The outbreak of COVID-19 has overwhelmed healthcare systems all over the world. The aim of this article is to describe the process of transforming the Vall d’Hebron University Hospital, the second largest hospital in Spain, into a COVID-19 centre coordinating response to the pandemic in its reference area.
Materials and methodsThe study draws on the experience of the authors in transforming the hospital into a comprehensive resource in response to the COVID-19 pandemic. The strategy is based on four central strategies: early planning, coordination of all healthcare agents in its reference area, definition of clear leadership roles, and the organisation of care based on multidisciplinary teams with minimal recruitment of new staff.
ResultsThe transformation strategy enabled the hospital to cope with the surge in patients without exceeding its capacity. During the response phases, which amounted to a period of 57 days, 3106 patients consulted the ER and 2054 were admitted, 346 of whom were treated at the ICU. To accommodate the number of adult COVID-19 patients, adult ICU availability was progressive increased by 371%, and ordinary beds increased by 240. A total of 671 staff members went on sick leave after testing positive for COVID-19.
ConclusionThe transformation experience of the hospital provides insight into how effectively adapt the structures and functioning of large hospitals. The relevance of territorial coordination during the pandemic is stressed as an effective strategy that contributed coping the pandemic.
La pandemia de COVID-19 ha sobrepasado los sistemas sanitarios de todo el mundo. El objetivo de este artículo es el de describir el proceso de transformación del Hospital Universitario Vall d’Hebron, segundo hospital más grande de España, en un centro de respuesta coordinada a la pandemia de COVID-19 en su área de referencia.
Materiales y métodosEste estudio muestra la experiencia de los autores en la transformación del hospital en un importante recurso en respuesta a la pandemia de COVID-19. La estrategia seguida se basa en 4 ejes centrales: planificación previa, coordinación de los agentes sanitarios en el área de referencia, definición clara de las funciones de los cargos de liderazgo y organización de la atención basada en equipos multidisciplinarios con la mínima contratación de nuevo personal.
ResultadosLa estrategia de transformación permitió al hospital hacer frente a la oleada de pacientes sin exceder su capacidad. Durante la fase de respuesta, que duró 57 días, 3.106 pacientes acudieron a urgencias y 2.054 fueron ingresados, 346 de los cuales fueron tratados en la UCI. Para atender al gran número de pacientes adultos de COVID-19, la UCI de adultos se amplió progresivamente hasta el 371% y el número de camas normales aumentó en 240. Un total de 671 miembros del personal tuvieron la baja por enfermedad después de ser positivos en el test de COVID-19.
ConclusiónLa experiencia adquirida durante esta transformación aporta una visión de cómo adaptar efectivamente la estructura y la función de grandes hospitales. La importancia de la coordinación territorial durante la pandemia se muestra como una estrategia efectiva para evitar que los hospitales excedan su capacidad.
The COVID-19 outbreak has overwhelmed healthcare systems around the planet, since the systems currently in place have limited experience in coping with the intensive challenges that a pandemic poses. Past outbreaks such as the Middle East Respiratory Syndrome Coronavirus (MERS-CoV), the Severe Acute Respiratory Syndrome (SARS) and the 2009 swine flu epidemic highlighted the risks that a pandemic might represent in terms of hospital capacity; however, the demands on resources in the current situation have far exceeded those of past epidemics. In fact, hospitals around the world have had to undergo unprecedented transformations to cope with the impact of COVID-19.1,2
Some previous research report the transformation processes of healthcare hospitals into COVID-19 centres. In China, where most reports have been published, the national strategy was oriented towards concentrating patients, health staff, resources and treatments in special facilities3 including the construction of temporary ark hospitals to treat mildly ill patients4 and the creation of makeshift hospitals in existing buildings.5 In Italy, the hospital in Lodi, Lombardy centralised the management of the pandemic inside a crisis unit which worked in close contact relation with the regional authorities and reorganised its entire hospital infrastructure in record time.1 In France, the Assistance Publique-Hôpitaux de Paris developed a data-driven strategy based on the coordinated management of their centres, using multidisciplinary working groups and developing a unified platform to recruit human resources and a central ICU bed-allocation system.6
In Spain, the first case of COVID-19 was confirmed on January 31 in La Gomera in the Canary Islands. Six weeks later, on March 14, Spain declared a state of emergency and imposed rigorous lockdown measures for the population.7 Hospitals across the country have undergone functional transformations to attend to the large number of COVID-19 patients requiring emergency and inpatient care while at the same protecting the safety of workers in a context of limited economic and material resources. Given that the pandemic significantly limited the possibility of external support, each hospital had to define a transformation strategy with the resources available to it. These transformations took place in a context of scarce evidence stemming from the Chinese experience.8–11
Vall d’Hebron University Hospital (HUVH) is a public tertiary care hospital in Barcelona. It is part of the Catalan Public Healthcare System, which provides universal coverage to the population. The hospital works in close coordination with other healthcare organisations in the area, including one secondary care hospital, three intermediate care centres and 19 primary care centres. The HUVH is equipped with approximately 1100 beds, has over 7500 healthcare professionals and provides coverage to a population of around 450,000 people. It is also a reference hospital at regional and national level for highly complex procedures and rare diseases. Each year, the hospital performs around 36,000 major surgical procedures, 420 transplants, 60,000 hospitalisations, 210,000 emergency care contacts, and over a million outpatient consultations.
