El 25,9% de los españoles padece dolor crónico. Se recomienda un enfoque integral, interdisciplinar, con terapias farmacológicas y no farmacológicas, participando los pacientes en su autocuidado.
Objetivoevaluar la efectividad y el impacto en recursos de un programa/taller con terapias no farmacológicas en el control del dolor crónico no-oncológico a corto y medio plazo.
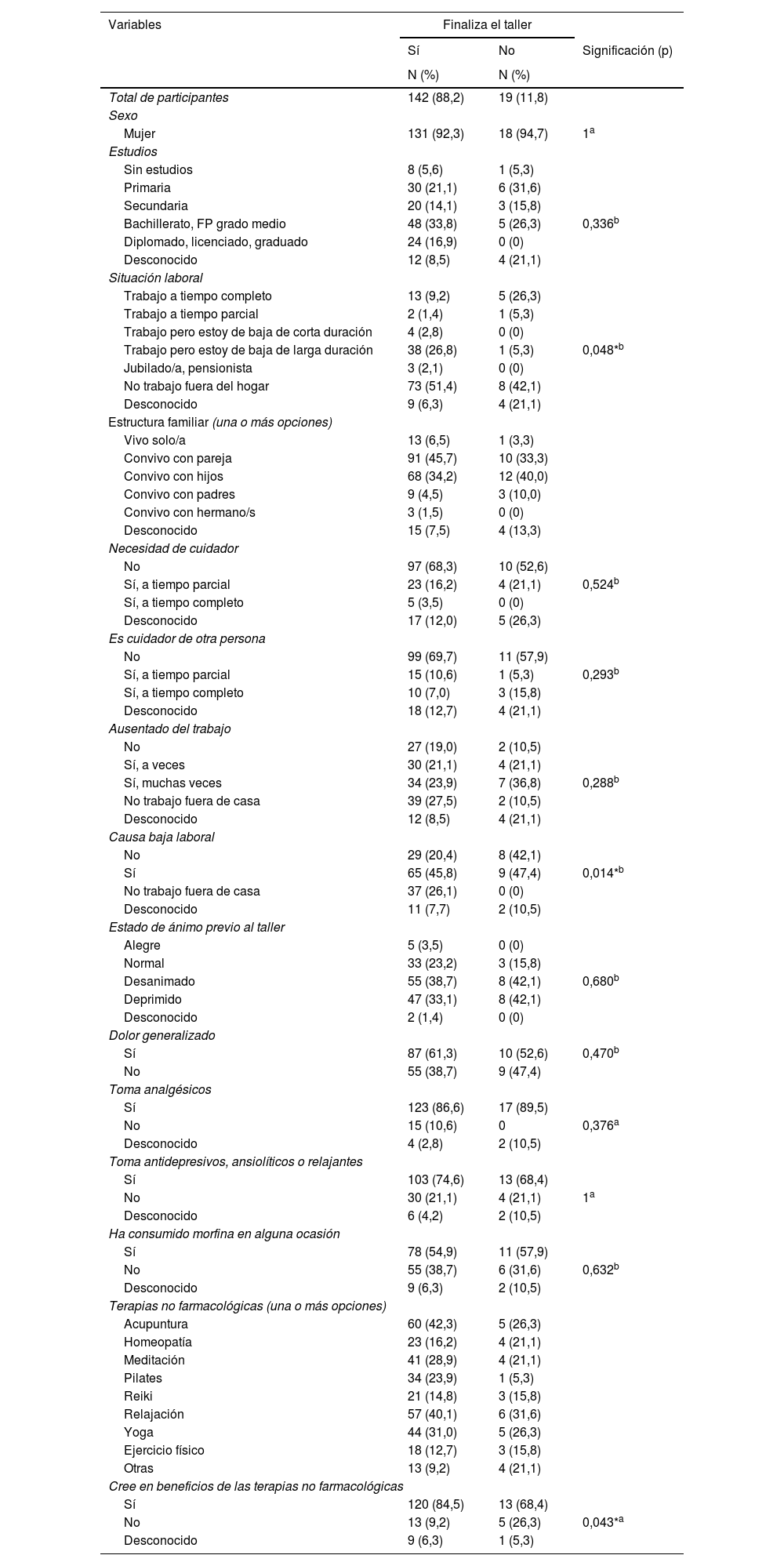
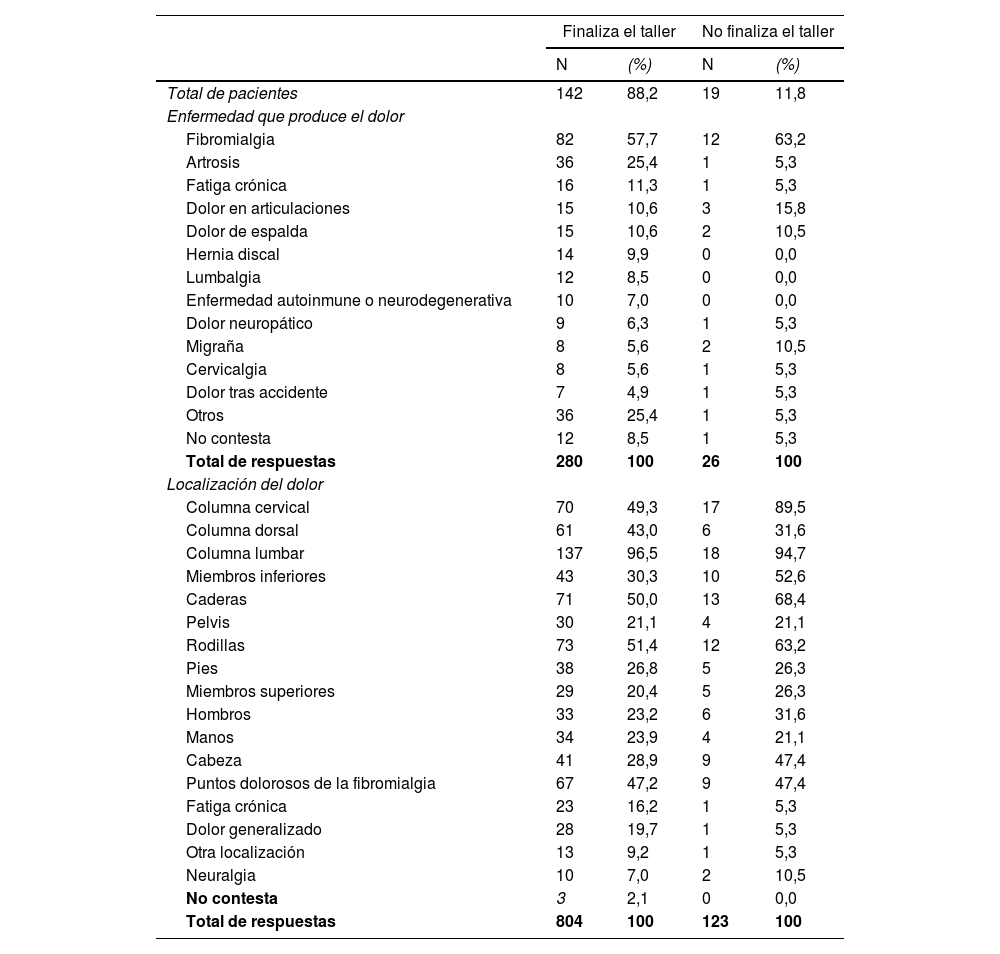
