Artículo
Comprando el artículo el PDF del mismo podrá ser descargado
Precio 19,34 €
Comprar ahora
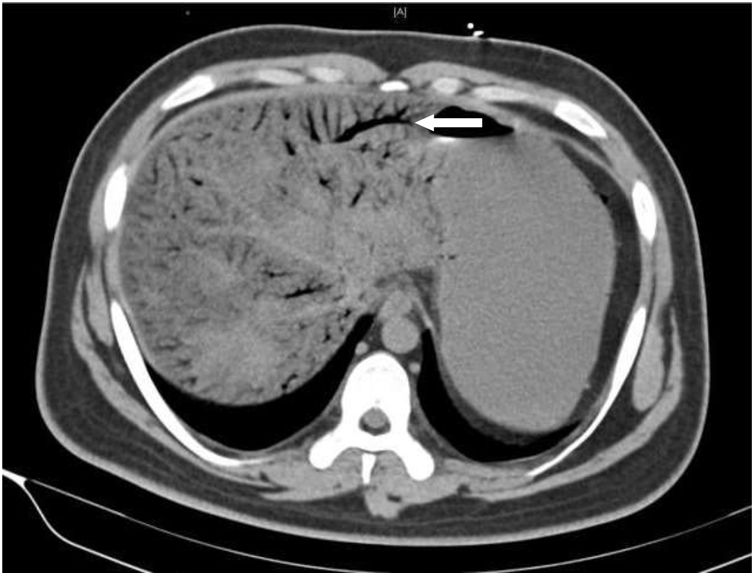
array:24 [ "pii" => "S0025775321003559" "issn" => "00257753" "doi" => "10.1016/j.medcli.2021.06.008" "estado" => "S300" "fechaPublicacion" => "2022-03-25" "aid" => "5737" "copyright" => "Elsevier España, S.L.U.. All rights reserved" "copyrightAnyo" => "2021" "documento" => "simple-article" "crossmark" => 1 "subdocumento" => "cor" "cita" => "Med Clin. 2022;158:296-7" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "Traduccion" => array:1 [ "en" => array:19 [ "pii" => "S2387020622001036" "issn" => "23870206" "doi" => "10.1016/j.medcle.2021.06.014" "estado" => "S300" "fechaPublicacion" => "2022-03-25" "aid" => "5737" "copyright" => "Elsevier España, S.L.U." "documento" => "simple-article" "crossmark" => 1 "subdocumento" => "cor" "cita" => "Med Clin. 2022;158:296-7" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "en" => array:11 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Letter to the Editor</span>" "titulo" => "Pneumatosis of portal vein: A report of 5 cases" "tienePdf" => "en" "tieneTextoCompleto" => "en" "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "296" "paginaFinal" => "297" ] ] "titulosAlternativos" => array:1 [ "es" => array:1 [ "titulo" => "Neumatosis de la vena porta: presentación de 5 casos" ] ] "contieneTextoCompleto" => array:1 [ "en" => true ] "contienePdf" => array:1 [ "en" => true ] "resumenGrafico" => array:2 [ "original" => 0 "multimedia" => array:7 [ "identificador" => "fig0005" "etiqueta" => "Fig. 1" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr1.jpeg" "Alto" => 576 "Ancho" => 755 "Tamanyo" => 54489 ] ] "descripcion" => array:1 [ "en" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">Abdominal CT imaging findings: extensive pneumatosis of intrahepatic portal vein (secondary branch), uneven intrahepatic density and ischemic change can be seen.</p>" ] ] ] "autores" => array:1 [ 0 => array:2 [ "autoresLista" => "Fangfei Wang, Shaocheng Lyu, Qiang He" "autores" => array:3 [ 0 => array:2 [ "nombre" => "Fangfei" "apellidos" => "Wang" ] 1 => array:2 [ "nombre" => "Shaocheng" "apellidos" => "Lyu" ] 2 => array:2 [ "nombre" => "Qiang" "apellidos" => "He" ] ] ] ] ] "idiomaDefecto" => "en" "Traduccion" => array:1 [ "en" => array:9 [ "pii" => "S0025775321003559" "doi" => "10.1016/j.medcli.2021.06.008" "estado" => "S300" "subdocumento" => "" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "idiomaDefecto" => "en" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S0025775321003559?idApp=UINPBA00004N" ] ] "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2387020622001036?idApp=UINPBA00004N" "url" => "/23870206/0000015800000006/v1_202204240523/S2387020622001036/v1_202204240523/en/main.assets" ] ] "itemSiguiente" => array:18 [ "pii" => "S0025775321003523" "issn" => "00257753" "doi" => "10.1016/j.medcli.2021.06.005" "estado" => "S300" "fechaPublicacion" => "2022-03-25" "aid" => "5734" "documento" => "simple-article" "crossmark" => 1 "subdocumento" => "cor" "cita" => "Med Clin. 2022;158:298" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "es" => array:10 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Carta al Editor</span>" "titulo" => "Consolidación lobar aislada como forma de presentación del linfoma MALT pulmonar" "tienePdf" => "es" "tieneTextoCompleto" => "es" "paginas" => array:1 [ 0 => array:1 [ "paginaInicial" => "298" ] ] "titulosAlternativos" => array:1 [ "en" => array:1 [ "titulo" => "Isolated lobar consolidation as a form of presentation of pulmonary MALT lymphoma" ] ] "contieneTextoCompleto" => array:1 [ "es" => true ] "contienePdf" => array:1 [ "es" => true ] "autores" => array:1 [ 0 => array:2 [ "autoresLista" => "Anna Torrente-Nieto, Marc Bonnin Vilaplana, Eric Rojas Calvera" "autores" => array:3 [ 0 => array:2 [ "nombre" => "Anna" "apellidos" => "Torrente-Nieto" ] 1 => array:2 [ "nombre" => "Marc" "apellidos" => "Bonnin Vilaplana" ] 2 => array:2 [ "nombre" => "Eric" "apellidos" => "Rojas Calvera" ] ] ] ] ] "idiomaDefecto" => "es" "Traduccion" => array:1 [ "en" => array:9 [ "pii" => "S2387020622000924" "doi" => "10.1016/j.medcle.2021.06.010" "estado" => "S300" "subdocumento" => "" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "idiomaDefecto" => "en" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2387020622000924?idApp=UINPBA00004N" ] ] "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S0025775321003523?idApp=UINPBA00004N" "url" => "/00257753/0000015800000006/v1_202203120542/S0025775321003523/v1_202203120542/es/main.assets" ] "itemAnterior" => array:19 [ "pii" => "S0025775321003584" "issn" => "00257753" "doi" => "10.1016/j.medcli.2021.06.010" "estado" => "S300" "fechaPublicacion" => "2022-03-25" "aid" => "5740" "copyright" => "Elsevier España, S.L.U." "documento" => "simple-article" "crossmark" => 1 "subdocumento" => "cor" "cita" => "Med Clin. 2022;158:295-6" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "es" => array:10 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Carta al Editor</span>" "titulo" => "Síndrome de Alagille y carcinoma hepatocelular en adulto no cirrótico" "tienePdf" => "es" "tieneTextoCompleto" => "es" "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "295" "paginaFinal" => "296" ] ] "titulosAlternativos" => array:1 [ "en" => array:1 [ "titulo" => "Alagille syndrome and hepatocellular carcinoma in a non-cirrhotic adult" ] ] "contieneTextoCompleto" => array:1 [ "es" => true ] "contienePdf" => array:1 [ "es" => true ] "autores" => array:1 [ 0 => array:2 [ "autoresLista" => "Juan Antonio Vázquez Rodríguez, Carmen Molina Villalba, Matías Estévez Escobar" "autores" => array:3 [ 0 => array:2 [ "nombre" => "Juan Antonio" "apellidos" => "Vázquez Rodríguez" ] 1 => array:2 [ "nombre" => "Carmen" "apellidos" => "Molina Villalba" ] 2 => array:2 [ "nombre" => "Matías" "apellidos" => "Estévez Escobar" ] ] ] ] ] "idiomaDefecto" => "es" "Traduccion" => array:1 [ "en" => array:9 [ "pii" => "S2387020622000948" "doi" => "10.1016/j.medcle.2021.06.012" "estado" => "S300" "subdocumento" => "" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "idiomaDefecto" => "en" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2387020622000948?idApp=UINPBA00004N" ] ] "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S0025775321003584?idApp=UINPBA00004N" "url" => "/00257753/0000015800000006/v1_202203120542/S0025775321003584/v1_202203120542/es/main.assets" ] "en" => array:16 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Letter to the Editor</span>" "titulo" => "Pneumatosis of portal vein: A report of 5 cases" "tieneTextoCompleto" => true "saludo" => "Dear Editor," "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "296" "paginaFinal" => "297" ] ] "autores" => array:1 [ 0 => array:4 [ "autoresLista" => "Fangfei Wang, Shaocheng Lyu, Qiang He" "autores" => array:3 [ 0 => array:2 [ "nombre" => "Fangfei" "apellidos" => "Wang" ] 1 => array:2 [ "nombre" => "Shaocheng" "apellidos" => "Lyu" ] 2 => array:4 [ "nombre" => "Qiang" "apellidos" => "He" "email" => array:1 [ 0 => "heqiang349@163.com" ] "referencia" => array:1 [ 0 => array:2 [ "etiqueta" => "<span class="elsevierStyleSup">*</span>" "identificador" => "cor0005" ] ] ] ] "afiliaciones" => array:1 [ 0 => array:2 [ "entidad" => "Department of Hepatobiliary Surgery, Beijing Chaoyang Hospital, Capital Medical University, No.8, Gongtinan Road, Chaoyang District, 100020 Beijing, China" "identificador" => "aff0005" ] ] "correspondencia" => array:1 [ 0 => array:3 [ "identificador" => "cor0005" "etiqueta" => "⁎" "correspondencia" => "Corresponding author." ] ] ] ] "titulosAlternativos" => array:1 [ "es" => array:1 [ "titulo" => "Neumatosis de la vena porta: presentación de 5 casos" ] ] "resumenGrafico" => array:2 [ "original" => 0 "multimedia" => array:7 [ "identificador" => "fig0005" "etiqueta" => "Fig. 1" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr1.jpeg" "Alto" => 576 "Ancho" => 755 "Tamanyo" => 54489 ] ] "descripcion" => array:1 [ "en" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">Abdominal CT imaging findings: extensive pneumatosis of intrahepatic portal vein (secondary branch), uneven intrahepatic density and ischemic change can be seen.</p>" ] ] ] "textoCompleto" => "<span class="elsevierStyleSections"><p id="par0005" class="elsevierStylePara elsevierViewall">Portal venous gas (PVG) refers to the abnormal accumulation of gas in portal vein and intrahepatic portal vein branches due to various reasons. At present, CT is an important auxiliary examination for definite diagnosis. Now we report the general information and diagnosis and treatment of 5 patients with pneumatosis of portal vein in our hospital. Among them, 3 cases were seriously ill and could not tolerate operation. Finally, 5 patients received conservative treatment, 3 patients were cured and 2 patient died. The characteristics of the 5 patients were analyzed and the related literature was reviewed. The results showed that the patients with mild portal vein pneumatosis could be treated conservatively and the changes of the disease should be closely observed. If the condition could not be controlled or suspected of intestinal necrosis, intestinal perforation or severe infection, emergency surgery should be actively carried out (<a class="elsevierStyleCrossRef" href="#fig0005">Fig. 1</a>).</p><elsevierMultimedia ident="fig0005"></elsevierMultimedia><p id="par0010" class="elsevierStylePara elsevierViewall">The 5 patients above were 4 males and 1 female, aged 22–83 years, with acute abdomen caused by intestinal obstruction and cavity pressure rise. In addition, 3 patients also had severe abdominal infection symptoms (fever, elevated white blood cells, and signs of peritonitis). The other 2 patients only showed abdominal distension with slight abdominal pain after stopping exhaust and defecation, without fever and peritonitis. 5 patients with PVG were diagnosed by plain abdominal CT scan. In 3 patients with severe infection, the gas in portal vein extended to the secondary branch of portal vein. And in 2 patients with mild symptoms, the gas in portal vein only appeared in the third branch of portal vein.</p><p id="par0015" class="elsevierStylePara elsevierViewall">There are 2 treatment methods for PVG: surgical treatment and conservative treatment. The choice of different treatment methods mainly depends on the primary disease and the severity of the disease.