Journal Information
Vol. 157. Issue 6.
Pages 298-299 (September 2021)
Vol. 157. Issue 6.
Pages 298-299 (September 2021)
Scientific letter
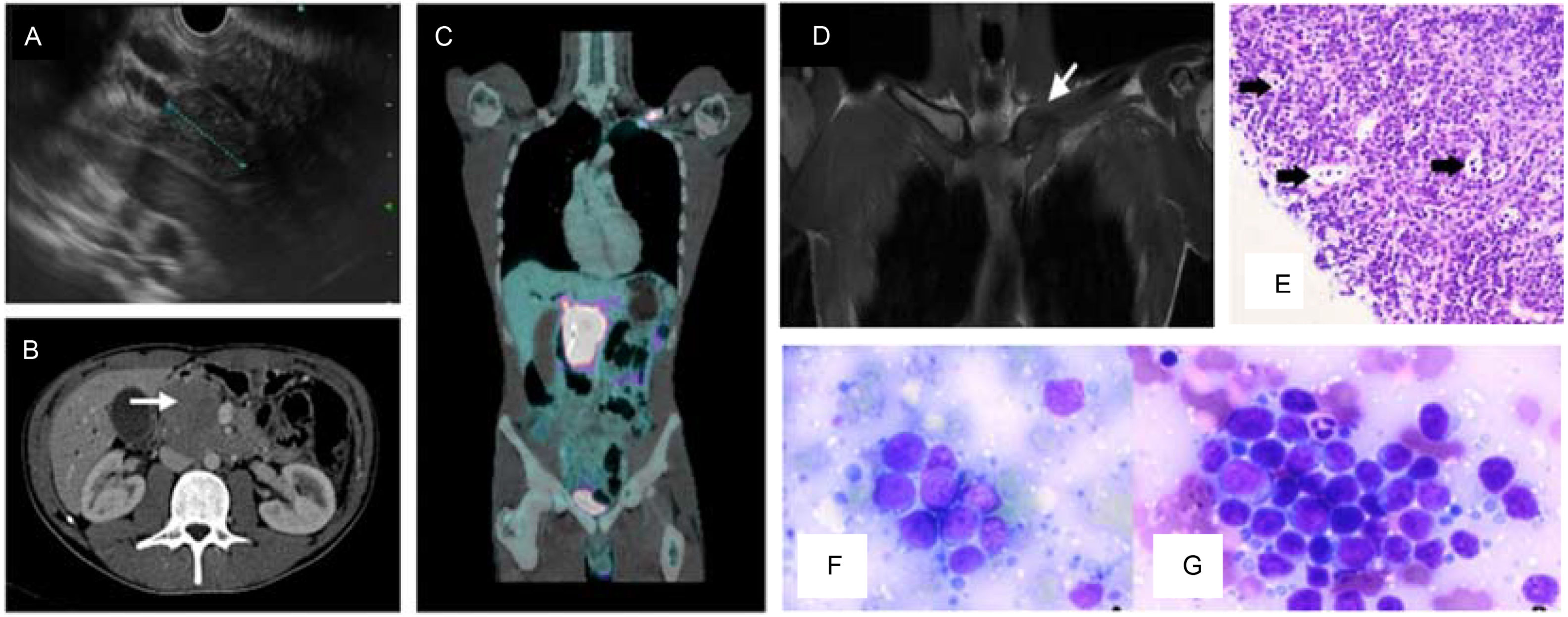
Pancreatic lymphoma: Case report
Linfoma pancreático: presentación de un caso
Visits
1
Cristina Rubín de Célix
, Celia Gómez-Labrador, Jorge Mendoza
Corresponding author
Gastroenterology Department, La Princesa University Hospital, Instituto de Investigación Sanitaria Princesa (IIS-IP), Centro de Investigación Biomédica en Red de Enfermedades Hepáticas y Digestivas (CIBEREHD), Madrid, Spain
This item has received
Article information
These are the options to access the full texts of the publication Medicina Clínica (English Edition)
Subscriber
Subscribe
Purchase
Contact
Phone for subscriptions and reporting of errors
From Monday to Friday from 9 a.m. to 6 p.m. (GMT + 1) except for the months of July and August which will be from 9 a.m. to 3 p.m.
Calls from Spain
932 415 960
Calls from outside Spain
+34 932 415 960
E-mail