Countries around the world are currently facing the threat of successive waves of the pandemic. However, unlike the first wave, we have now the experience and several strategies put in place, such as response plans and coordination structures, which may assist hospitals in their response. Here, we describe the transformation of the HUVH, the second biggest hospital in Spain, into a COVID-19 hospital which coordinates action at territorial level with public and private hospitals inside its reference area. Our aim is to provide useful information on effective management and organizational strategies that we hope will be a valuable resource for other hospitals around the world to respond further pandemic waves.
Coordination and planning of response measuresThe Executive Board (EB) of the HUVH, comprising its CEO and Directors, is the hospital's highest planning and decision-making body. In mid-January 2020, to prepare the hospital for the imminent pandemic, the EB decided: (i) to create a COVID-19 Task Force, (ii) to plan the organisational transformation of the hospital during the pandemic, and (iii) to lead the coordination among healthcare agents in the area to ensure the most efficient allocation of patients and resources. By then, the spread of COVID-19 as a global pandemic was already a likely scenario and these measures were designed to avoid risks related to improvisation, tension, the lack of coordination between different actors, and deficiencies of essential resources.
(i) The aim of the COVID-19 Task Force was to provide the EB with a scientific and organisational overview of the situation in order to guide decision-making with regard to new emerging data and needs, exercising a scientific leadership role. It began its operations on January 27 and met three to five times per week until May 18. The Task Force was led by the Chief Medical Officer (CMO) and comprised a multidisciplinary team including epidemiologists, infectious disease experts, microbiologists, emergency care and occupational health specialists, and members of the EB.
(ii) The plan for the organisational transformation of the hospital defined a set of measures to respond to the pandemic, taking into account input from the COVID-19 Task Force. It was defined considering the existing workforce, since it was impossible to take on significant numbers of new staff. The two deputy directors of the EB were responsible for the transformation of the hospital and for defining the rhythm of the process. The EB also coordinated the progressive creation of COVID-19 clinical teams: the departments of Infectious Diseases, Pulmonology and Internal Medicine, defined as the Core Medical Departments, took on the clinical leadership of all the COVID-19 teams and oversaw the application of clinical decisions in the hospital wards.
(iii) Territorial coordination was one of the most important activities for guaranteeing the availability of resources. The aim was to map and coordinate all the available resources in the area that could be fully dedicated to attending to COVID-19 patients, including public and private health care centres (hospitals, primary care, social care, clinics) and non-health centres such as sports centres and hotels. To prepare this unprecedented move, the EB made an agreement with the five hospitals in the territory to simultaneously transform these hospitals into a coordinated network of COVID-19 hospitals. The participating hospitals were Hospital San Rafael, Hospital Pere Virgili, Hospital Isabel Roig, Hospital Quirón and Hospital HM Delfos. This agreement was approved by the regional healthcare authority.