<a class="elsevierStyleCrossRef" href="#bib0030"><span class="elsevierStyleSup">1</span></a> In the past, PVG was generally considered to be associated with intestinal necrosis, so it was considered as the surgical indication for abdominal exploration in acute abdomen. In 1978, Liebman<a class="elsevierStyleCrossRef" href="#bib0035"><span class="elsevierStyleSup">2</span></a> and others first reviewed and analyzed the literature about PVG. The incidence of intestinal necrosis in 64 patients with PVG was 72%, and the overall mortality rate was 75%. However, with the deepening of the understanding of PVG, it is considered that conservative treatment should be tried for patients with mild symptoms, stable vital signs or poor general conditions that are not suitable for surgery. The conservative treatment programs mainly include the fasting water, gastrointestinal decompression, intravenous nutrition support treatment, anti-inflammatory treatment, etc. In the conservative process, it was possible to closely observe the changes of the condition, and adopted surgical treatment when the condition could not be controlled.<a class="elsevierStyleCrossRef" href="#bib0040"><span class="elsevierStyleSup">3</span></a> However, patients who are highly suspected to have intestinal necrosis, intestinal perforation or severe infection at the beginning should be actively treated with emergency surgery.<a class="elsevierStyleCrossRef" href="#bib0045"><span class="elsevierStyleSup">4</span></a> Among the 5 patients, 2 elderly patients gave up surgical exploration due to the history of coronary heart disease and unstable angina pectoris. The young patient with severe infection was given conservative treatment first, however the disease progressed rapidly and deteriorated quickly. The 2 patients with mild symptoms were treated with conservative treatment including anti-inflammatory, gastrointestinal decompression and nutritional support. Finally, the young one elderly patient died during the observation period, and the remaining three patients were cured.</p><p id="par0020" class="elsevierStylePara elsevierViewall">It can be seen that PVG is not the indication of surgical exploration for acute abdomen.<a class="elsevierStyleCrossRef" href="#bib0050"><span class="elsevierStyleSup">5</span></a> Once found, it is necessary to carefully evaluate whether there is intestinal ischemia and necrosis in patients. Dynamic assessment should be made according to the etiology, vital signs and changes of auxiliary examination, so as to avoid improper selection of treatment plan and delay of treatment opportunity. For patients with mild symptoms, stable vital signs or poor general conditions, conservative treatment such as fasting water, gastrointestinal decompression, intravenous nutrition support, anti-inflammatory treatment can be tried first; for patients with intestinal necrosis, active surgical treatment should be taken.</p><span id="sec0005" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0005">Contributors</span><p id="par0025" class="elsevierStylePara elsevierViewall">HQ proposed the study. WFF and LSC performed the research and wrote the first draft. LSC and WFF had equal contribution to the study. All authors contributed to the design and interpretation of the study and to further drafts. HQ is the guarantor.</p></span><span id="sec0010" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0010">Ethical approval</span><p id="par0030" class="elsevierStylePara elsevierViewall">Yes.</p></span><span id="sec0015" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0015">Funding</span><p id="par0035" class="elsevierStylePara elsevierViewall">No.</p></span><span id="sec0020" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0020">Conflict of interest</span><p id="par0040" class="elsevierStylePara elsevierViewall">No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.