To assess the prevalence and impact of cerebrovascular risk factors (CRF) on cerebrovascular events (CVE) in patients with giant cell arteritis (GCA).
MethodsAnalysis of the patients diagnosed with GCA identified in the Spanish Hospital Discharge Database between 2016 and 2018.
Results8,474 hospital admissions from patients diagnosed with GCA were identified. 3.4% of the admissions were motivated by CVE (stroke in 2.8% and transient ischemic attack in 0.6%). When compared with the admissions due to other causes, the patients who suffered from CVE presented a higher rate of male sex (36.2% vs 43.5%, p=0.007), hypertension (66.9% vs 74.4%, p=0.004), diabetes (27.6% vs 33.7%, p=0.016) and atherosclerosis (6.6% vs 10.2%, p=0.0.017). After adjustment, male sex (OR=1.35, 95% CI 1.06–1.72) and mainly hypertension (OR=1.44, 95% CI 1.11–1.90) were associated with a higher risk of CVE.
ConclusionHypertension, along with male sex, was the strongest risk factor for cerebrovascular events in GCA patients. In these high-risk patients, antiplatelet therapy should be re-considered and evaluated in prospective studies.
Evaluar la prevalencia e impacto de los factores de riesgo cerebrovasculares en los episodios cerebrovasculares (ECV) de pacientes con arteritis de células gigantes (ACG).
MétodosAnálisis de los pacientes diagnosticados con ACG identificados en la base de altas hospitalarias española entre 2016 y 2018.
ResultadosSe identificaron 8.474 ingresos hospitalarios en pacientes diagnosticados de ACG. El 3,4% de los ingresos se atribuyó a ECV (ictus en 2,8% y accidente isquémico transitorio en 0,6%). En comparación con los ingresos por otras causas, los pacientes que presentaron ECV mostraron una mayor tasa de sexo masculino (36,2 frente a 43,5%, p=0,007), hipertensión (66,9 frente a 74,4%, p=0,004), diabetes (27,6 frente a 33,7%, p=0,016) y aterosclerosis (6,6 frente a 10,2%, p=0,0017). Tras el ajuste, el sexo masculino (OR=1,35, IC 95% 1,06-1,72) y principalmente la hipertensión (OR=1,44, IC 95% 1,11-1,90) se asociaron con un mayor riesgo de ECV.
ConclusiónLa hipertensión, junto con el sexo masculino, fueron los principales factores de riesgo de ECV en los pacientes con ACG. En estos pacientes de alto riesgo, el tratamiento con antiagregantes debería reconsiderarse y evaluarse en estudios prospectivos.
Giant cell arteritis (GCA) is a chronic granulomatous vasculitis affecting the aorta and its main ramifications, with special predilection for the extracranial branches of the carotid artery.1,2 In the setting of arterial inflammation and vascular deficit, severe arterial compromise can even lead to ischemic phenomena, one of the most severe complications of the disease, with a high morbidity and mortality impact.1,2 Herein, several studies have reported a higher risk of cerebrovascular events in the presence of classical cardiovascular risk factors.3,4 In light of the previous, prophylactic antiplatelet therapy was initially encouraged in the original EULAR recommendations. However, since other reports did not confirm a solid effect of aspirin in GCA, aspirin use was no longer routinely recommended in the latest recommendations.5
Therefore, the aim of our study was to analyze the prevalence and impact of cerebrovascular risk factors (CRF) in patients with GCA, to identify those who are at higher risk and could potentially benefit from antiplatelet therapy.
Materials and methodsPatientsWe performed an observational and retrospective analysis with data from The Spanish Hospital Discharge Database (SNHDD), a registry that belongs to the Spanish Ministry of Health. SNHDD includes demographic and epidemiological data and up to 20 discharge diagnoses carried out during admission defined by the International Classification of Diseases (ICD-10) from 1 January 2016. We selected hospital admissions from 1 January 2016 to 31 December 2018 for patients with a diagnosis within the ICD-10 code M31.5 (giant cell arteritis with polymyalgia rheumatica) and M31.6 (other giant cell arteritis), at any position in the diagnostic list. The study complies with the Declaration of Helsinki and was approved by the local research ethics committee.
Assessment of cerebrovascular events and identification of cardiovascular risk factorsOnce patients with CGA diagnosis were selected, those whose admission was attributable to cerebrovascular events (CVE) were identified. CVE were considered if the main diagnosis was acute ischemic stroke (code I63) or transient ischemic attack (TIA, code G45). Patients were identified as hypertense if they presented primary hypertension (code I10), hypertensive cardiac disease (I11), hypertensive chronic kidney disease (I12), hypertensive cardiac and chronic kidney disease (I13) or secondary hypertension (I15). Diabetes was identified by type 1 diabetes mellitus (E10), type 2 diabetes mellitus (E11) and other types of diabetes mellitus (E12). Dyslipidemia was defined by hypercholesterolemia (E78) and hyperlipidemia (E78.2 and E78.5). Tobacco was classified according to tobacco consumption (Z72.0) or nicotine dependence (F17).
