Severe influenza is often associated with bacterial coinfection and can trigger sepsis, which increases the severity, complexity and mortality of the disease. To determine an effective method for predicting 28-day mortality of emergency department (ED) patients with influenza, we investigated the Mortality in Emergency Department Sepsis (MEDS) score, procalcitonin (PCT) and other relevant biomarkers.
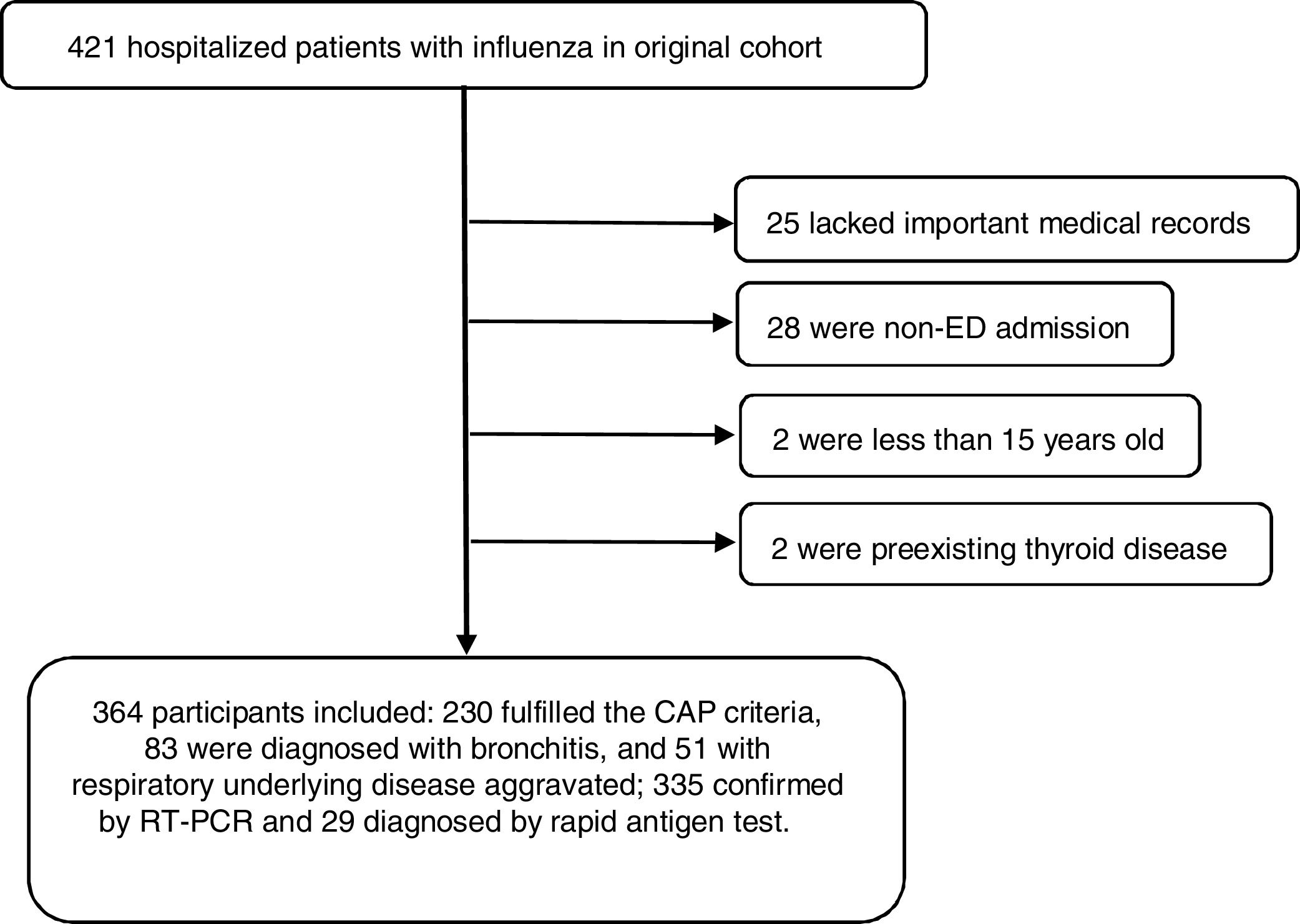
MethodsWe conducted a retrospective, observational, monocentric study, and the endpoint was 28-day mortality. Independent predictors were identified and a new combination predictive model was created both by logistic regression, and the model was evaluated by a receiver operating characteristic (ROC) curve.