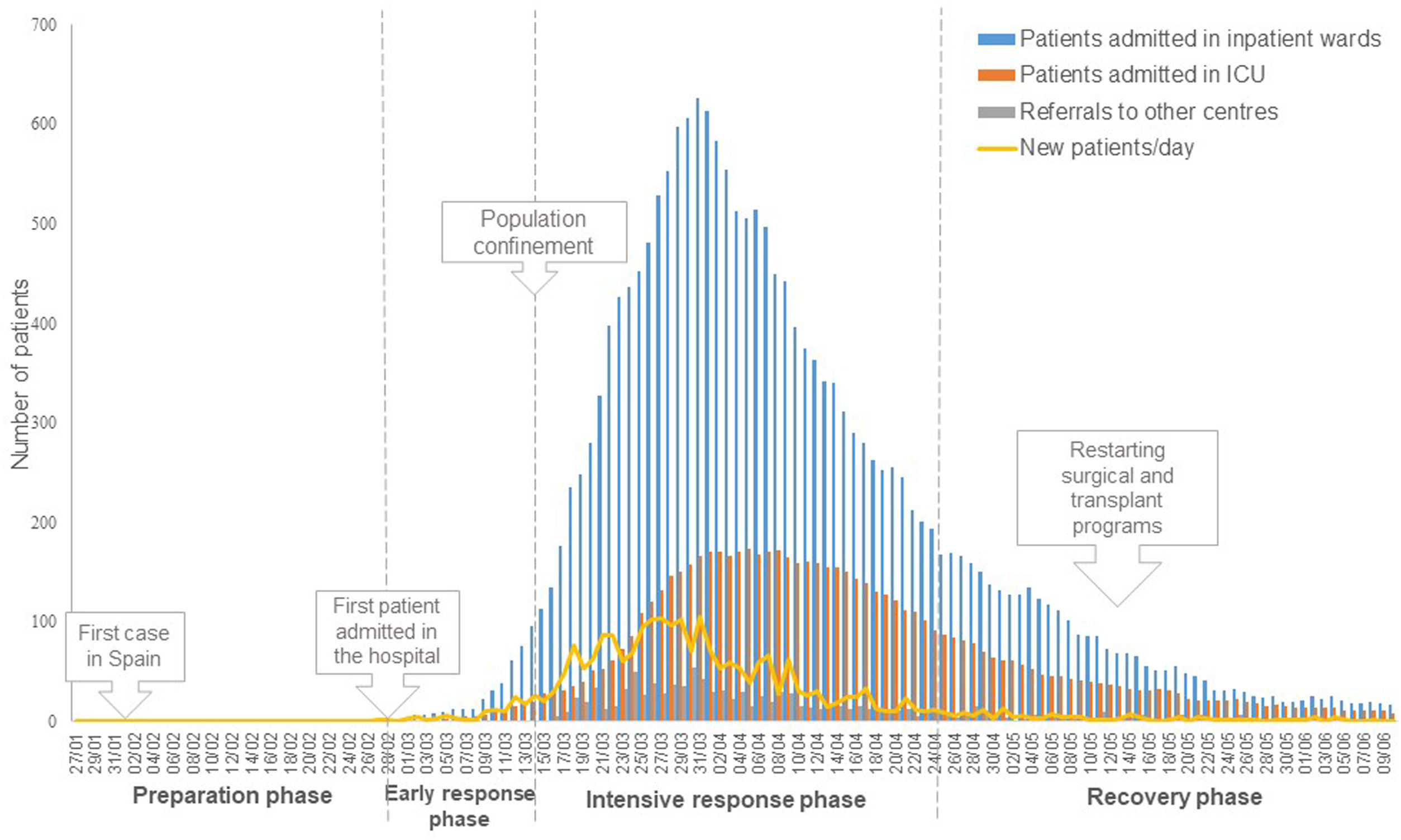
Response phasesThe response to the first wave of the pandemic can be divided into four phases (see Fig. 1). The specific actions implemented are described below.
(i) Preparation phase: January 27 to February 26 2020The preparation phase began once the risk of a pandemic became real. The first step was the creation of the COVID-19 Task Force. During this phase, actions were mainly focused on defining the basis for coordinated action, including the analysis of possible scenarios and actions to deal with risks, the definition of specific workflows, and the establishment of communication channels with staff. When hypothetical scenarios were analysed, only the ones in which a successful response of the hospital was possible were considered: catastrophic scenarios that might have had a paralysing effect were avoided.
Infection prevention and control measures. The EB and the COVID-19 Task Force defined the necessary premises for guaranteeing the safest possible conditions for healthcare professionals. As early as the second week of February, a specific workflow in the emergency rooms (ER) for COVID-19-suspected patients was defined. In contrast to the protocols in place and to avoid the risk of misdiagnosis, we assumed that communitarian virus transmission might be possible from the very beginning. Consequently, all patients with suspected pneumonia or respiratory infection who were admitted to the emergency room were placed in specific ER boxes and tested for SARS-CoV-2 by PCR. The hospital's microbiology laboratory was in charge of conducting PCR tests, although at that moment the recommendation was that a centralised laboratory should carry out tests for the whole of Catalonia. Experienced infectious disease specialists joined ER staff in attending to the COVID-19 suspected patients.
