Immune thrombocytopenia (ITP) is a potentially severe manifestation of systemic lupus erythematosus (SLE) reported in 7–40% of SLE patients. ITP has been associated with a higher risk of organ damage and mortality.
ObjectivesTo describe which factors are associated with the presence of ITP in SLE patients.
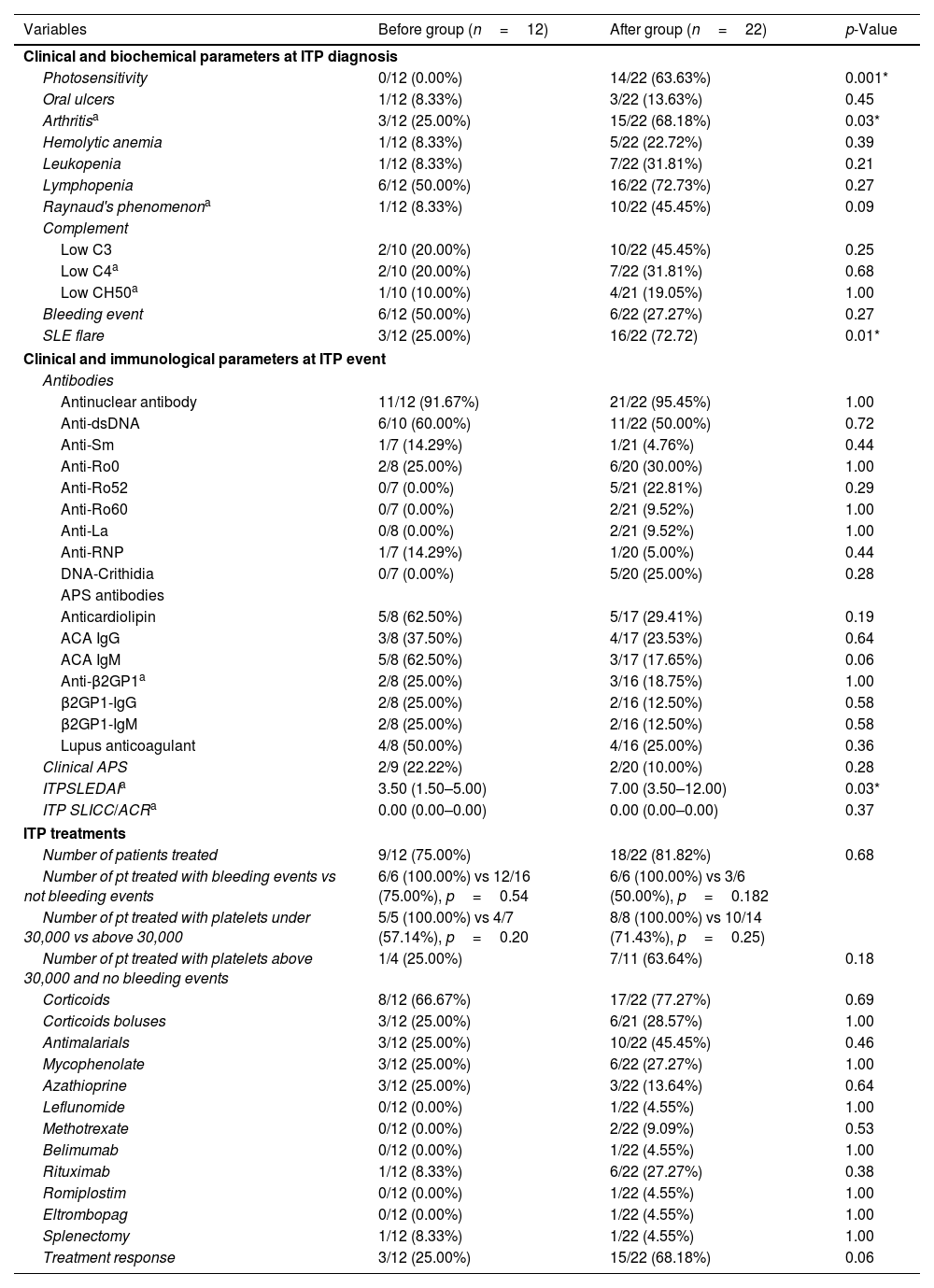
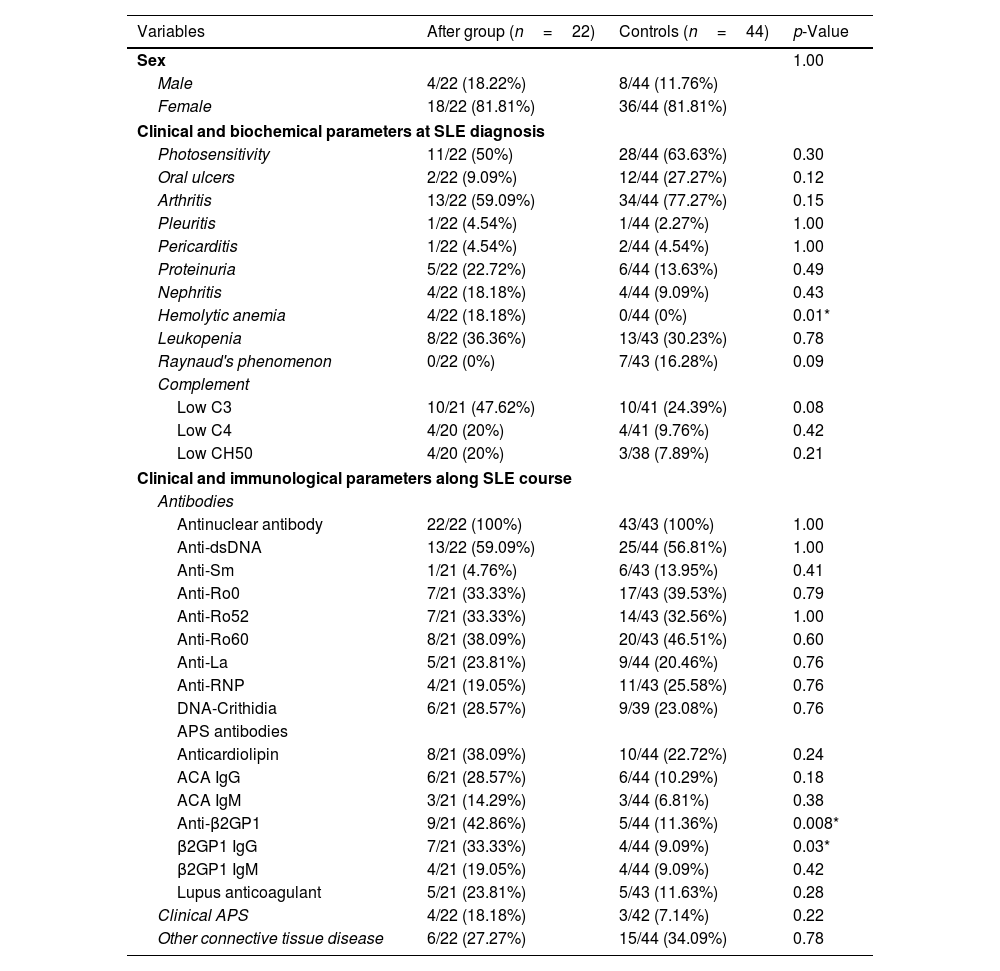
MethodsRetrospective case–control study. Cases were defined as SLE patients who had ever developed ITP and were sex- and age-matched with two controls. A predictive model was constructed to identify SLE patients who were at risk of developing ITP.
