Las estatinas, fármacos utilizados fundamentalmente por su efecto hipocolesterolemiante, parecen tener efectos inmunomoduladores, antioxidativos, anticoagulantes y antimicrobianos.
ObjetivoAnalizar el impacto del uso prehospitalario de las estatinas sobre la presentación y el pronóstico de la sepsis.
DiseñoEstudio observacional prospectivo de 1.042 pacientes sépticos en una unidad de cuidados intensivos (UCI) de un hospital de tercer nivel, durante un periodo de 5 años.
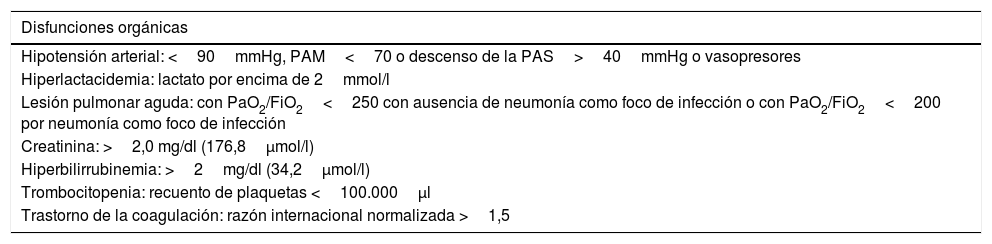
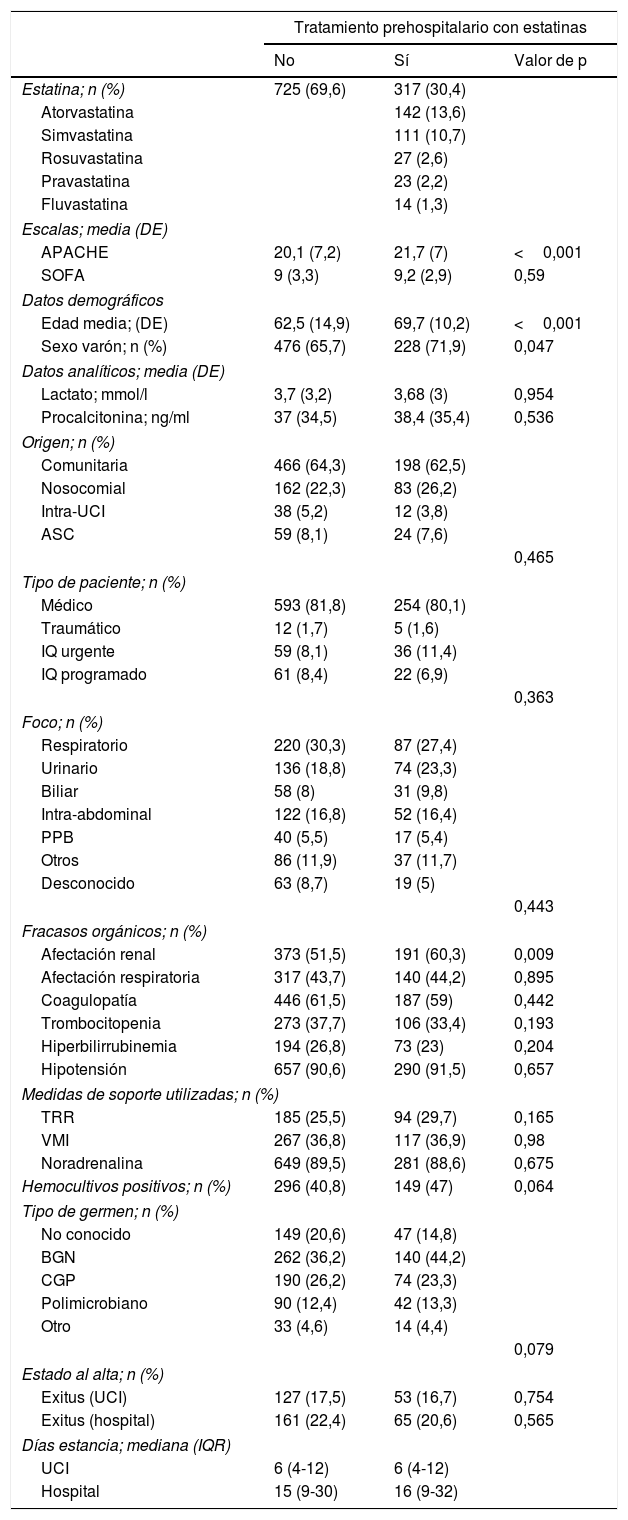
ResultadosTrescientos diecisiete (30,4%) pacientes sépticos recibían estatinas prehospitalariamente, siendo mayor el porcentaje de varones (71,9 versus 65,7%; p=0,047), la edad (69,7 años versus 62,5; p<0,001) y Acute Physiology and Chronic Health Evaluation (APACHE) II (21,7 versus 20,1; p<0,001), respecto a los que no las tomaban. Presentaron, al ingreso, una proporción superior de afectación renal (60,3 versus 51,5%; p=0,009), sin mayor requerimiento de técnicas de reemplazo renal (TRR). No objetivamos diferencias en Secuencial Organ Failure Assessment (SOFA), procalcitonina, foco, tipo de microorganismo, porcentaje de sepsis nosocomiales, mortalidad ni días de estancia intra-UCI ni hospitalaria global.
ConclusiónEl uso prehospitalario de estatinas no influyó significativamente en la presentación y el pronóstico de la sepsis.
In addition to being effective at lowering cholesterol, statins seem to have immunomodulatory, antimicrobial, antioxidant and anticoagulant effects.
ObjectiveTo determine whether the presentation of sepsis and its outcome in patients who have had prehospital statin therapy are different.
MethodsA prospective, observational study was carried out on 1042 septic patients, for 5 consecutive years in the Intensive Care Unit (ICU) of a tertiary hospital.
Results317 (30.4%) septic patients were receiving statins prior to hospitalization. Patients on statin therapy were older (69.7 years old vs 62.5; p <.001), males (71.9% vs 65.7%; p=.047) and with a higher mean Acute Physiology and Chronic Health Evaluation (APACHE) II score (21.7 vs 20.1; p<.001). Renal dysfunction was observed in a greater proportion (60.3% vs 51.5%; p=.009) in statin users but without requiring more continuous renal replacement therapies (CRRT). No differences were observed in Sequential Organ Failure Assessment (SOFA) score, procalcitonin levels, source of infection, microorganism and nosocomial infections in ICU and hospital mortality or length of stay.
ConclusionsStatin therapy prior to hospitalization does not significantly influence sepsis presentation or sepsis outcomes.