Real time data analysis and information systems. Epidemiologists modelled possible scenarios according to the epidemiological data available. These scenarios, updated as new data emerged, provided useful input for defining and modifying the plan for the organisational transformation of the hospital.
Communication plan. To avoid panic, confusion, and disorientation and to promote adherence to constantly evolving clinical protocols and workflows, leaders of the Epidemiology and Infectious Diseases departments and the Occupational Risk Prevention Unit offered daily meetings for all hospital workers in the conference hall of the hospital. Updated information regarding the disease, changes in protocols or workflows and recommendations was shared.
(ii) Early response phase: from February 27 to March 13, 2020The early response phase started when the first COVID-19 patient was admitted to the hospital. In this phase, the plan for the transformation of the hospital was progressively deployed and updated according to the analysis of possible scenarios and the capacity requirements in terms of spaces, beds, supplies, and human resources. All these actions were shared with other hospitals in our area, which introduced the protocols, workflows and other actions designed to achieve coordinated territorial strategy.
Actions to increase the hospital infrastructure and capacity. Several strategies were put in place to ensure that the required number of ICU and conventional hospitalisation beds were available. Surgical and transplant programmes were progressively reduced. On March 10, a plan to convert most hospital wards into COVID-19 clinics (W-COVID-19) was initiated. On March 11, all locations that might serve as an ICU with enough space to include 20 or more beds were identified, including operating theatres and reanimation facilities. Before the pandemic, the HUVH had 56 adult ICU beds, and the plan was to add a further 245 ICU beds.
Reorganisation of the workforce. As a significant increase in staff was not possible in our context, the efficient reorganisation of the human resources was of paramount importance. Three types of teams were created to treat COVID-19 patients. First, in the ER, the ER-COVID-19 teams were reorganised to include one experienced physician from the Emergency Care, Infectious Diseases, Pulmonology, and Internal Medicine departments. These teams were completed by specialised nurses. Secondly, in the hospital wards, W-COVID-19 teams were created, each team comprised eight physicians who attended 28 patients per ward led by an expert physician at one of the Core Medical Departments. The rest of the team was made up of staff members or residents from almost all the medical and surgical departments in the hospital. COVID-19 teams were organised in two daily shifts. Finally, in the ICU, staff numbers rose progressively; the ICU-COVID-19 teams included anaesthesiologists, paediatricians, cardiologists, maxillo-facial surgeons, plastic surgeons, and traumatologists.
Actions to enhance human resources capacity. Vacations and travel authorisations were cancelled for all hospital staff. Retired ICU specialists were incorporated and the hiring of nurses who had completed their training this year was encouraged. Finally, the hospital recruited volunteers to reinforce non-clinical work.
Infection control and prevention measures. Several measures were implemented to reduce the probability of the disease spreading in the hospital. Clinical sessions were limited to those essential for decision-making, respecting the interpersonal distances marked by the protocols at all times, and coffee bars and restaurants inside the hospital were closed.
Real time data analysis and information systems. The Information Systems department produced automatic reports that provided twice-daily information to monitor the epidemic progression curve and the hospital's situation in terms of capacity and needs.
Communication plan. Face-to-face meetings with staff were cancelled and streaming sessions started. The sessions included updated information concerning the disease and protocols, and served to address concerns and doubts of staff. In addition, the Communication Department was responsible for publishing updated information regarding actions and measures decided by the EB.
(iii) Intensive response phase, from March 14 to April 23, 2020The intensive response phase started when the Real Decreto de Alarma (Royal Decree of Alarm) was published on March 14 by the Spanish authorities. In this phase, the overall contingency plan was updated in response to the new scenario of the rapid rise in the number of infected patients. The main actions at this point included the extension of the hospital facilities outside the buildings of the HUVH, and the strengthening of security measures, including restrictions on visits.
Actions to transform the hospital infrastructure and increase capacity. Several actions to increase the number of available beds were carried out. All scheduled non-urgent surgery was cancelled on March 16, including transplants, thus making more beds available to treat COVID-19 patients. The cancellation of the transplant programme, one of the hospital's most emblematic activities, was seen by the staff as an unequivocal message regarding the seriousness of the situation. Many areas of the hospital were converted to create additional inpatient and ICU wards, including outpatient clinics and administrative areas. In addition, 132 beds were added for the treatment of patients who were not candidates for ICU admission by expanding the hospital facilities to the Olympic Sports pavilion, located across the road from the hospital. Finally, two nearby hotels were adapted to be able to admit discharged patients and staff who lacked adequate isolation conditions in their homes. The hospital was in charge of providing the resources, logistics and care required in these hotels.
