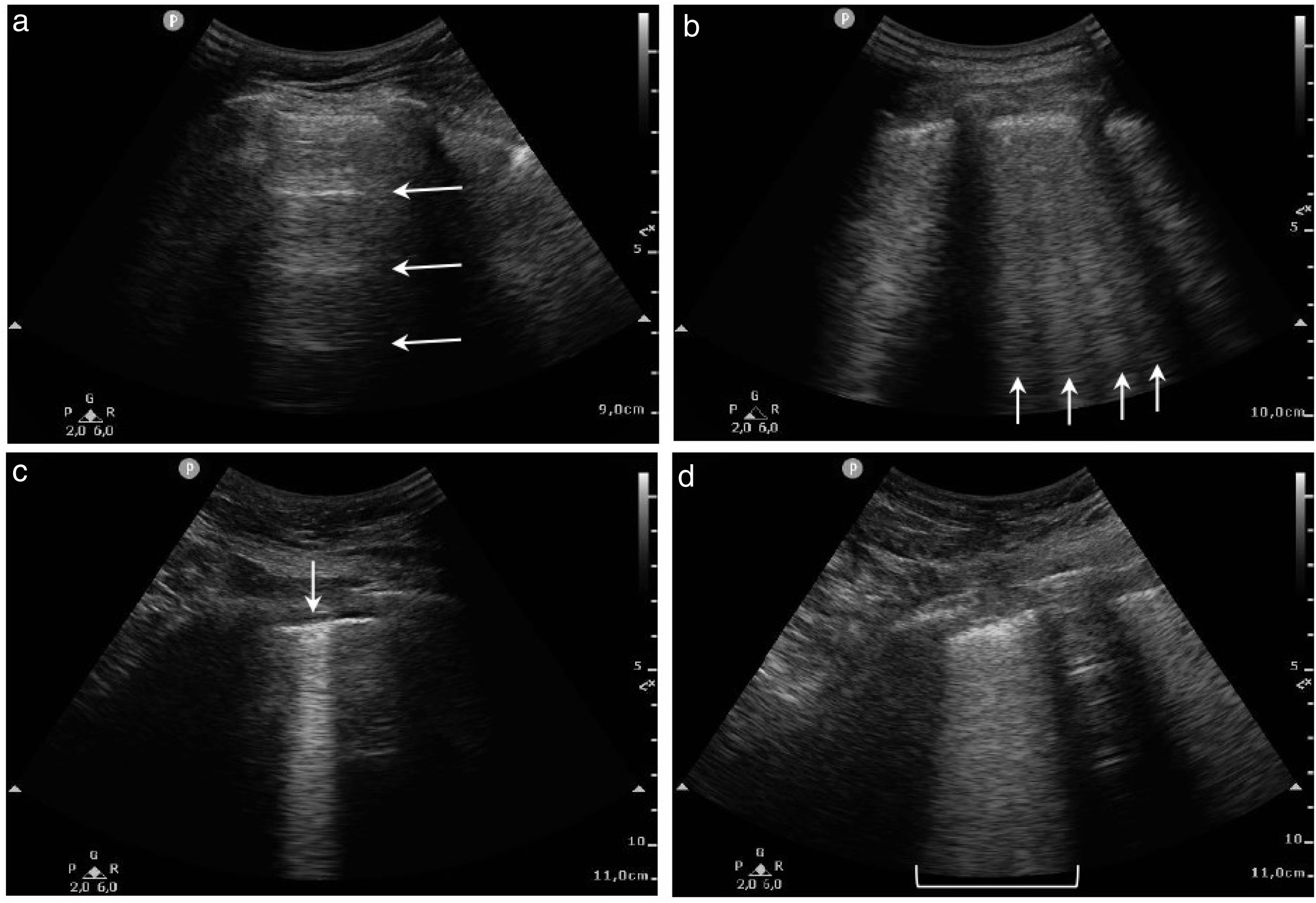
Our purpose was to establish different cut-off points based on the lung ultrasound score (LUS) to classify COVID-19 pneumonia severity.
MethodsInitially, we conducted a systematic review among previously proposed LUS cut-off points. Then, these results were validated by a single-centre prospective cohort study of adult patients with confirmed SARS-CoV-2 infection. Studied variables were poor outcome (ventilation support, intensive care unit admission or 28-days mortality) and 28-days mortality.
ResultsFrom 510 articles, 11 articles were included. Among the cut-off points proposed in the articles included, only the LUS>15 cut-off point could be validated for its original endpoint, demonstrating also the strongest relation with poor outcome (odds ratio [OR]=3.636, confidence interval [CI] 1.411–9.374). Regarding our cohort, 127 patients were admitted. In these patients, LUS was statistically associated with poor outcome (OR=1.303, CI 1.137–1.493), and with 28-days mortality (OR=1.024, CI 1.006–1.042). LUS>15 showed the best diagnostic performance when choosing a single cut-off point in our cohort (area under the curve 0.650). LUS≤7 showed high sensitivity to rule out poor outcome (0.89, CI 0.695–0.955), while LUS>20 revealed high specificity to predict poor outcome (0.86, CI 0.776–0.917).
ConclusionsLUS is a good predictor of poor outcome and 28-days mortality in COVID-19. LUS≤7 cut-off point is associated with mild pneumonia, LUS 8–20 with moderate pneumonia and ≥20 with severe pneumonia. If a single cut-off point were used, LUS>15 would be the point which better discriminates mild from severe disease.
Establecer diferentes puntos de corte basados en el Lung Ultrasound Score (LUS) para clasificar la gravedad de la neumonía COVID-19.
MétodosInicialmente, realizamos una revisión sistemática entre los puntos de corte LUS propuestos previamente. Estos resultados fueron validados por una cohorte prospectiva unicéntrica de pacientes adultos con infección confirmada por SARS-CoV-2. Las variables analizadas fueron la mala evolución y la mortalidad a los 28 días.
ResultadosDe 510 artículos, se incluyeron 11. Entre los puntos de corte propuestos en los artículos incluidos, solo LUS>15 pudo ser validado para su objetivo original, demostrando también la relación más fuerte con mala evolución (odds ratio [OR]=3,636, intervalo de confianza [IC] 1,411-9,374). Respecto a nuestra cohorte, se incluyeron 127 pacientes. En estos pacientes, el LUS se asoció estadísticamente con mala evolución (OR=1,303, IC 1,137-1,493) y con mortalidad a los 28 días (OR=1,024, IC 1,006-1,042). LUS>15 mostró el mejor rendimiento diagnóstico al elegir un único punto de corte en nuestra cohorte (área bajo la curva 0,650). LUS≤7 mostró una alta sensibilidad para descartar mal resultado (0,89, IC 0,695-0,955), mientras que LUS>20 reveló gran especificidad para predecir mala evolución (0,86, IC 0,776-0,917).
ConclusionesLUS es un buen predictor de mala evolución y mortalidad a 28 días en COVID-19. LUS≤7 se asocia con neumonía leve, LUS 8-20 con neumonía moderada y ≥20 con neumonía grave. Si se utilizara un único punto de corte, LUS>15 sería el que mejor discriminaría la enfermedad leve de la grave.