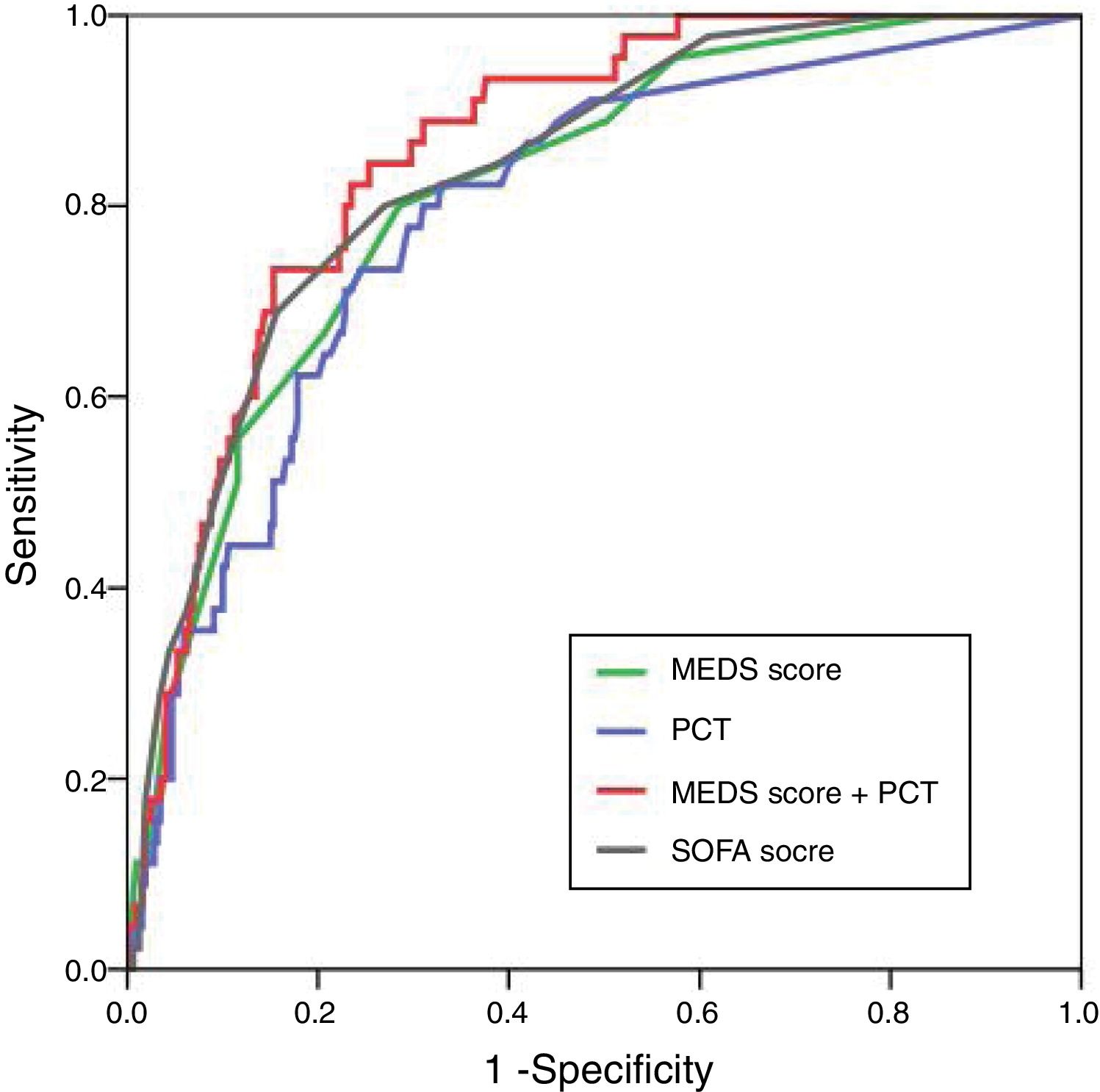
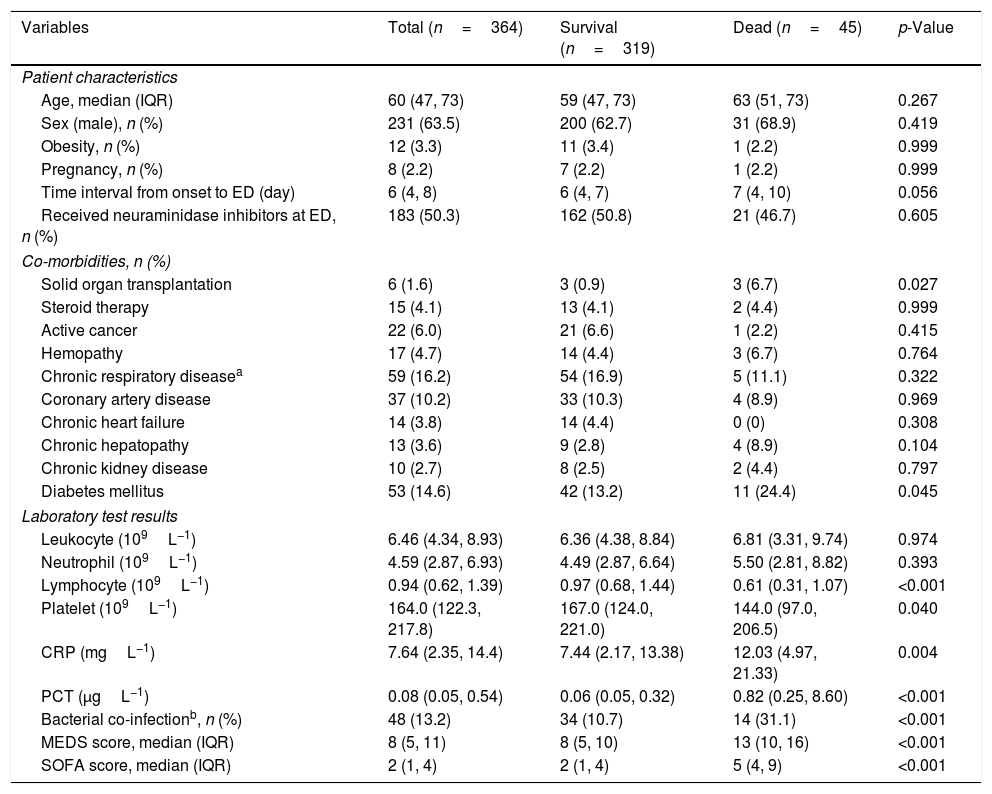
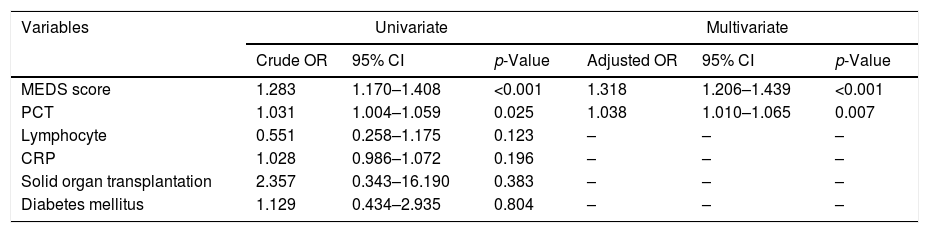
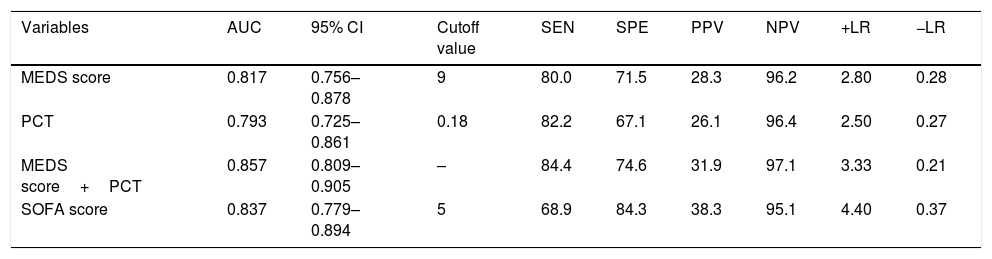
ResultsA total of 364 consecutive ED admitted patients with influenza were enrolled and 45 patients died within 28 days. For predicting 28-day mortality, the MEDS score and PCT were independent predictors with adjusted odds ratio of 1.318 (95% CI 1.206–1.439) and 1.038 (95% CI 1.010–1.065), and with AUCs of 0.817 (95% CI 0.756–0.878) and 0.793 (95% CI 0.725–0.861), respectively. The new combination of the MEDS score with PCT significantly improved the efficacy for predicting 28-day mortality with an AUC of 0.857 (95% CI 0.809–0.905), and was superior to the SOFA score with an AUC of 0.837 (95% CI 0.779–0.894).
ConclusionThe MEDS score and PCT, especially when combined, perform well for predicting mortality of ED admitted patients with influenza.
La gripe severa se asocia a menudo a la coinfección bacteriana, pudiendo desencadenar sepsis, lo cual incrementa la gravedad, la complejidad y la mortalidad de la enfermedad. Para determinar un método efectivo de predecir la mortalidad a 28 días de los pacientes con gripe en la unidad de urgencias (ED), investigamos la puntuación de mortalidad por sepsis en la unidad de urgencias (MEDS), procalcitonina (PCT) y otros biomarcadores relevantes.