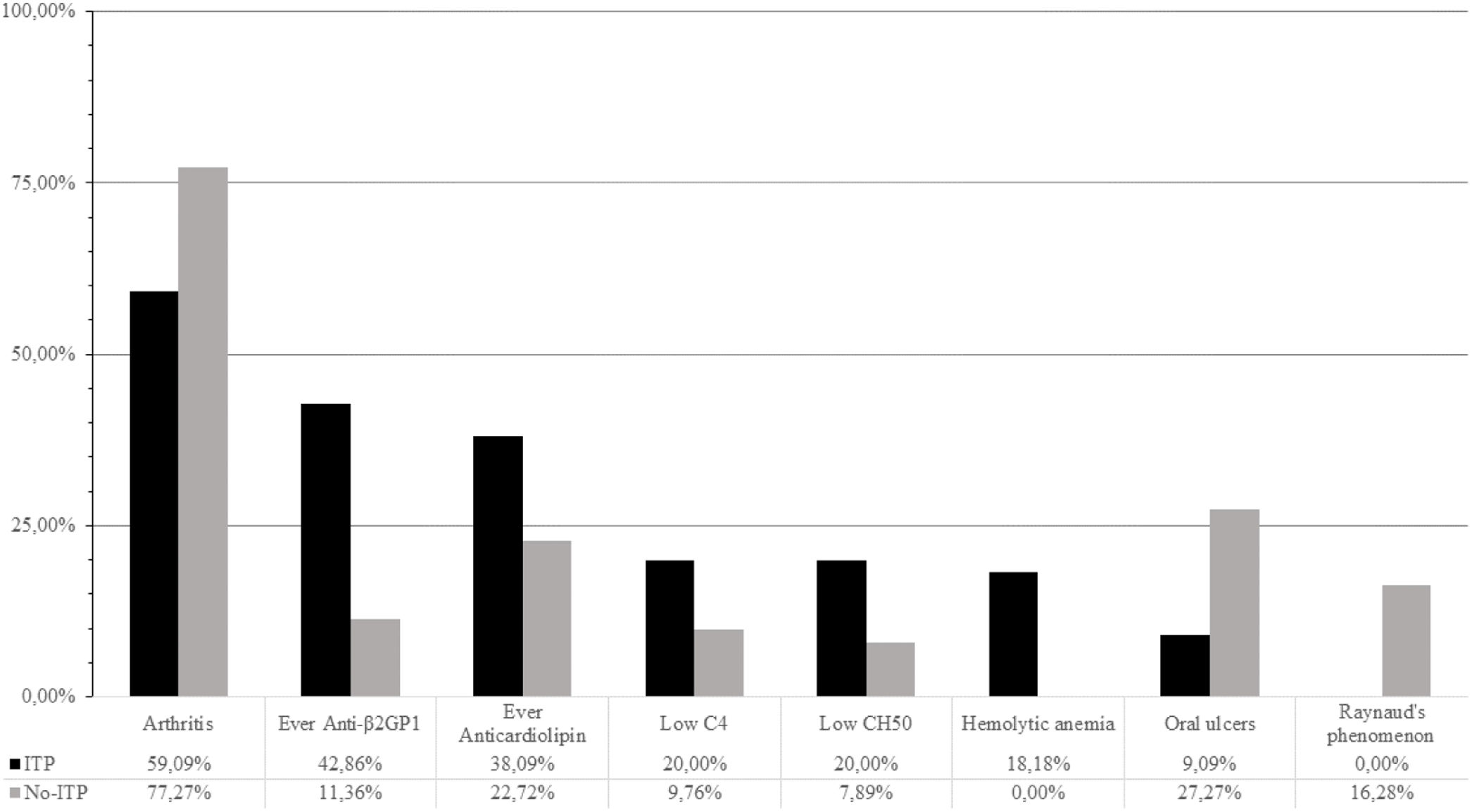
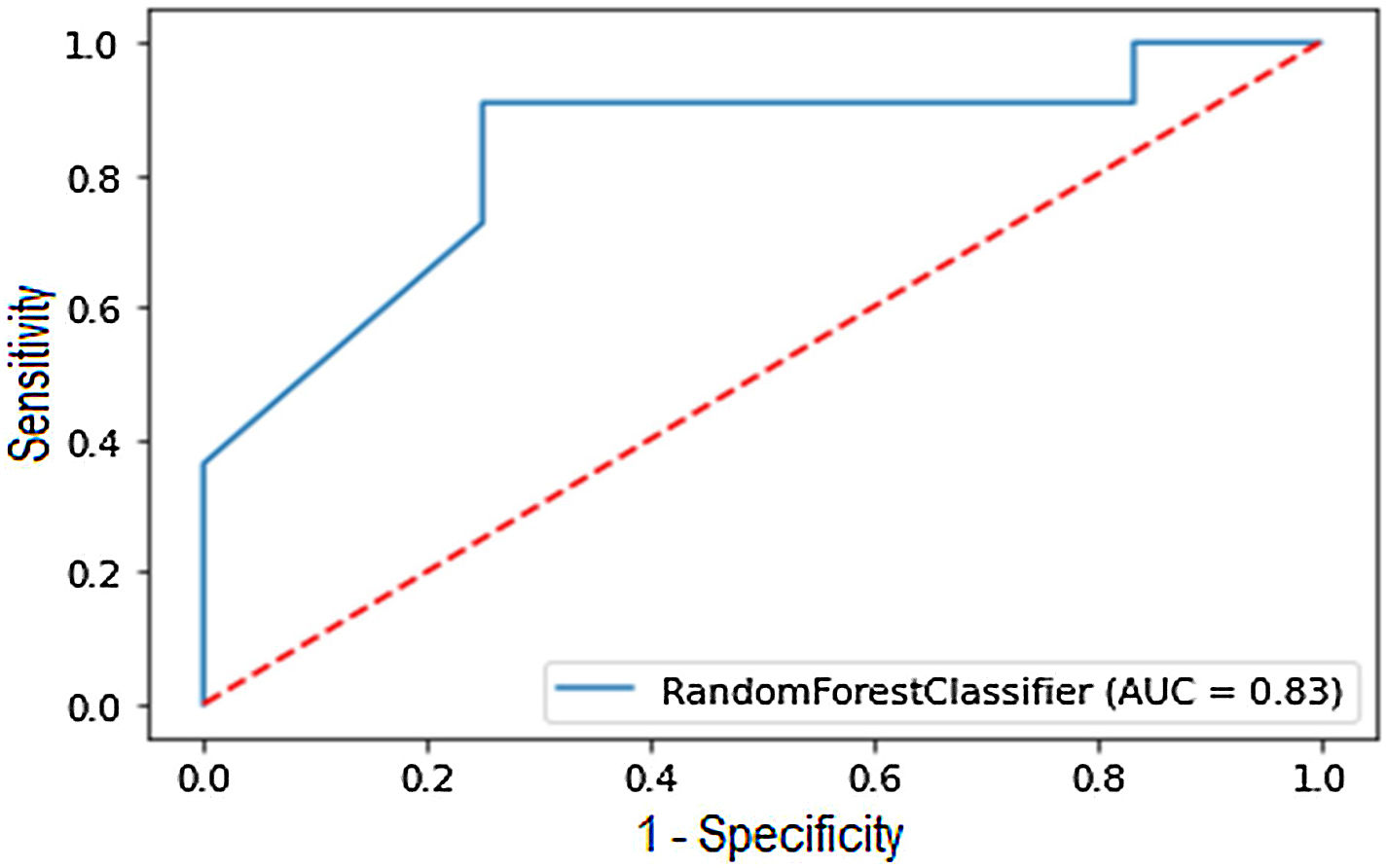
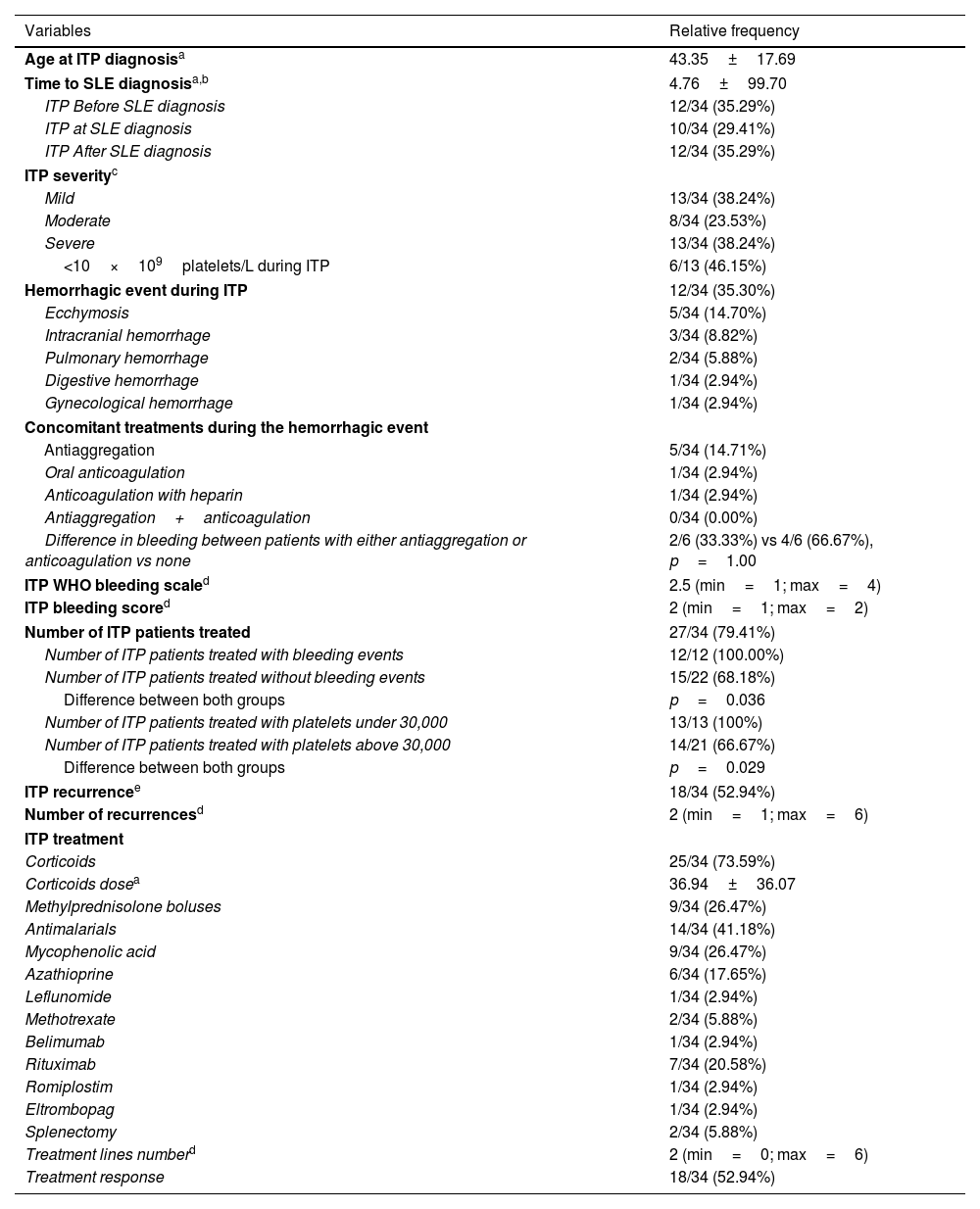
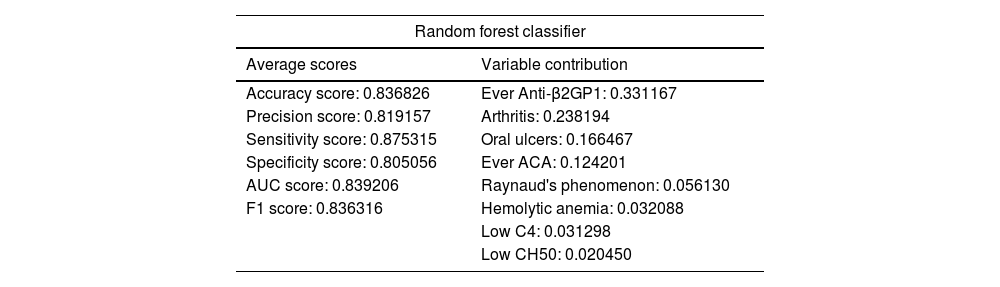
ResultsITP prevalence in our SLE cohort was 8.35%. Cases had a higher frequency of hemolytic anemia, while controls had a higher prevalence of arthritis at SLE diagnosis. During SLE progression, cases tested positive for anticardiolipin, anti-β2-glycoprotein 1, and lupus anticoagulant antibodies more frequently. Cases received mycophenolic acid and azathioprine more often than controls and had a higher SLICC/ACR score. The model demonstrated a sensitivity of 87.53%, a positive predictive value of 81.92%, a specificity of 80.50%, area under the curve of 83.92%, a F1 of 83% and an overall accuracy of 83.68%. The variables that best explain the model were hemolytic anemia, arthritis, oral ulcers, Raynaud's phenomenon, low C4, low CH50, anticardiolipin and anti-β2GP1 antibodies.
