There is a lack of data about adverse events (AE) in intermediate and long-term care centers (ILCC). We aimed to synthesize the available scientific evidence on instruments used to identify and characterize AEs. We also aimed to describe the most common adverse events in ILCCs.
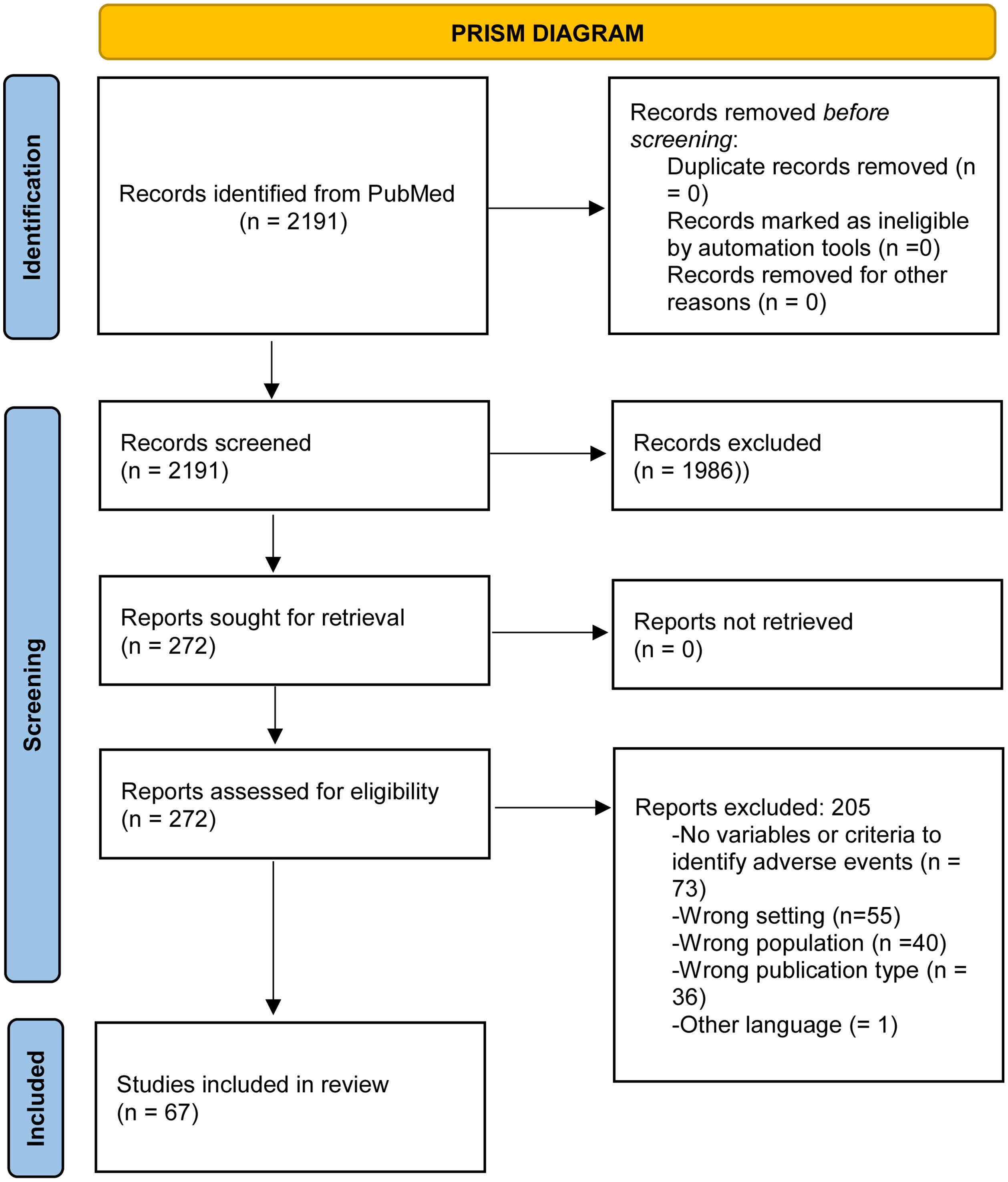
Material and methodsA narrative systematic review of the literature was conducted according to Prisma recommendations. The PubMed database was searched for articles published between 2000 and 2021. Two reviewers independently screened and reviewed the studies through blind and independent review. We evaluated bias risk with Cochrane's risk of bias tool. Disagreements were resolved by consensus. Discrepancies that were not resolved by discussion were discussed with a third reviewer. Descriptive data was extracted and qualitative content analysis was performed.