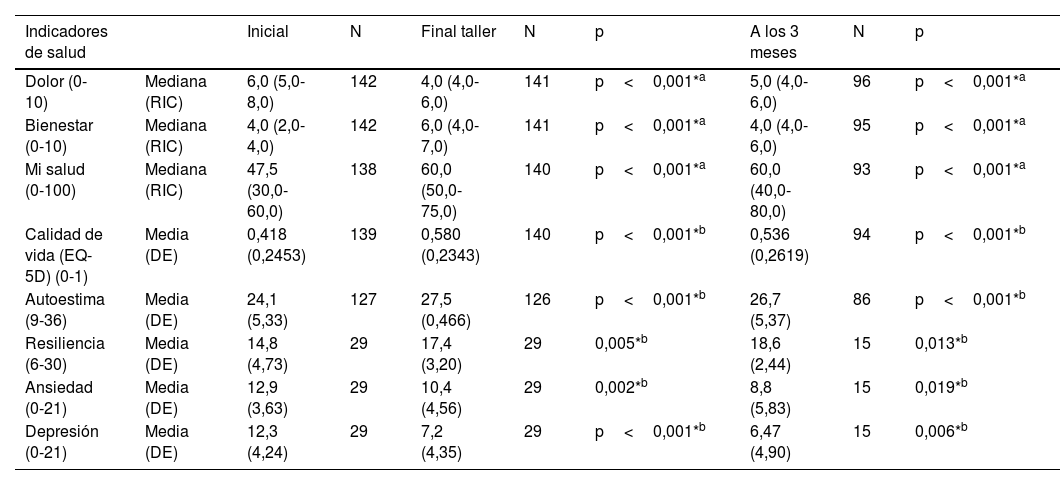
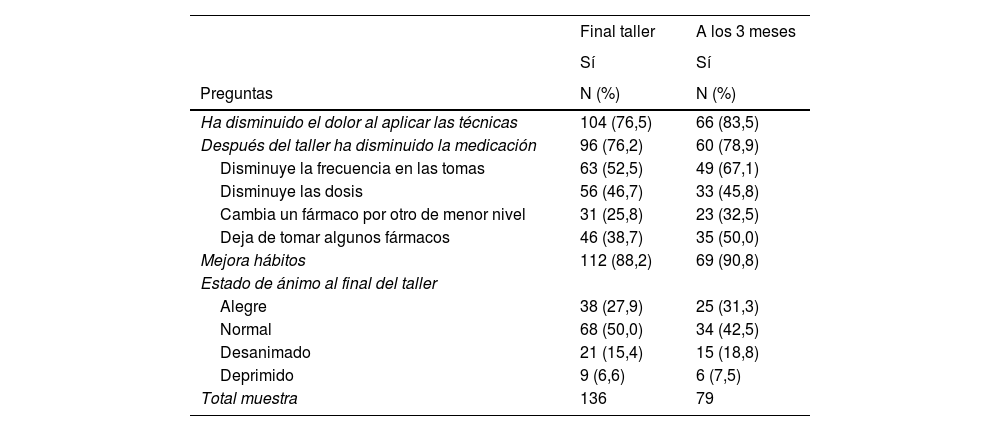
Material y métodosEstudio cuasiexperimental antes-después, seguimiento 3-6 meses, midiendo: dolor, bienestar, calidad de vida, autoestima, resiliencia, ansiedad/depresión (escalas validadas); resultados aportados por los pacientes del impacto del programa en manejo del dolor, hábitos y ánimo; visitas a urgencias y consultas; consumo de fármacos y situación laboral.