Infection prevention and control measures. All visits were prohibited, including those by relatives of hospitalised patients. Following the advice of the Healthcare Ethics Committee, relatives’ visits were allowed under specific circumstances: for instance, end-of-life care, paediatric patients, post-partum, and patients with high dependence or with cognitive needs. A team of physicians was entrusted with guaranteeing regular communication between professionals and the relatives of admitted patients. Several programmes were implemented to help patients and families cope with isolation and anxiety, and to ensure good quality communication and accurate information. Telecommuting was promoted when possible. Outpatient clinics were closed, and outpatient consultations were attended only in case of emergency. We started a programme of home delivery of medication which in normal circumstances is supplied at the hospital, and telemedicine was encouraged.
Psychological support to healthcare workers. The Psychiatry department launched a Mental Health Intervention Plan for all professionals to ensure their psycho-emotional well-being and to prevent adverse emotional reactions. This plan included the detection of psychological needs, the implementation of psychosocial interventions, organisation of mindfulness sessions with staff under high emotional pressure (such as ICU staff), and the provision of guidance on how to provide basic emotional and practical support to affected people.
Communication plan. From March 14 onwards, daily morning sessions were conducted by the CMO to report the latest actions carried out and the evolution of the pandemic in the hospital to directors and deputy directors. Daily streaming sessions open to all the hospital staff continued. In addition, a space was created in the hospital intranet where professionals could consult protocols and the latest information from local and national authorities, and access the latest streaming meetings and other pertinent documentation generated by the hospital.
(iv) Recovery phase, start April 24, 2020The recovery phase started when there was evidence of the remission of the epidemic, with a decrease in the number of admissions below ten patients per day, and a sustained increase in the number of daily discharges. This phase aimed to be a transition towards normality in the hospital. At this point, the transformation strategy focused on structuring the coexistence of COVID-19 and non-COVID-19 activity. The main activities were the reorganisation of the ER and the hospitalisation and ICU wards to increase the number of spaces available for non-COVID-19 patients, the progressive activation of the surgical programme, and the restructuring of outpatient clinics.
Actions to adapt the hospital infrastructure, capacity and taskforce. We introduced new strategies to address the challenge of combining care for patients with COVID-19 with care for patients with other pathologies. All hospitalised patients with COVID-19 were grouped in spatially differentiated areas: the upper floors remained as COVID-19 hospitalisation wards, and the lower ones were progressively re-converted to non-COVID-19 wards. In addition, we increased the number of spaces available to treat non-COVID-19 patients in the ER. The number of ICU wards started to be reduced in order to recover space for surgical procedure, outpatient care and Day Hospital activities. Staff who had been providing support to COVID-19 teams in the ER, ICU and hospital wards progressively returned to their original departments.
Restructuring of outpatient visits. Face-to-face outpatient clinical activity was resumed on May 18. Agglomerations were avoided by limiting the number of patients in waiting rooms. All first consultations were maintained face-to-face. However, follow-up consultations are currently conducted by telemedicine unless the physician considers that a face-to-face appointment is needed.
Infection prevention and control measures. All patients requiring hospital admission or diagnostic tests are tested for COVID-19 by PCR in the previous 48h.
Crisis in numbersDuring the response phases, which amounted to a period of 57 days, 3106 patients consulted the ER at the HUVH and 2054 were admitted, 346 of whom were treated at the ICU.