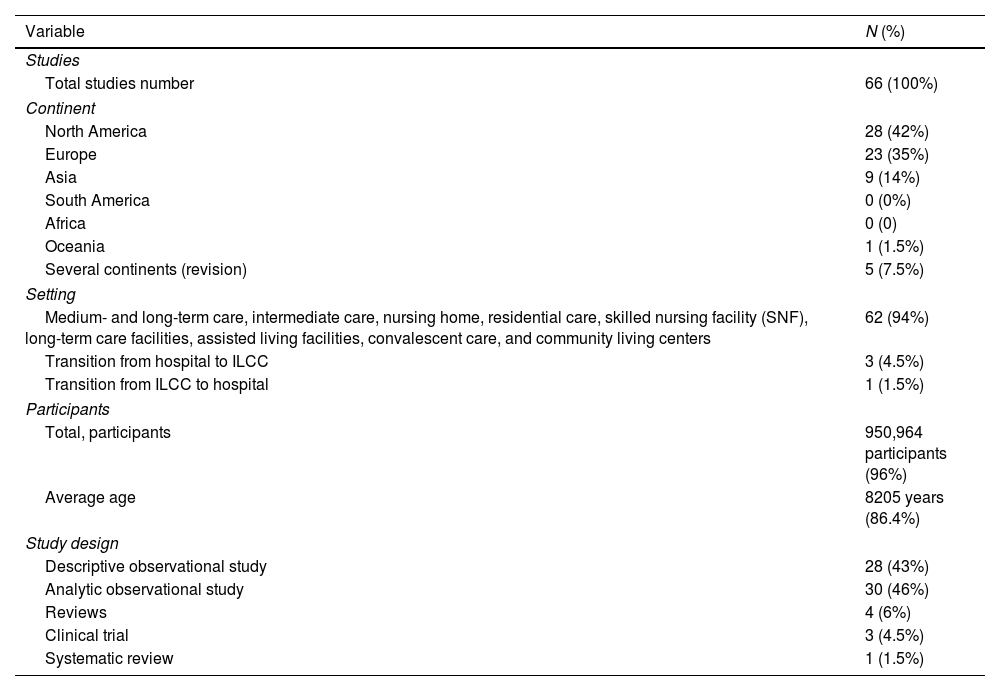
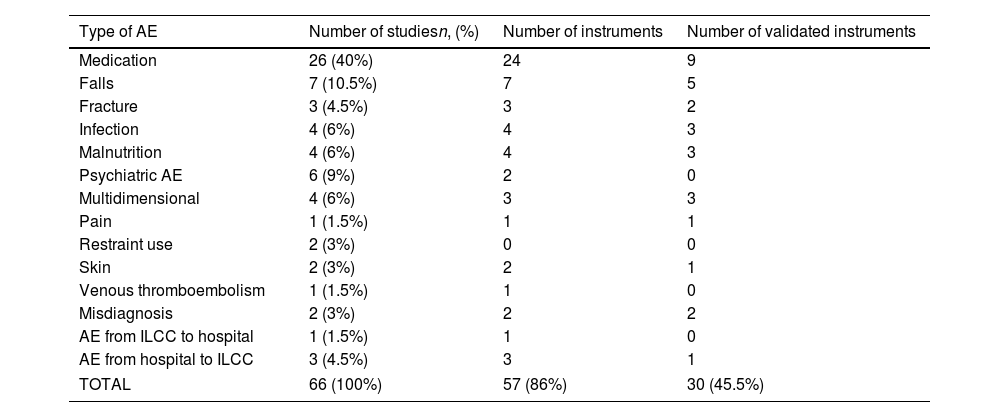
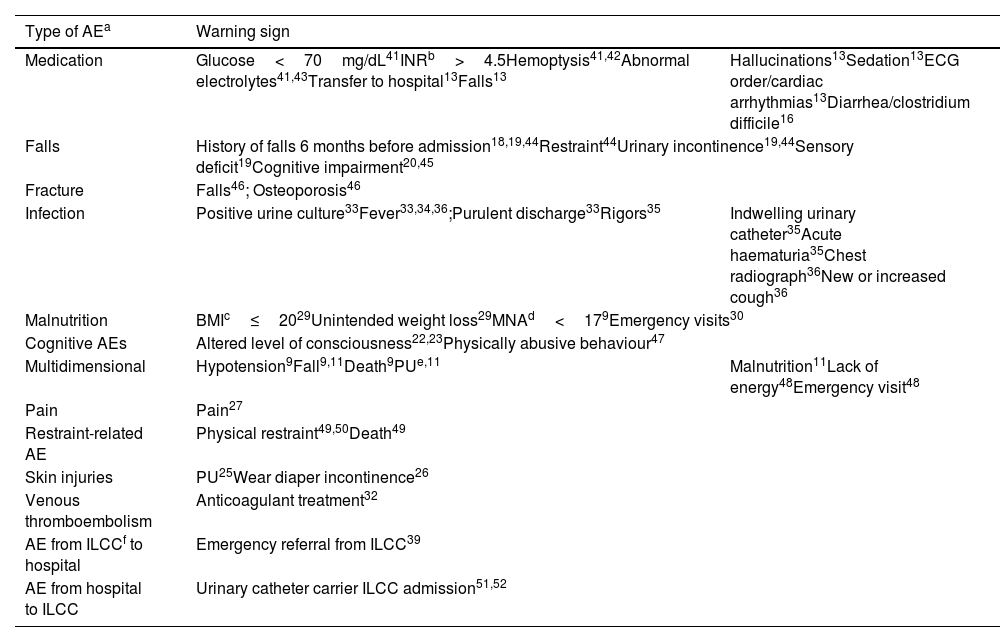
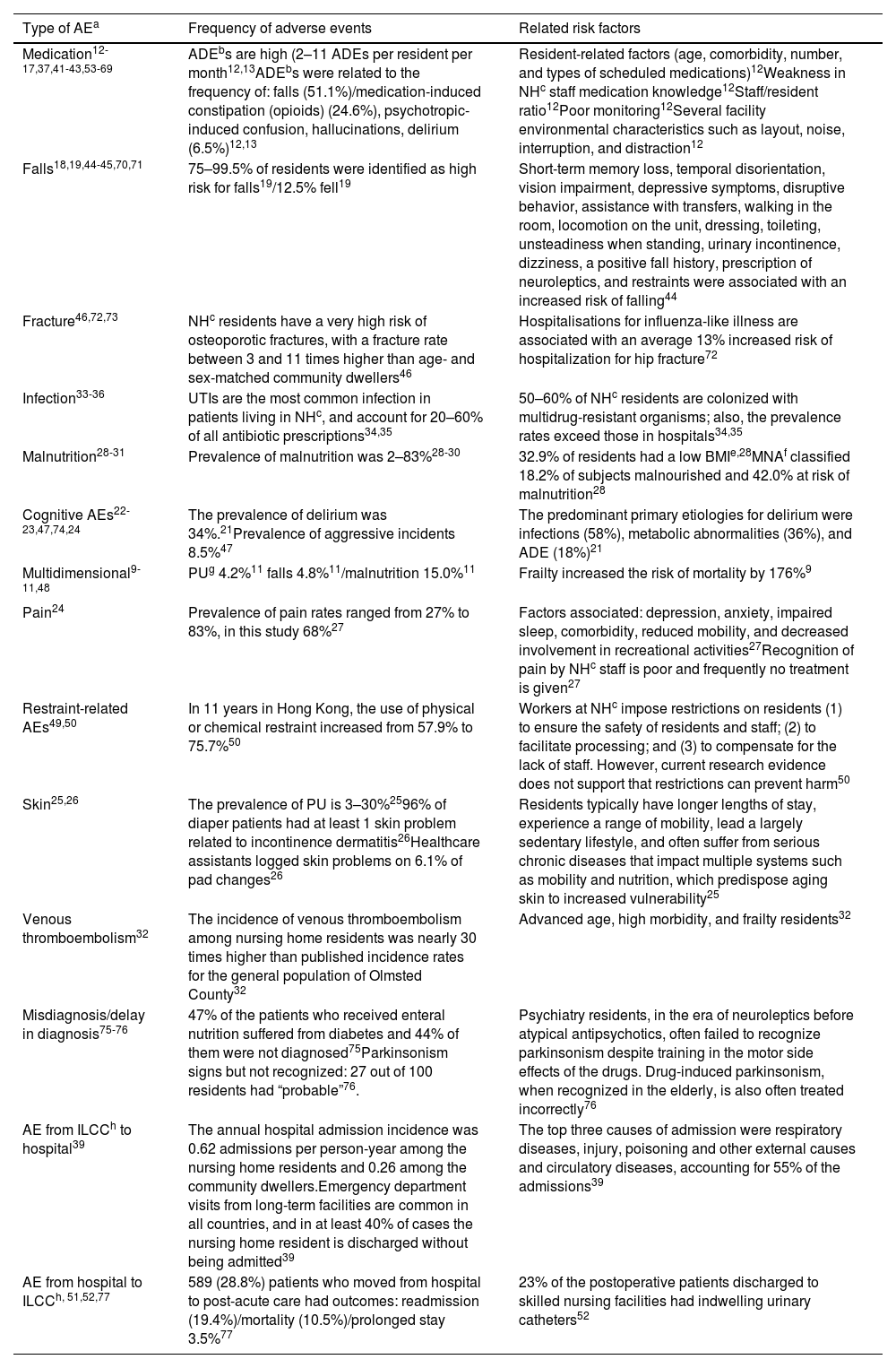
ResultsWe found 2191 articles. Based on the inclusion and exclusion criteria, 272 papers were screened by title and abstract, and 66 studies were selected for full review. The instruments used to identify AEs were mostly tools to identify specific AEs or risks of AEs (94%), the remaining 6% were multidimensional. The most frequent categories detected medication-related AEs (n=26, 40%); falls (n=7, 11%); psychiatric AEs (6.9%); malnutrition (4.6%), and infections (4.6%). The studies that used multidimensional tools refer to frailty, dependency, or lack of energy as predictors of AEs. However, they do not take into account the importance of detecting AEs. We found 2–11 adverse drug events (ADE) per resident/month. We found a prevalence of falls (12.5%), delirium (9.6–89%), pain (68%), malnutrition (2–83%), and pressure ulcers (3–30%). Urinary tract infections, lower respiratory tract infections, skin and soft tissue infections, and gastroenteritis were the most common infections in this setting. Transitions between different care settings (from hospitals to ILCC and vice versa) expose AE risk.
ConclusionThere are many instruments to detect AEs in ILCC, and most have a specific approach. Adverse events affect a significant proportion of patients in ILCC, the nurse-sensitive outcomes, nosocomial infections, and adverse drug events are among the most common.