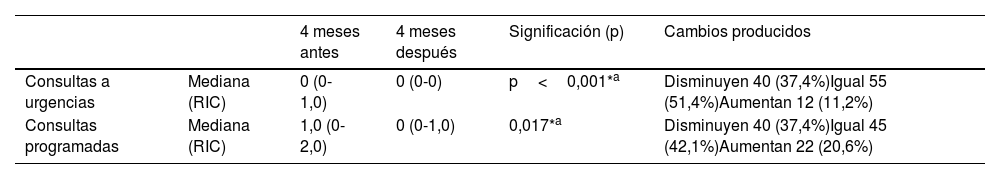
ResultadosFinalizaron el taller 142 pacientes; 131 (92,3%) eran mujeres, edad: 56,0. Disminuyeron: dolor (escala 0-10) (inicio: 6,0; fin taller: 4,0; 3 meses: 5,0); ansiedad (12,9; 10,4; 8,8) y depresión (12,3; 7,23; 6,47) (escalas 0-21). Aumentaron: bienestar (escala 0-10) (4,0; 6,0; 4,0); calidad de vida (escala 0-1) (0,418; 0,580; 0,536); estado de salud (escala 0-100) (47,5; 60,0; 60,0); autoestima (escala 9-36) (24,1; 27,5; 26,7); resiliencia (escala 6-30) (14,8; 17,4; 18,6). Realizan aportación de resultados 136 pacientes al finalizar el taller y 79 a los 3 meses: disminuyeron el dolor (final taller: 104, 76,5%; 3 meses: 66, 83,5%); disminuyeron medicación (96, 76,2%; 60, 78,9%); mejoraron hábitos (112, 88,2%; 69, 90,8%). Redujeron visitas a urgencias 40 pacientes (37,4%), 40 (37,4%) disminuyeron las consultas programadas. Satisfacción global: 9,8 sobre 10.
ConclusionesEl paciente aprende a mitigar su dolor, participa en su autocuidado y mejora su calidad de vida, autoestima y estado emocional. Los efectos se mantienen 3-6 meses.
25.9% of Spanish people suffer from chronic pain. An integrated, interdisciplinary approach is recommended, with pharmacological and non-pharmacological therapies, involving patients in their self-care.
ObjectiveTo evaluate the effectiveness and impact on resources of a program with non-pharmacological therapies in the control of non-oncological chronic pain in the short and medium term.
Material and methodsQuasi-experimental before-after study, follow-up 3-6 months, measuring: pain, well-being, quality of life, self-esteem, resilience, anxiety/depression (validated scales); patient-reported outcomes of workshop impact on pain management, habits and mood; ED and office visits; drug consumption and employment status.
ResultsOne hundred and forty-two patients completed the program; 131 (92.3%) were women, age: 56.0. Decreased: pain (scale 0-10) (start: 6.0; end of workshop: 4.0; 3 months: 5.0); anxiety (12.9; 10.4; 8.8) and depression (12.3; 7.23; 6.47) (scales 0-21). They increased: well-being (scale 0-10) (4.0; 6.0; 4.0); quality of life (scale 0-1) (0.418; 0.580; 0.536); health status (scale 0-100) (47.5; 60.0; 60.0); self-esteem (scale 9-36) (24.1; 27.5; 26.7); resilience (scale 6-30) (14.8; 17.4; 18.6). Patient-reported outcomes were performed by 136 patients at the end of the workshop and 79 at 3 months: pain decreased (end of program: 104, 76.5%; 3 months: 66, 83.5%); medication decreased (96, 76.2%; 60, 78.9%); habits improved (112, 88.2%; 69, 90.8%). Forty patients (37.4%) reduced visits to the emergency room, 40 (37.4%) reduced scheduled visits. Overall satisfaction: 9.8 out of 10.
ConclusionsPatients learn to mitigate their pain, participate in their self-care and improve their quality of life, self-esteem and emotional state. The effects remained for 3-6 months.