Several authors have reported the association between COVID-19, acral dermo-vascular findings, pulmonary embolism (PE) and disseminated intravascular coagulation (DIC).1–5 Herein we report a case of a COVID-19 pneumonia in a lung cancer patient with solitary brain metastases, whose initial clinical findings were secondary acrocyanosis and PE.
A 59-year-old man diagnosed with bone metastasis and solitary brain metastasis secondary to lung adenocarcinoma in treatment with osimertinib came into Radiation Oncology Department to receive brain stereotactic radiation therapy. Several comorbidities were identified: atrial fibrillation anticoagulated with LMWH, arterial hypertension and hypercholesterolemia treated with medications. Previous neurologic symptoms were fully abolished with dexamethasone 12mg/d and lumbar pain related with bone metastases was controlled with transdermic fentanyl. No respiratory distress was present upon the first visit.
On the first treatment day (day 0) the patient presented to the hospital with cushingoid face, cough, fatigue, shortness of breath beginning suddenly two days before, lower extremities edemas, and painful, discolored skin area surrounding small shallow ulcer on the right big toe. Vital signs on day 0 were T 37.0°C, HR 110bpm, BP 89/56mm Hg, and SpO2 88% on room air. Most prominent physical exam findings were dispersed crackles on lungs auscultation, leg edemas up to the knees, and a painful 5mm in diameter clean shallow ulcer with sharp margins located in the plantar surface of the right big toe, surrounded by patches of violaceous skin extended to the second toe. The violaceus patches faded under pressure. The baseline EKG showed rapid atrial fibrillation.
Cardiac failure secondary to PE was suspected and treatment with digoxin was started. On CT pulmonary angiogram (CTPA) it was documented the presence of filling defects in several lobar arteries diagnostic for PE associated with extensive opacifications involving both lungs interpreted as lung infarctions. Furthermore, tumor progression in the primary site and mediastinum was observed. Based on these findings, the patient was hospitalized, the LMWH dose was increased, oxygen was supplied through nasal cannula, and diuretics plus antibiotics (tazobactam and clindamycin) were started.
Vascular surgeons examined the patient on day 8, verifying popliteal and foot pulse and not recommending vascular radiological exams due to the apparent distal nature of the vascular compromise. On day 9, the violaceus discoloration was more extensive, involving the right aspect of the foot. More severe dyspnea than before prompted to a thorax X-ray showing an extensive and diffuse bilateral lung infiltrate raising the suspicion of COVID-19 pneumonia. The patient was tested with positive result on PCR for SARS-CoV-2.
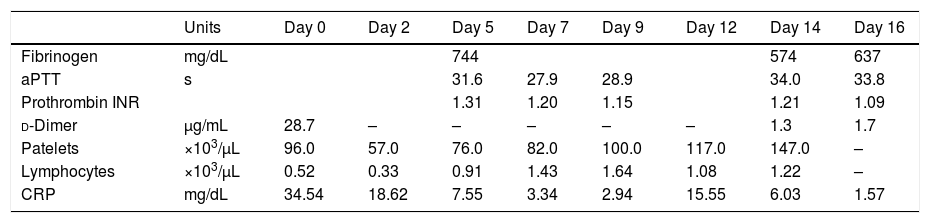
Table 1 shows the most relevant analytical parameters in chronological order. The clotting profile was not impaired (aPTT normal and Prothrombin INR slightly increased above 1.2), but d-dimer levels were elevated above 0.6mg/mL (normal level, <0.6mg/mL) and low platelet count reached grade 2 thrombocytopenia. No DIC criteria were fulfilled.
Analytical parameters in chronological order.
| Units | Day 0 | Day 2 | Day 5 | Day 7 | Day 9 | Day 12 | Day 14 | Day 16 | |
|---|---|---|---|---|---|---|---|---|---|
| Fibrinogen | mg/dL | 744 | 574 | 637 | |||||
| aPTT | s | 31.6 | 27.9 | 28.9 | 34.0 | 33.8 | |||
| Prothrombin INR | 1.31 | 1.20 | 1.15 | 1.21 | 1.09 | ||||
| d-Dimer | μg/mL | 28.7 | – | – | – | – | – | 1.3 | 1.7 |
| Patelets | ×103/μL | 96.0 | 57.0 | 76.0 | 82.0 | 100.0 | 117.0 | 147.0 | – |
| Lymphocytes | ×103/μL | 0.52 | 0.33 | 0.91 | 1.43 | 1.64 | 1.08 | 1.22 | – |
| CRP | mg/dL | 34.54 | 18.62 | 7.55 | 3.34 | 2.94 | 15.55 | 6.03 | 1.57 |
After 22 days of hospitalization the patient died due to COVID-19 infection, Staph. Aureus bacteremia, bilateral pulmonary embolism, and progressive metastatic lung cancer.
Compared with COVID-19 patients without cancer, COVID-19 patients with cancer had higher risks in death, admission into an intensive care unit, development of severe/critical symptoms, and utilization of invasive mechanical ventilation.3 Patients with blood cancers, lung cancers, or with metastatic cancer (stage IV) had the highest frequency of severe events.1
Cases of COVID-19 bilateral pneumonia and concomitant acute PE have been reported.2,3 The incidence of venous thrombo-embolism (VTE) in 81 patients with severe COVID-19 pneumonia is 25%.4 The VTE group had older age, lower lymphocytes count, longer APTT, and higher d-dimer.4 Among 184 COVID-19 patients in a Dutch ICU, 31% had thrombotic complications, PE being the most frequent thrombotic complication (n=25, 81%).3
Central thromboembolic events are not the only vascular complications of COVID-19. Zhang et al. have reported 7 patients with critical COVID-19 pneumonia and acro-ischemia.5 All patients had finger/toe cyanosis, skin bulla and dry gangrene. d-Dimer, fibrinogen and fibrinogen degradation product (FDP) were significantly elevated in most patients.
In summary, we now report one COVID-19 case with lung cancer and atrial fibrillation presenting central and peripheral intravascular complications highlighting the importance of hypercoagulation status in the pathogenesis, clinical presentation and prognosis of the disease.