The systematic review was registered with Prospero, ID: CRD42022348168.
Existe una falta de datos sobre los eventos adversos (EA) en los centros de cuidados intermedios y de larga estancia (CCIL). Nuestro objetivo fue sintetizar la evidencia científica disponible sobre los instrumentos utilizados para identificar y caracterizar los EA. También pretendemos describir los EA más frecuentes en los CCIL.
Material y métodosSe desarrolló una revisión sistemática narrativa de la literatura siguiendo las recomendaciones Prisma. Se realizaron búsquedas en la base de datos PubMed de artículos publicados entre 2000 y 2021. Dos revisores seleccionaron y revisaron de forma independiente los estudios mediante revisión ciega e independiente. Se evaluó el riesgo de sesgo con la herramienta de riesgo de sesgo de Cochrane. Los desacuerdos se resolvieron por consenso, las discrepancias que no se resolvieron mediante discusión se solucionaron con un tercer revisor. Se extrajeron datos descriptivos y se utilizó el análisis de contenido cualitativo.
ResultadosSe encontraron 2.191 artículos. Según los criterios de inclusión y exclusión, se examinaron 272 artículos por título y resumen y se seleccionaron 66 estudios para la revisión completa. Los instrumentos para identificar los EA eran en su mayoría herramientas para detectar EA específicos