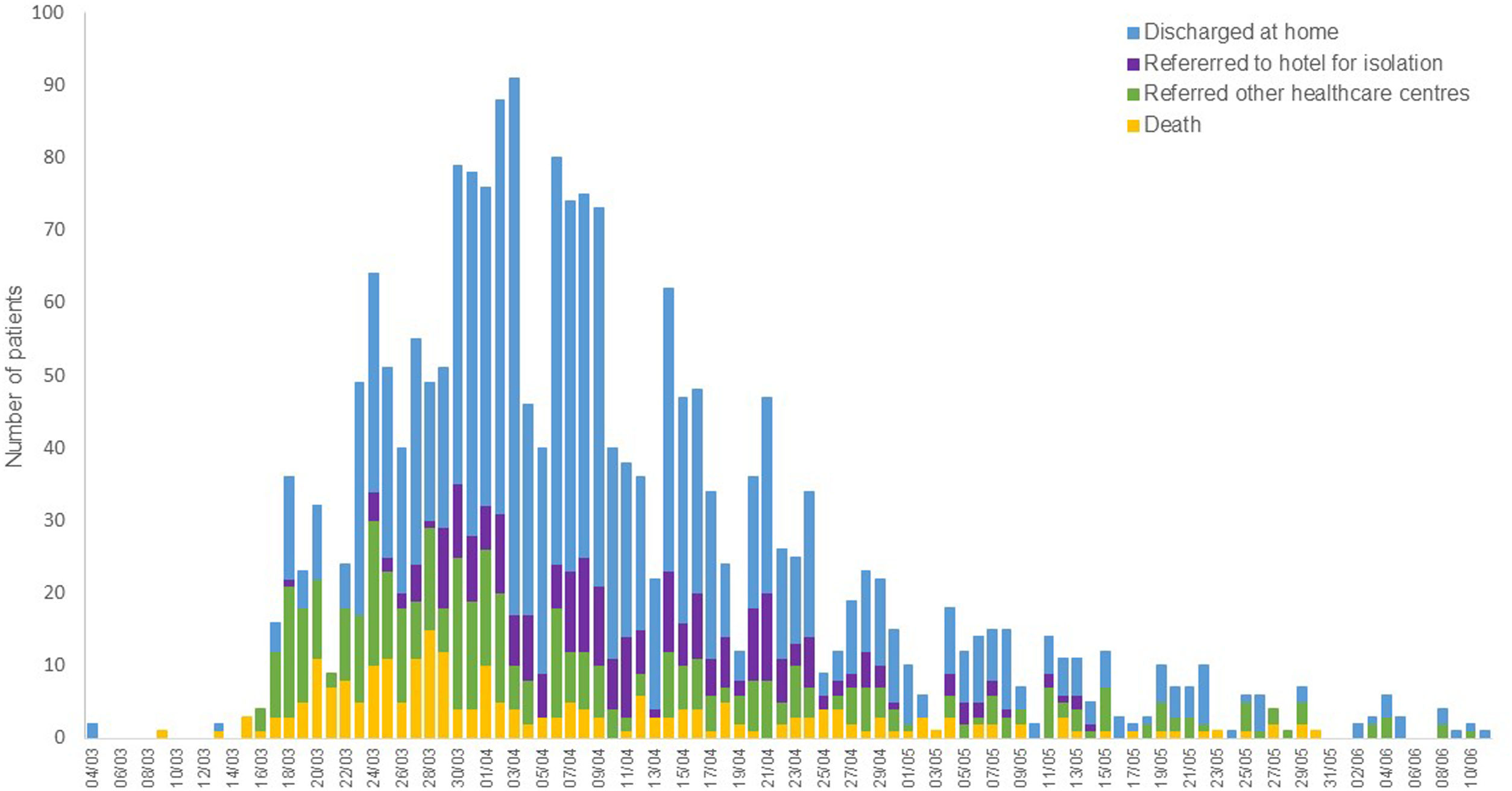
Admissions at the hospitalIn the response phases (February 27 to April 23), a total of 2076 hospitalisations were performed for 2054 patients (Fig. 1). The mean age of hospitalised patients was 60.1 years, and 45.8% were female. At the peak of the epidemic, 626 patients were simultaneously admitted to hospital, 166 of them in the ICU. In total, 1183 patients were discharged home, 250 patients were referred to nearby hotels to guarantee conditions of isolation until their return home was considered safe, 402 patients were referred to other healthcare centres in the area, and eight were still admitted at the end of the period (Fig. 2). In all, 233 patients (11.2%) died in the hospital, with a maximum of 20 patients per day at the peak of the epidemic. Forty discharged patients were readmitted in the following days. Mean length of stay was 10.67 days (22,112 accumulated days). More complicated patients, mainly those transferred to the ICU, had a mean hospital stay of 28.66 days.