Statistical analysisCategorical variables were reported as frequencies and percentages and continuous variables were presented as mean and standard deviation. The significance of baseline differences between admissions attributable to CVE and those who did not was determined by the chi-square, Fisher's or Student's t test as appropriate. A multivariate logistic regression analysis was performed to determine the factors related to CVE in patients with GCA. For all the analyses, a significance level of 0.05 was set. Statistical analysis was performed using SPSS version 26.0 (IBM, Spain).
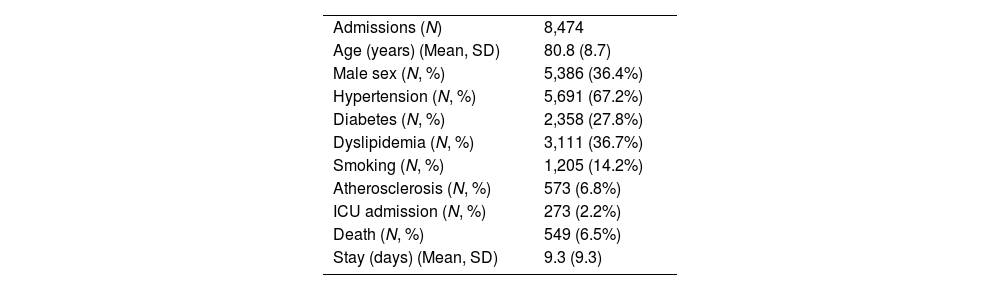
ResultsPatient's characteristics8,474 admissions in GCA diagnosed patients were identified between 2016 and 2018. The characteristics of the admissions and the population are shown in Table 1. Overall, the mean age was 80.8 years-old and 36.4% were male. Regarding CRF, 67.2% were hypertense, 27.8% suffered from diabetes, 36.7% from dyslipidemia and in 14.2% the smoking habit was identified. 6.8% presented prior atherosclerosis diagnosis. Overall mortality rate was 6.5% and the mean average stay was 9.3 days.
Admitted patients in Spain with GCA.
| Admissions (N) | 8,474 |
| Age (years) (Mean, SD) | 80.8 (8.7) |
| Male sex (N, %) | 5,386 (36.4%) |
| Hypertension (N, %) | 5,691 (67.2%) |
| Diabetes (N, %) | 2,358 (27.8%) |
| Dyslipidemia (N, %) | 3,111 (36.7%) |
| Smoking (N, %) | 1,205 (14.2%) |
| Atherosclerosis (N, %) | 573 (6.8%) |
| ICU admission (N, %) | 273 (2.2%) |
| Death (N, %) | 549 (6.5%) |
| Stay (days) (Mean, SD) | 9.3 (9.3) |
GCA: giant cell arteritis, SD: standard deviation, ICU: intensive care unit.
Quantitative data are expressed in mean and standard deviation (SD), qualitative data as number and percentage (%).
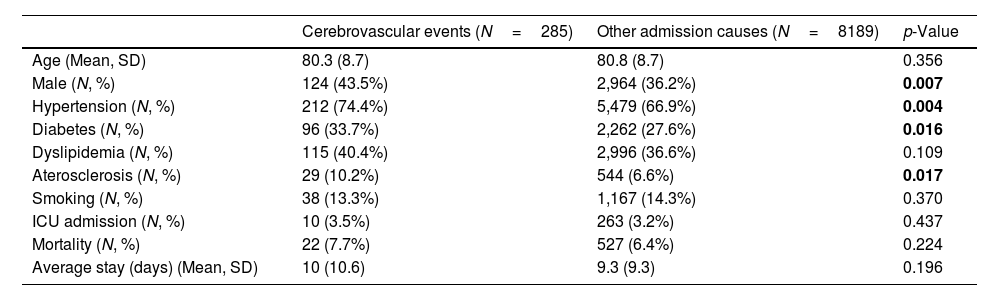
Overall, 3.4% of the admissions were attributable to a cerebrovascular event (ischemic stroke in 2.8% and TIA in 0.6%). When compared to the admissions due to other causes (Table 2), the patients who suffered from CVE presented a higher rate of male sex (36.2% vs 43.5%, p=0.007), a higher burden of cardiovascular risk factors as hypertension (66.9% vs 74.4%, p=0.004) or diabetes (27.6% vs 33.7%, p=0.016) and more atherosclerosis (6.6% vs 10.2%, p=0.0.02). No differences were found regarding age, ICU admission, mortality or average stays.
Differences among admissions related to a cerebrovascular event.
| Cerebrovascular events (N=285) | Other admission causes (N=8189) | p-Value | |
|---|---|---|---|
| Age (Mean, SD) | 80.3 (8.7) | 80.8 (8.7) | 0.356 |
| Male (N, %) | 124 (43.5%) | 2,964 (36.2%) | 0.007 |
| Hypertension (N, %) | 212 (74.4%) | 5,479 (66.9%) | 0.004 |
| Diabetes (N, %) | 96 (33.7%) | 2,262 (27.6%) | 0.016 |
| Dyslipidemia (N, %) | 115 (40.4%) | 2,996 (36.6%) | 0.109 |
| Aterosclerosis (N, %) | 29 (10.2%) | 544 (6.6%) | 0.017 |
| Smoking (N, %) | 38 (13.3%) | 1,167 (14.3%) | 0.370 |
| ICU admission (N, %) | 10 (3.5%) | 263 (3.2%) | 0.437 |
| Mortality (N, %) | 22 (7.7%) | 527 (6.4%) | 0.224 |
| Average stay (days) (Mean, SD) | 10 (10.6) | 9.3 (9.3) | 0.196 |
SD: standard deviation, ICU: intensive care unit.
