Journal Information
Vol. 161. Issue 7.
Pages 316-317 (October 2023)
Share
Download PDF
More article options
Vol. 161. Issue 7.
Pages 316-317 (October 2023)
Letter to the Editor
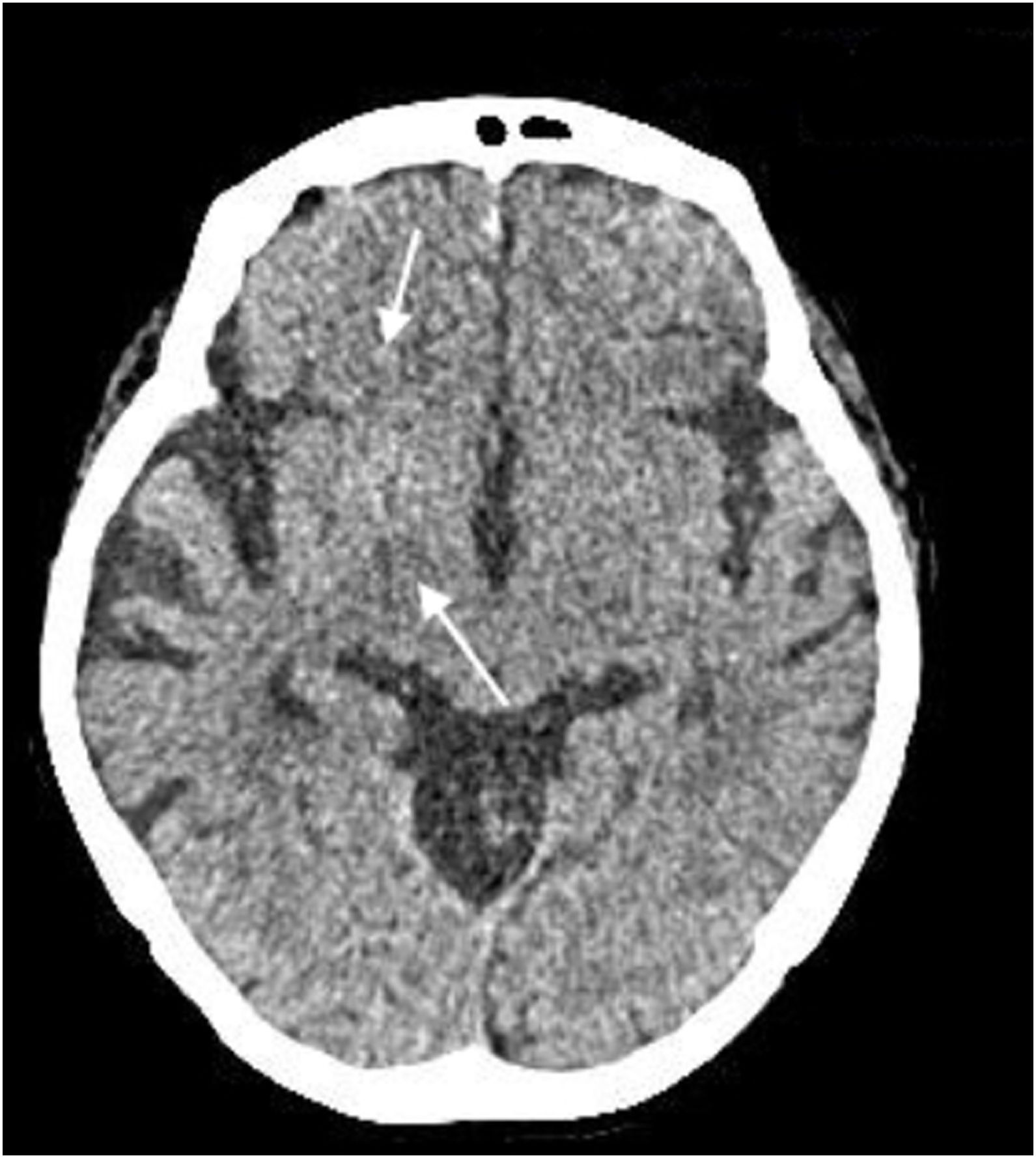
Chorea hyperglycemia basal ganglia syndrome
Síndrome de corea hiperglucémica de ganglios basales
Joaquín Valle Alonso
, Leandro Noblia Gamba, Esther Montoro Jorquera
Corresponding author
Servicio de Urgencias, Hospital Universitario Santa Lucia, Cartagena, Spain
Article information
These are the options to access the full texts of the publication Medicina Clínica (English Edition)
Subscriber
Subscribe
Purchase
Contact
Phone for subscriptions and reporting of errors
From Monday to Friday from 9 a.m. to 6 p.m. (GMT + 1) except for the months of July and August which will be from 9 a.m. to 3 p.m.
Calls from Spain
932 415 960
Calls from outside Spain
+34 932 415 960
E-mail