ConclusionSLE patients who develop ITP have a distinct phenotype characterized by more hemolytic anemia and less arthritis at SLE onset, and higher prevalence of antiphospholipid syndrome antibodies during SLE progression. This phenotype is associated with heightened organ damage and the need for more intensive therapies and stricter follow-up. Our predictive model has demonstrated an impressive ability to identify SLE patients at risk of developing ITP.
La trombocitopenia inmunitaria (TI) es una manifestación potencialmente grave del lupus eritematoso sistémico (LES) reportada en el 7-40% de los pacientes con LES. La TI se ha asociado con un mayor riesgo de daño orgánico y mortalidad.
Objetivos Describir qué factores se asocian con la presencia de TI en pacientes con LES.
MétodosEstudio retrospectivo de casos y controles. Los casos se definieron como pacientes con LES que alguna vez habían desarrollado TI y fueron emparejados por sexo y edad con 2 controles. Se construyó un modelo predictivo para identificar pacientes con LES que tenían riesgo de desarrollar TI.
ResultadosLa prevalencia de TI en nuestra cohorte de LES fue del 8,35%. Los casos tenían una mayor frecuencia de anemia hemolítica, mientras que los controles tenían una mayor prevalencia de artritis en el momento del diagnóstico de LES. Durante la progresión del LES, los casos dieron positivo para anticuerpos anticardiolipina, anti-β2-glucoproteína 1 y anticoagulante lúpico con mayor frecuencia. Los casos recibieron ácido micofenólico y azatioprina con más frecuencia que los controles y tuvieron una puntuación SLICC/ACR más alta. El modelo demostró una sensibilidad del 87,53%, un valor predictivo positivo del 81,92%, una especificidad del 80,50%, un área bajo la curva del 83,92%, una F1 del 83% y una precisión general del 83,68%. Las variables que mejor explican el modelo fueron anemia hemolítica, artritis, úlceras bucales, fenómeno de Raynaud, C4 bajo, CH50 bajo y anticuerpos anticardiolipina y anti-β2-glucoproteína 1.
ConclusiónLos pacientes con LES que desarrollan TI tienen un fenotipo distinto caracterizado por más anemia hemolítica y menos artritis al inicio del LES, y una mayor prevalencia de anticuerpos contra el síndrome antifosfolípido durante la progresión del LES. Este fenotipo se asocia con un mayor daño orgánico y la necesidad de tratamientos más intensivos y un seguimiento más estricto. Nuestro modelo predictivo ha demostrado una capacidad impresionante para identificar pacientes con LES en riesgo de desarrollar TI.