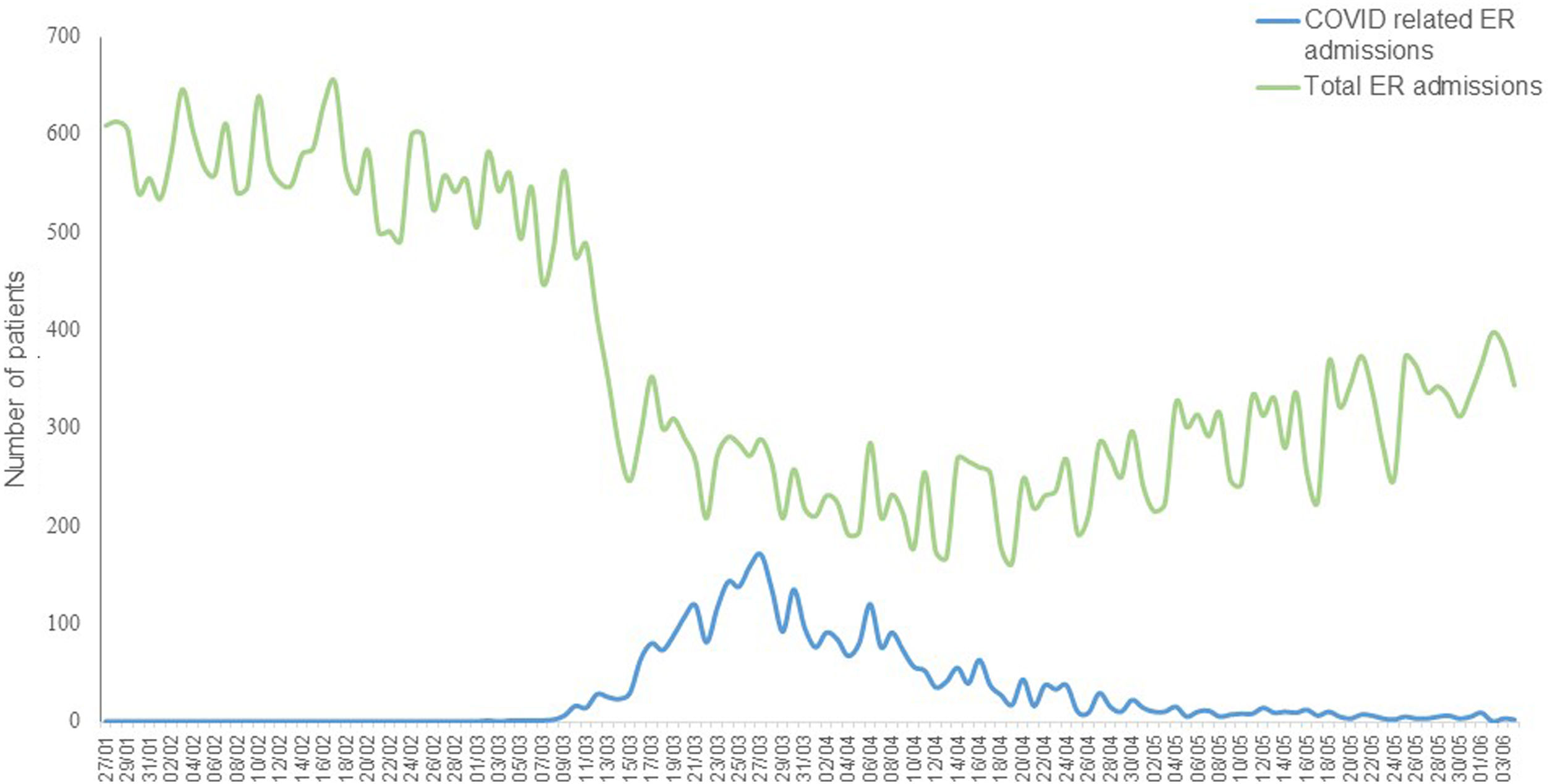
Emergency room admissionsDuring the first 57 days of the response, 3253 ER consultations were made by 3106 patients. Fifty-eight per cent of these consultations resulted in hospital admissions. Also, 19.4% of patients were discharged to their homes and 18.9% were referred to other centres. The percentage of patients who died during the ER stay was 2.2%. The total number of ER admissions was drastically reduced during the pandemic (Fig. 3). Non-related COVID-19 consultations fell during the peak days to a daily mean figure of 112 visits, a decrease of 80.5% in relation to the previous year.
Increase in hospital capacityDuring the intensive response phase, an extra 122 regular beds were provided, 78 in hospital wards and 44 in the Olympic Sports pavilion. In addition, the number of adult ICU beds increased progressively by 371%, from 56 to 208. Eighty-eight extra conventional beds in the pavilion and 65 extra ICU beds were planned, although they were not finally required. Finally, 470 hotel rooms were adapted for COVID-19 patients and health staff.
Human resources approachSix hundred and seventy-one staff members went on sick leave after testing positive for COVID-19 during the response phase. The highest rate of sick leaves was recorded amongst nursing staff (41.3% of total) and auxiliary nursing staff (24.0%), followed by physicians (11.6%) and medical residents (5.2%). Since the beginning of the pandemic, 1110 new staff have been hired, an increase of 13.6% compared with the period prior to COVID-19. By category, recruitment was highest amongst nurses (481 new hires), auxiliary nursing technicians (306 new hires), ancillary staff (141 new hires) and specialist doctors (71 new hires).