o riesgo de EA (94%), el 6% restante eran multidimensionales. Las categorías más frecuentes que se detectaron EA fueron los relacionados con la medicación (n=26, 40%); caídas (n=7, 11%); EA psiquiátricos (6,9%); malnutrición (4,6%), e infecciones nosocomiales (4,6%). Los estudios que utilizaron herramientas multidimensionales se relacionaron con la fragilidad, dependencia o falta de energía y se utilizaron como predictores de EA pero que no contemplaron la globalidad para detectar EA en este ámbito. Se encontraron de dos a 11 eventos adversos con medicamentos (EAM) por residente/mes. Encontramos prevalencia de caídas (12,5%), delirio (9,6-89%), dolor (68%), desnutrición (2-83%), úlceras por presión (3-30%). Las infecciones del tracto urinario, las infecciones del tracto respiratorio inferior, las infecciones de piel y tejidos blandos y la gastroenteritis fueron las infecciones más comunes en este entorno. Las transiciones entre diferentes entornos asistenciales (de hospitales a CCIL y viceversa) expusieron un riesgo adicional de desarrollar EA.
ConclusionesExiste una gran variedad de instrumentos para detectar EA en CCIL, y la mayoría de ellos tienen un enfoque específico. Los EA afectan a una proporción importante de pacientes en CCIL, siendo los resultados relacionados con los cuidados, las infecciones nosocomiales y los EAM los más frecuentes.
La revisión sistemática se registró en Prospero, ID: CRD42022348168.