cooperation of the medical staff in the EOL context, clarifying their respective roles in the EOL situation, spending more time on communicating with family members, obtaining more emotional support in the team, can all help to reduce the stress on EOL decision making, and initiate EOL decisions in a timely manner. These findings were also consistent with recent research in EOL context (Laurent, Bonnet, Capellier, Aslanian, & Hebert, 2017).
In order to further test the theoretical foundation of the EIDECS, we performed CFA with the original seven subscales. The results showed that the χ2/df was 4.71, which did not meet the strict standard range 1-3 but was within the range of the loose value <5. Because this value is susceptible to sample size, it needs to be combined with other indicators to make a comprehensive judgment about its applicability (Greene et al., 2019). The RMSEA and SRMR suggested an acceptable fit. Although TLI and CFI did not reach the best adaptation value, they were close to the cutoff value. Considering the numerical results obtained, as well as the theoretical and substantive aspects derived from the research field (Hughes, Booth, & Irwing, 2018), the seven-factor structure of EIDECS can be considered as being appropriate to be applied in China.
The structural validity of the questionnaire was further tested through the relationship between the subscales of C-EIDECS and other variables. Previous studies have shown that nurses are less involved and less satisfied with EOL decisions-making than physicians, have more negative evaluations of teamwork, and experience more ethical dilemmas (Jox et al., 2010; Noome, Dijkstra, van, & Vloet, 2016), which is consistent with the results obtained in the present investigation. Furthermore, there is a correlation between satisfaction with EOL decision making, communication, emotional exhaustion and stress overload. Most of these findings are similar to the original questionnaire, which suggests that to develop a collaborative decision-making framework involves all healthcare providers, improve EOL decision participation, and create a more standardized method for EOL decision (Brooks, Manias, & Nicholson, 2017). This approach may be beneficial to reduce the stress associated with EOL decision-making and to improve EOL satisfaction.
Following the European model for test quality evaluation (Muñiz & Fonseca-Pedrero, 2019), the reliability of the questionnaire is good with both internal consistency (Cronbach’s α of the subscales >.70) and test-retest reliability (ICC ranged from .75∼.86). In addition, the corrected item-total correlation coefficients were all over .40, indicating an adequate degree of item homogeneity.
The study has several limitations. This research adopted the principle of convenient cluster sampling and failed to select ICU medical staff of different grades in line with the equal probability stratified sampling method. Therefore, the sampling affected the representativeness of the sample to some extent. Henceforth, numerous medical institutions from different geographical areas and different natures should be selected to expand the breadth and depth of the samples, and the questionnaires should be further revised and verified. On the other hand, some fit indices of CFA failed to reach the cutoff limit. Due to the lack of strict standards for modification indices (MI), the residuals and their magnitudes to be released depend on the subjective choices of the researchers. Also some degree of bias is unavoidable when the final modified model is to be tested with a new sample. No further modification was made to the model using MI. In the future, more extensive samples can be selected to further explore the model.
In conclusion, the C-EIDECS questionnaire is a reliable and valid instrument for measuring the facilitators of and barriers to effective EOL decision making and communication and the associated pressure perceived by relevant ICU medical staff among the Chinese population.
FundingThis article was funded by Zhejiang Health Science and Technology Project (No. 2020KY159).