The characteristics and outcomes of patients with subsyndromatic delirium (SSD) at hospitalization are still under discussion. The objectives were to describe the incidence of delirum and SSD in the intensive care unit care (ICU), to analyze the association with risk factors and to explore outcomes of delirium and subsyndromal delirium (SSD) at hospitalization and three months after discharge.
Patients and methodsA prospective study, with telephone follow-up three months after discharge. The study included 270 patients over one year. Delirium and SSD were assessed with the CAM-ICU.
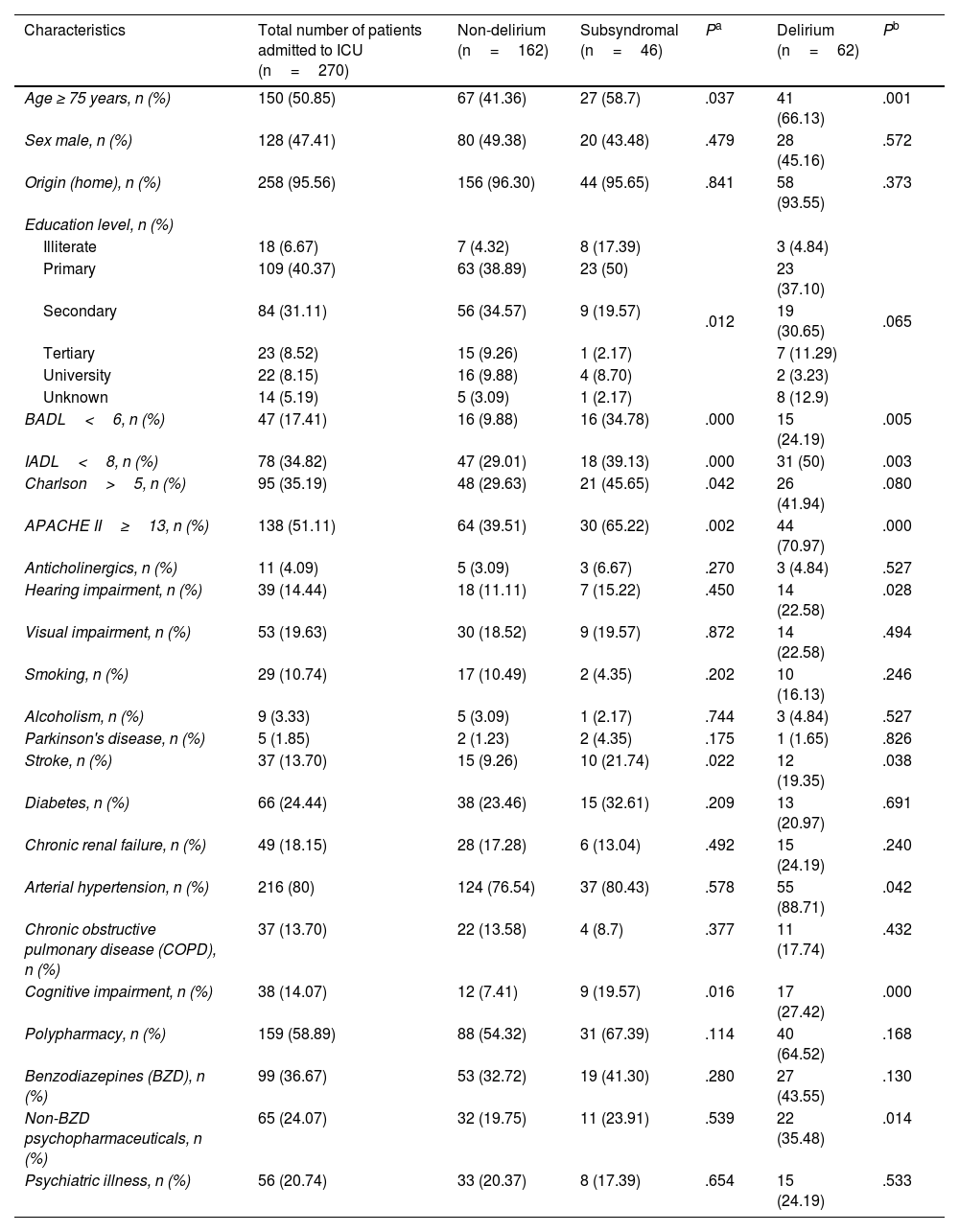
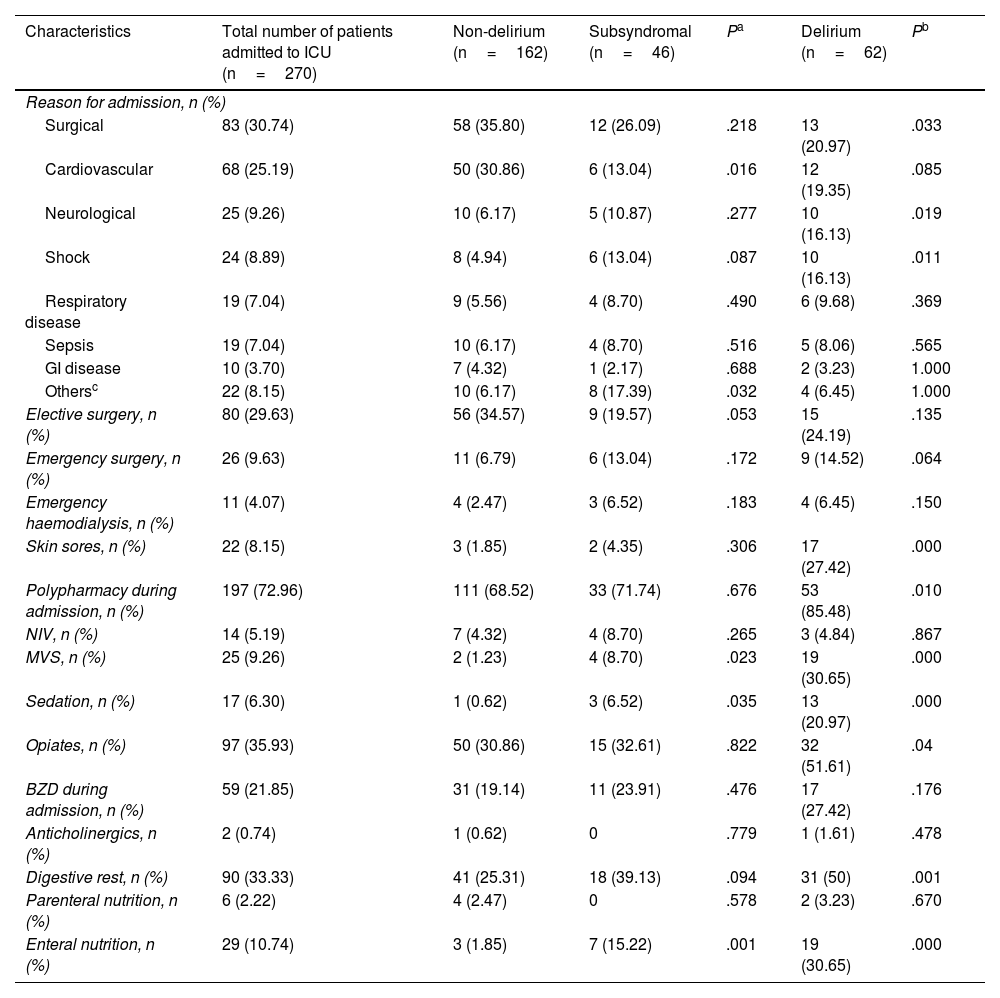
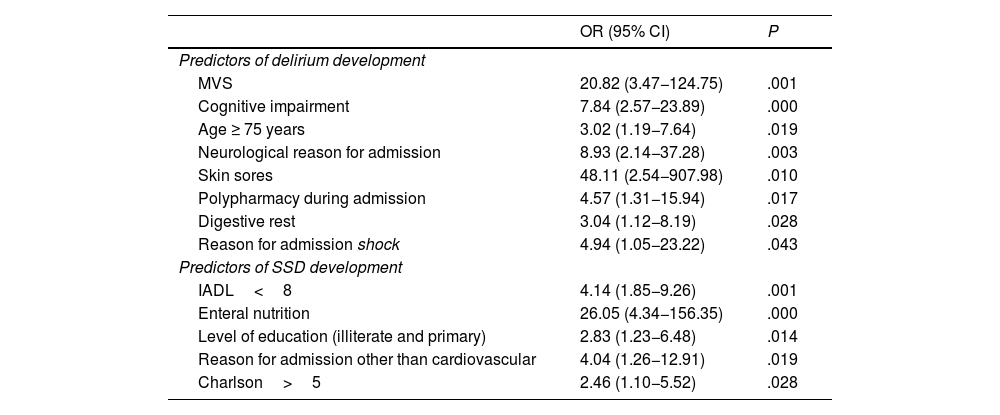
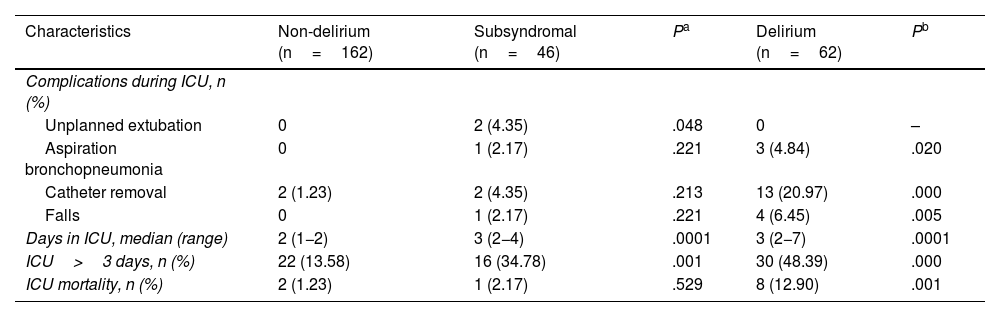
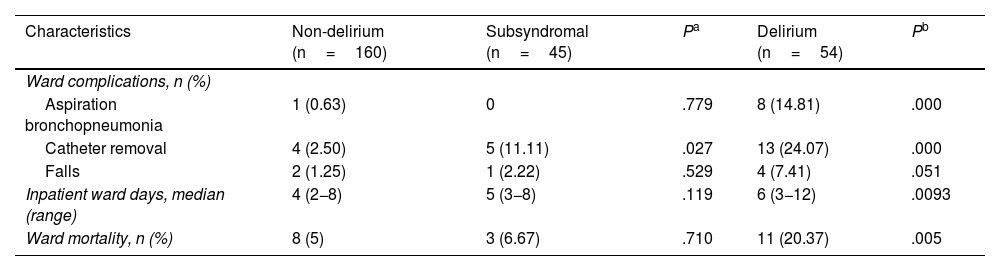
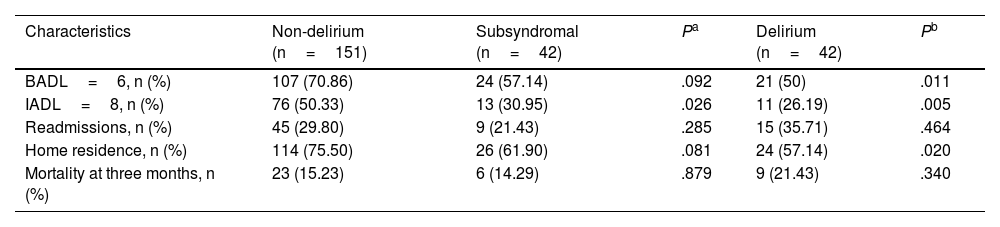
Results22.96% developed delirium and 17.03% SSD. The main risk factors associated with the development of delirium were cognitive impairment (P=.000), age≥75 years (P=.019), neurological admission (P=.003), shock (P=.043), bedsores (P=.010), polypharmacy (0.017), ARM (P=.001) and fast (P=.028) and with the development