MétodosRealizamos un estudio retrospectivo, observacional y unicéntrico, cuya evaluación clínica fue la mortalidad a 28 días. Identificamos factores predictivos independientes, creamos un nuevo modelo predictivo combinado por regresión logística, y evaluamos el modelo mediante una curva ROC.
ResultadosIncluimos a un total de 364 pacientes consecutivos ingresados en la ED, de los cuales 45 fallecieron en el plazo de 28 días. Para predecir la mortalidad a 28 días, la puntuación MEDS y PCT fueron factores predictivos independientes con odds ratio ajustados de 1,318 (IC 95%: 1,206-1,439) y 1,038 (IC 95%: 1,010-1;065), y ABC de 0,817 (IC 95%: 0,756-0,878) y 0,793 (IC 95%: 0,725-0,861), respectivamente. La nueva combinación de la puntuación MEDS y PCT mejoró significativamente la eficacia para predecir la mortalidad a 28 días con ABC de 0,857 (IC 95%: 0,809-0,905), siendo superior a la puntuación SOFA con ABC de 0,837 (IC 95%: 0,779-0,894).
ConclusiónLa puntuación MEDS y PCT, especialmente cuanto se combinan, constituyen una buena predicción de la mortalidad de los pacientes ingresados en la ED con gripe.