Se han descrito diferencias pronósticas entre portadores y no portadores de catéter venoso central (CVC) con trombosis venosa profunda de miembros superiores (TVPMS), pero la evidencia en los pacientes hospitalizados es limitada.
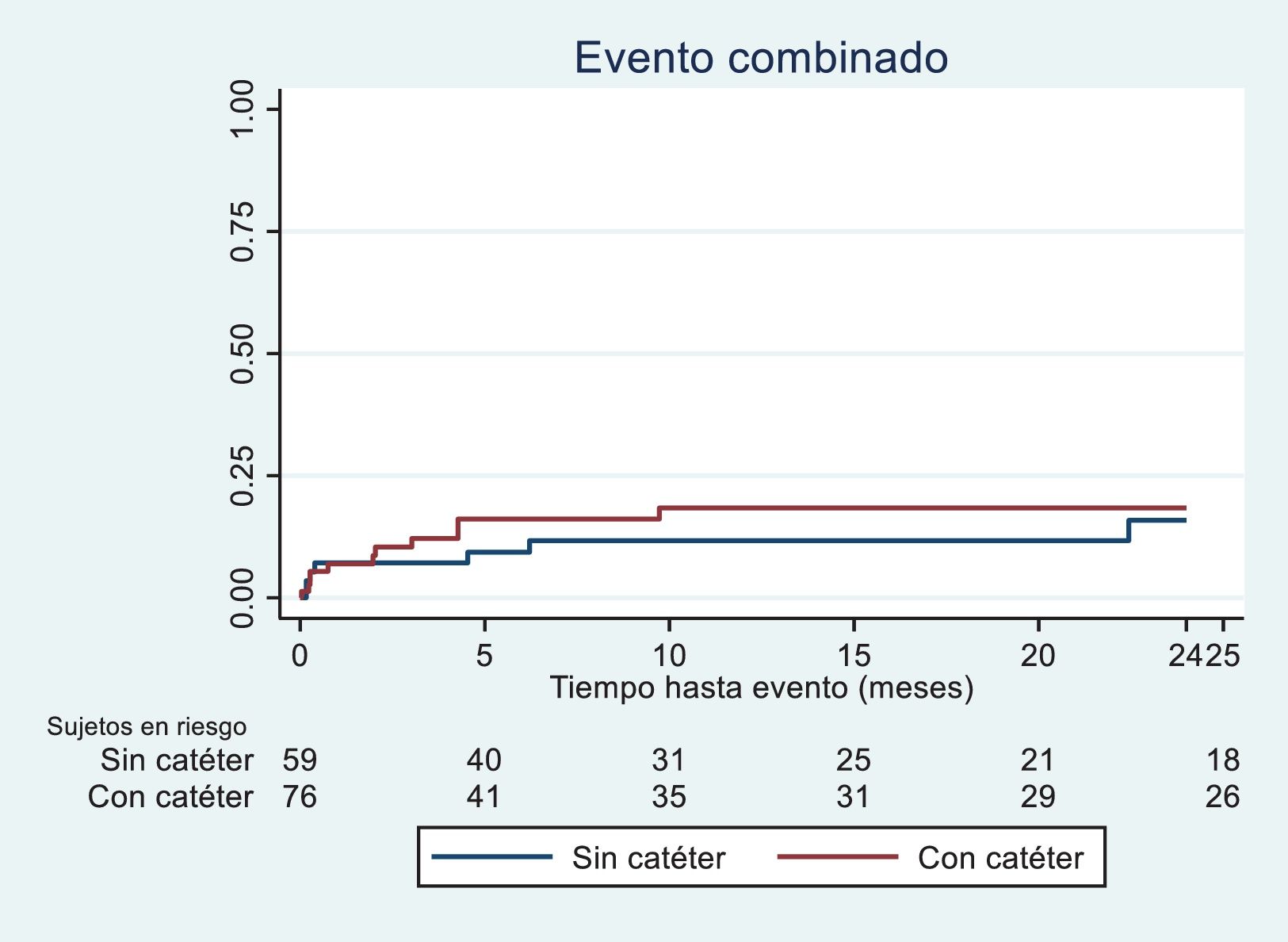
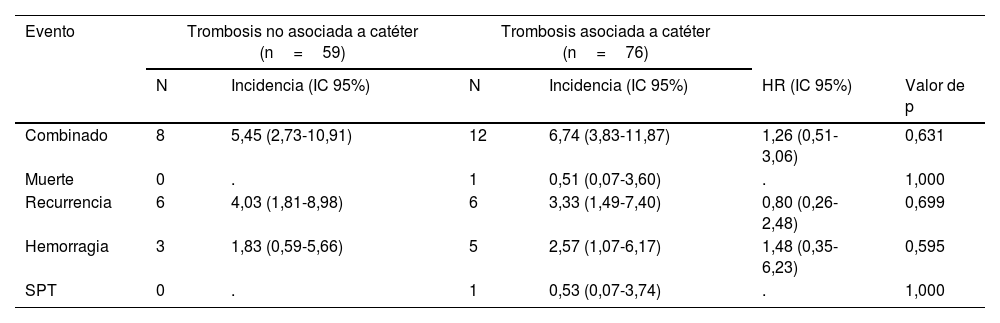
Material y métodoEstudio de cohortes retrospectivo con pacientes ingresados entre marzo de 2012 y marzo de 2023 con TVPMS, asociada a CVC (TAC) y no asociada a CVC (TNAC). Se analizaron las tasas de recurrencia trombótica, hemorragia, síndrome postrombótico y muerte por embolia pulmonar usando curvas de Kaplan-Meier y modelos de riesgos proporcionales de Cox.
ResultadosSe incluyeron 135 pacientes (76 con CVC y 59 sin CVC), con una edad media de 67±15 años y un 44% de mujeres. No se observaron diferencias significativas en la incidencia del evento combinado entre los grupos TNAC y TAC (5,45 vs. 6,74 por 1.000 pacientes/mes, respectivamente (HR: 1,26; IC 95%: 0,51-3,06). Tras ajuste multivariable, no se detectaron diferencias significativas en el riesgo (HR: 1,09; IC 95%: 0,44-2,72).
ConclusionesNo se confirman diferencias pronósticas significativas entre los pacientes portadores y no portadores de CVC ingresados por TVPMS.
Prognostic differences between central venous catheters (CVC) carriers and non-carriers, who have upper extremity deep vein thrombosis (UEDVT), have been described; however, evidence in hospitalized patients is limited.
Materials and methodsThis retrospective cohort study included hospitalized patients from March 2012 to March 2023 with UEDVT, classified into CVC-associated and non-CVC-associated UEDVT groups. Rates of thrombotic recurrence, hemorrhage, post-thrombotic syndrome, and death from pulmonary embolism were analyzed using Kaplan-Meier curves and Cox proportional hazards models.
ResultsA total of 135 patients were included (76 with CVC and 59 without CVC), with a mean age of 67±15 years and 44% female. No significant differences were observed in the incidence of the combined endpoint between CVC non-carriers and carriers (5.45 vs 6.74 per 1000 patient-months respectively; HR: 1.26; 95% CI: 0.51-3.06). After multivariable adjustment, no significant differences in risk were detected (HR: 1.09; 95% CI: 0.44-2.72).
ConclusionsThere are no significant prognostic differences between patients with and without CVC hospitalized for UEDVT.