of SSD were low schooling (P=.014), charlson>5 (P=.028), AIVD<8 (P=.001), enteral feeding (P=.000) and non-cardiovascular admission (P=.019). Overall mortality was 6% in the group without delirium (reference), 8% in SSD (P=.516) and 30% in delirium (P=.000). Median ICU length of stay was 2 (IQR, 1−2) days in the group without delirium, 3 (IQR, 2−4) days in SSD (P=.0001), and 3 (IQR, 2−7) days in delirium group (P=.0001). Three months after discharge, instrumental ADL were preserved in 50% of the group without delirium, 30% of SSD (P=.026) and 26% of delirium (P=.005).
ConclusionsThe SSD group presented an intermediate prognosis between no delirium and delirium groups. It is advisable to promote its diagnosis for better risk classification.
Las características y evolución de pacientes con confusional subsindromático (CSS) en la internación aún continúa en discusión. El objetivo fue describir la incidencia de síndrome confusional agudo (SCA) y CSS en terapia intensiva (UTI), analizar su asociación con la presencia de factores de riesgo y explorar diferencias en la evolución hospitalaria y a los tres meses del alta.
Pacientes y métodosEstudio prospectivo con seguimiento telefónico tres meses luego del alta. Se aplicó el CAM-ICU para definir tres grupos: sin delirio (de referencia), CSS y SCA.
ResultadosEn 270 pacientes, 22,96% presentó SCA y 17,03% CSS. Factores relacionados con mayor riesgo de SCA: deterioro cognitivo (P=,000), edad≥75 años (P=,019), motivo de ingreso neurológico (P=,003), shock (P=,043), escaras (P=,010), polifarmacia (0,017), ARM (P=,001) y reposo digestivo (P=,028); con mayor riesgo de CSS: baja escolaridad (P=,014), Charlson>5 (P=,028), AIVD<8 (P=,001), alimentación enteral (P=,000) y motivo de ingreso no cardiovascular (P=,019). La mortalidad global fue de 6% en el grupo sin delirio, 8% en CSS (P=,516) y 30% en SCA (P=,000). La mediana de internación en UTI fue de 2 días (rango 1−2) en el grupo sin delirio, 3 (2−4) días en CSS (P=,0001) y 3 (2−7) días en SCA (P=,0001). A 3 meses del alta, las AIVD estaban conservadas en el 50% del grupo sin delirio, 30% de CSS (P=,026) y 26% de SCA (P=,005).
ConclusionesEl CSS presentó un pronóstico intermedio entre el grupo sin delirio y el SCA. Se aconseja su diagnóstico para mejor clasificación de riesgo.