Lessons learnedThe maximisation of pre-existing resources is mandatory in the context of a pandemic. A situation of this kind is different to other calamities such as terrorist attacks or natural disasters. In those two situations, external support is possible, since they require only limited space and end in a relatively short time; in contrast, the pandemic situation starts insidiously, may affect the entire world, and can range in length from several weeks to months. Thus, the strategy applied should optimise the use and distribution of the hospital's material and human resources.
The HUVH's approach to guarantee the availability of sufficient resources has been innovative, although some of the strategies deployed have also been reported in other countries in the context of the COVID-19 pandemic.1,6,12 In this regard, territorial coordination is of paramount importance. Instead of rapidly creating temporary hospitals in the territory, as was the case in China,4 our hospital led a coordinated action aimed at making an efficient use of the health and non-health resources already available. A network of public and private facilities and organisations worked together to ensure that patients were attended to in the best place possible according to their specific care needs. Coordination was possible due to the willingness of the various actors for collaborating, and to the firm leadership of the hospital, which from the beginning transmitted the message that the epidemic could only be faced through the joint commitment of all the stakeholders. The experience of this coordination has created a unique opportunity to improve care integration in the area, establish operational flow circuits of patients, improve the data information flow to the professionals, and define the basis for further collaboration for the benefit of patients.
The successful transformation of the HUVH was also possible due to the design of visible and coordinated leadership roles from the start of the pandemic threat. Leadership is recognised as the cornerstone of crisis management,13 and strong management and clinical and scientific leadership roles served to provide consistency, agility and adaptability in the transformation of the hospital as the pandemic unfolded, as observed in other contexts.14 Input from the scientific leaders allowed the management leaders to plan actions and make informed decisions, which were then applied by the clinical leaders in the daily activities of the hospital. The clear definition of the leadership roles and regular communication made possible the prompt deployment of the pandemic response plan... This tripartite division of roles provided a firm foundation on which to carry out transformation processes in the hospital context. In addition, the reorganisation of the existing workforce into multidisciplinary teams made a rapid response possible, due to a clear definition of clinical roles. Nonetheless, the recruitment of new staff was necessary, especially among nurses and auxiliary nurses, because of the high rates of COVID-19-related sick leave among these health care professionals.
After this first wave, we have faced new waves of the pandemic. However, we are now more prepared. New waves were expected, so the hospital continued working on further developing and updating the response plan. In addition, some of the limitations that we faced on the first wave have been addressed, thus streamlining the hospital response capacity. For example, there are stable patient flow channels between the various organizations in the territory, and there is a reserve of beds (ICU and non-ICU) to face a sudden increase in the number of COVID-19 patients admitted at the hospital. In addition, we have now more evidence than before on the epidemiology of the disease that has allowed us to update our plan with more efficient safety measures. However, we also face new threats that must be properly addressed, including the mental exhaustion of professionals and the pressure of non-COVID-19 patients who have had their disease monitoring and treatment postponed for many months.
However, it was needed such a rapid response that leads to extreme decisions such as cancelling elective surgeries and transplantations or not allowing inpatients to have visits of their relatives. After this crisis, we must assess our actions and identify some alternative interventions to develop different strategies to avoid such measures in a future crisis.
All around the world, the COVID-19 pandemic has put health services to the test. In these unprecedented times, innovative strategies allowing the rapid transformation of hospitals are required. The HUVH opted to reorganise its activity based on four central strategies: early planning, territorial coordination involving all the healthcare actors in its reference area, the definition of clear leadership roles, and care organisation focused on multidisciplinary teams with only small increases in staff. As a result, we were able to cope with the surge of COVID-19 patients accessing the hospital, without ever reaching a collapse situation, since several actions to increase the number of available beds were progressively deployed, including the cancellation of non-urgent activities, such as elective surgery. The crisis is not yet over, but the adaptability shown by the hospital raises confidence in its ability to face possible large-scale health emergencies in the future. This crisis has also served to highlight deficiencies or areas for improvement in the hospital, such as the need of disposing of additional structural spaces to respond to punctual increases in demand for hospital beds.
FundingThe research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interestWe declare no competing interests.
The authors would like to thank all the staff from Vall d’Hebron and its nearby territory for all their effort, understanding and dedication in these uncertain, hard times.