</p></span></span>" "textoCompletoSecciones" => array:1 [ "secciones" => array:6 [ 0 => array:2 [ "identificador" => "sec0005" "titulo" => "Contributors" ] 1 => array:2 [ "identificador" => "sec0010" "titulo" => "Ethical approval" ] 2 => array:2 [ "identificador" => "sec0015" "titulo" => "Funding" ] 3 => array:2 [ "identificador" => "sec0020" "titulo" => "Conflict of interest" ] 4 => array:2 [ "identificador" => "xack591503" "titulo" => "Acknowledgements" ] 5 => array:1 [ "titulo" => "References" ] ] ] "pdfFichero" => "main.pdf" "tienePdf" => true "multimedia" => array:1 [ 0 => array:7 [ "identificador" => "fig0005" "etiqueta" => "Fig. 1" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr1.jpeg" "Alto" => 576 "Ancho" => 755 "Tamanyo" => 54489 ] ] "descripcion" => array:1 [ "en" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">Abdominal CT imaging findings: extensive pneumatosis of intrahepatic portal vein (secondary branch), uneven intrahepatic density and ischemic change can be seen.</p>" ] ] ] "bibliografia" => array:2 [ "titulo" => "References" "seccion" => array:1 [ 0 => array:2 [ "identificador" => "bibs0015" "bibliografiaReferencia" => array:5 [ 0 => array:3 [ "identificador" => "bib0030" "etiqueta" => "1" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "In-hospital mortality for hepatic portal venous gas: analysis of 1590 patients using a Japanese national inpatient database" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:5 [ 0 => "C. Koizumi" 1 => "N. Michihata" 2 => "H. Matsui" 3 => "K. Fushimi" 4 => "H. Yasunaga" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1007/s00268-017-4189-y" "Revista" => array:6 [ "tituloSerie" => "World J Surg" "fecha" => "2018" "volumen" => "42" "paginaInicial" => "816" "paginaFinal" => "822" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/28879575" "web" => "Medline" ] ] ] ] ] ] ] ] 1 => array:3 [ "identificador" => "bib0035" "etiqueta" => "2" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Hepatic-portal venous gas in adults: etiology, pathophysiology and clinical significance" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:5 [ 0 => "P.R. Liebman" 1 => "M.T. Patten" 2 => "J. Manny" 3 => "J.R. Benfield" 4 => "H.B. Hechtman" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1097/00000658-197803000-00012" "Revista" => array:6 [ "tituloSerie" => "Ann Surg" "fecha" => "1978" "volumen" => "187" "paginaInicial" => "281" "paginaFinal" => "287" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/637584" "web" => "Medline" ] ] ] ] ] ] ] ] 2 => array:3 [ "identificador" => "bib0040" "etiqueta" => "3" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Bowel ischemia and portal venous gas: what to do?" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:2 [ 0 => "P. Sridhar" 1 => "P.M. Fisichella" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1089/lap.2016.0171" "Revista" => array:5 [ "tituloSerie" => "J Laparoendosc Adv Surg Tech A" "fecha" => "2016" "volumen" => "26" "paginaInicial" => "713" "paginaFinal" => "714" ] ] ] ] ] ] 3 => array:3 [ "identificador" => "bib0045" "etiqueta" => "4" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Hepatic portal venous gas: an III omen or a misleading sign" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:5 [ 0 => "S. Mehta" 1 => "G.S. Desai" 2 => "S. Shah" 3 => "H. Mehta" 4 => "A. Phadke" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1055/s-0040-1702919" "Revista" => array:5 [ "tituloSerie" => "Surg J (N Y)" "fecha" => "2020" "volumen" => "6" "paginaInicial" => "37" "paginaFinal" => "41" ] ] ] ] ] ] 4 => array:3 [ "identificador" => "bib0050" "etiqueta" => "5" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Optimal treatment strategies for hepatic portal venous gas: a retrospective assessment" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:5 [ 0 => "M. Gonda" 1 => "T. Osuga" 2 => "Y. Ikura" 3 => "H. Mehta" 4 => "A. Phadke" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.3748/wjg.v26.i14.1628" "Revista" => array:6 [ "tituloSerie" => "World J Gastroenterol" "fecha" => "2020" "volumen" => "26" "paginaInicial" => "1628" "paginaFinal" => "1637" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/32327911" "web" => "Medline" ] ] ] ] ] ] ] ] ] ] ] ] "agradecimientos" => array:1 [ 0 => array:4 [ "identificador" => "xack591503" "titulo" => "Acknowledgements" "texto" => "<p id="par0045" class="elsevierStylePara elsevierViewall">We will thank the patients for their great help in this report. This paper is supported by Dr. HQ.</p>" "vista" => "all" ] ] ] "idiomaDefecto" => "en" "url" => "/00257753/0000015800000006/v1_202203120542/S0025775321003559/v1_202203120542/en/main.assets" "Apartado" => array:4 [ "identificador" => "66430" "tipo" => "SECCION" "es" => array:2 [ "titulo" => "Cartas al Editor" "idiomaDefecto" => true ] "idiomaDefecto" => "es" ] "PDF" => "https://static.elsevier.es/multimedia/00257753/0000015800000006/v1_202203120542/S0025775321003559/v1_202203120542/en/main.pdf?idApp=UINPBA00004N&text.app=https://www.elsevier.es/" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S0025775321003559?idApp=UINPBA00004N" ]
Consulte los artículos y contenidos publicados en este medio, además de los e-sumarios de las revistas científicas en el mismo momento de publicación
Esté informado en todo momento gracias a las alertas y novedades
Acceda a promociones exclusivas en suscripciones, lanzamientos y cursos acreditados
Medicina Clínica, fundada en 1943, es la única publicación semanal de contenido clínico que se edita en España y constituye el máximo exponente de la calidad y pujanza de la medicina española. Son características fundamentales de esta publicación el rigor científico y metodológico de sus artículos, la actualidad de los temas y, sobre todo, su sentido práctico, buscando siempre que la información sea de la mayor utilidad en la práctica clínica. Los contenidos de Medicina Clínica abarcan dos frentes: trabajos de investigación original rigurosamente seleccionados atendiendo a su calidad, originalidad e interés, y trabajos orientados a la formación continuada, encomendados por la revista a autores relevantes (Editoriales, Revisiones, Conferencias clínicas y clínico-patológicas, Diagnóstico y Tratamiento). En estos artículos se ponen al día aspectos de destacado interés clínico o conceptual en la medicina actual. Medicina Clínica es un vehículo de información científica de reconocida calidad, como demuestra su inclusión en los más prestigiosos y selectivos índices bibliográficos del mundo.
Current Contents/Clinical Medicine, Journal Citation Reports, SCI-Expanded, Index Medicus/Medline, Excerpta Medica/EMBASE, IBECS, IME, MEDES, PASCAL, SCOPUS, ScienceDirect
Ver másEl factor de impacto mide la media del número de citaciones recibidas en un año por trabajos publicados en la publicación durante los dos años anteriores.
© Clarivate Analytics, Journal Citation Reports 2022
SJR es una prestigiosa métrica basada en la idea de que todas las citaciones no son iguales. SJR usa un algoritmo similar al page rank de Google; es una medida cuantitativa y cualitativa al impacto de una publicación.
Ver másSNIP permite comparar el impacto de revistas de diferentes campos temáticos, corrigiendo las diferencias en la probabilidad de ser citado que existe entre revistas de distintas materias.
Ver más¿Es usted profesional sanitario apto para prescribir o dispensar medicamentos?
Are you a health professional able to prescribe or dispense drugs?
Você é um profissional de saúde habilitado a prescrever ou dispensar medicamentos