Quantitative data are expressed in mean and standard deviation (SD), qualitative data as number and percentage (%).
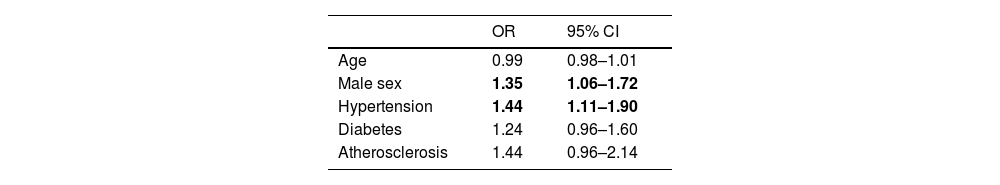
Finally, a multivariate analysis was performed to identify the factors related to cerebrovascular events (Table 3). After adjustment, male sex (OR=1.35, 95% CI 1.06–1.72) and hypertension (OR=1.44, 95% CI 1.11–1.90) were associated with a higher risk while diabetes (OR=1.24, 95% CI 0.96–1.60) and atherosclerosis (OR=1.44, 95% CI 0.96–2.14) did not.
DiscussionThis nation-wide analysis is one of the largest studies exploring factors related to cerebrovascular events in GCA, confirming that male sex and hypertension determine a higher risk of stroke in patients with this disease.
In our registry, 3.4% of GCA patients were admitted because of either stroke or TIA. While ischemic complications have been described in up to 50% of the patients, severe events such as TIA and stablished stroke have been identified in a similar proportion as in ours.1,2 Therefore, these data highlight the remarkable CVE risk and in the setting of GCA. Despite the relative low prevalence, their impact is obviously significant.
In GCA, ischemic events occur in relation to intimal hyperplasia that eventually occludes the lumen of the vessel.1,2 However, it has been pointed out that cardiovascular risk factors may increase the risk of ischemic events in these patients, since they are likely to be involved in the development of thrombotic phenomena on the damaged vessel, as occurs in atheromatous arterial disease.6,7 In our study, patients with CVE presented a higher rate of male sex, hypertension, diabetes and more atherosclerosis, confirming that CRF contribute to the inflammatory injury of the vessel. However, in the multivariate analysis, only male sex and hypertension were related to CVE. Similar findings have been described by others, confirming that hypertension is the main factor related to cerebral ischemic events in the setting of GCA, over diabetes, dyslipidemia or tobacco.2 Besides, hypertension is also the stronger risk factor of stroke in general population and male sex presents inherent higher risk of stroke.8
In the light of the aforementioned, diagnosis and treatment of atherosclerotic disease might play a major role during GCA management. In addition to prompt identification and treatment of the cardiovascular risk factors, questions about prophylactic use of antiaggregant therapy arise. Prior retrospective cohorts have shown that aspirin-treated groups developed less cerebrovascular complications,6,7 while more recent studies, including one metanalysis, have not confirmed that antiplatelet or anticoagulant therapy could reduce severe ischemic events in GCA.4,9,10 After these, the latest EULAR recommendations did not encouraged again prophylactic antiplatelet treatment as in the original guideline.5 However, the not despicable prevalence of serious CVE and the prevalence and impact of the cerebrovascular risk factors in our cohort suggest that probably antiaggregant use in GCA should be more carefully analyzed. To this purpose, other studies should also consider the cardiovascular risk factors, atherosclerosis prevalence as well as the bleeding risk, in order to individualize the best approach.
Our study presents several limitations. Due to the database configuration, essential information such as antiplatelet, anticoagulant, tocilizumab or steroid treatment prior to the admission, and more complete data about the course and diagnosis of the disease, including the number of confirmatory biopsies, the extent of disease, the number or type of vessels involved, and length of disease, among others, was lacking. This information could have yielded a more complete understanding of the factors related to cerebrovascular events. Despite these pitfalls, we believe that our results are valid and robust although prospective and multicentric studies are needed to confirm our findings.
ConclusionsOur study reveals that hypertension, along with male sex, was the strongest risk factor of cerebrovascular events in GCA patients. In these high-risk patients, the debate about antiplatelet therapy should be re-considered and evaluated in prospective studies.
Ethical considerationsThe study was developed in accordance with the Code of Ethics of the World Medical Association (Declaration of Helsinki) and was approved by the Research Ethics Committee of the center (PI 67-23).
FinancingThis work has been financed with the help of the Carlos III Health Institute (Río-Hortega contract of the first author, file CM19/00223) and with the help of the Academia Médico-Quirúrgica Española.
Conflicts of interestThe authors declare they have no conflicts of interest.