COVID-19 pneumonia is the most frequent clinical manifestation of this disease, and its long-term sequelae and possible progression to pulmonary fibrosis are still unknown. The aim of this study is a mid-term review of the sequelae on plain chest radiography (CXR) in patients with a previous diagnosis of COVID-19 pneumonia.
Patients and methodsRetrospective review of patients with a diagnosis of COVID-19 pneumonia, assessing the persistence of residual lesions in the control CXR and analysing their possible relationship with epidemiological factors, risk factors, treatments received and initial radiological patterns.
ResultsA total of 143 patients (52 women and 91 men) were analysed. Mean age was 64 years. Radiological complete resolution (CR) was observed in 104 (73%) and partial resolution (PR) in 39 (27%). Of the risk factors only age was significantly related to persistence of residual lesions (OR 1.06 CI95% (1.02,1.10). In relation to treatments, significant differences were found with tocilizumab and glucocorticoids, where treated patients had a higher risk of residual lesions (OR 2.44 (1.03,5.80) and 3.05(1.43,6.51) respectively. In the analysis of radiological patterns, significant differences were observed in patients with peripheral condensations in the acute course and a pattern of early radiological worsening. A clinical-radiological dissociation was evident: 83% of patients with residual lesions had no respiratory symptoms.
DiscussionCOVID19 pneumonias may have a slower radiological resolution in older patients with certain initial radiological patterns, but the development of pulmonary fibrosis in these patients is still questionable.
La neumonía por la enfermedad por el coronavirus 19 (COVID-19) es la manifestación clínica más frecuente de esta afección, siendo aún desconocidas sus secuelas a largo plazo y la posible evolución a fibrosis pulmonar. El objetivo de este trabajo es una revisión a medio plazo de las secuelas en la radiografía simple de tórax (RxTx) de pacientes con diagnóstico previo de neumonía por la COVID-19.
Pacientes y métodosRevisión retrospectiva de pacientes con diagnóstico de neumonía por la COVID-19 en la que hemos valorado la persistencia de lesiones residuales en la RxTx de control y hemos analizado su posible relación con factores epidemiológicos, factores de riesgo, tratamientos recibidos y patrones radiológicos iniciales.
ResultadosSe analizan 143 pacientes (52 mujeres y 91 hombres). Edad media de 64 años. Se objetivó una resolución completa (RC) radiológica en 104 (73%) y resolución parcial (RP) en 39 (27%). De los factores de riesgo sólo la edad se relacionó significativamente con la persistencia de lesiones residuales (OR 1.06 IC95% (1.02,1.10). En relación con los tratamientos se encontraron diferencias significativas con el tocilizumab y glucocorticoides, donde los pacientes tratados tenían más riesgo de lesiones residuales (OR 2.44 (1.03,5.80) y 3.05(1.43,6.51) respectivamente. En el análisis de los patrones radiológicos se observaron diferencias significativas en los pacientes que presentaban en la evolución aguda condensaciones periféricas y un patrón de empeoramiento radiológico precoz. Se evidenció una disociación clínico-radiológica: de los pacientes con lesiones residuales un 83% no tenían síntomas respiratorios.
DiscusiónLas neumonías por COVID19 pueden tener una resolución radiológica más lenta en pacientes de mayor edad y con ciertos patrones radiológicos iniciales, pero el desarrollo de fibrosis pulmonar en estos pacientes es un hecho aún cuestionable.
The coronavirus-19 disease (COVID-19) pandemic is placing health systems under extreme pressure; and the long-term complications in affected patients are still unknown.
The similarities between COVID-19 and SARS and MERS suggest that there may be a comparable progression to pulmonary fibrosis,1–3 although most studies investigating sequelae in COVID-19 include patients with severe pneumonia, requiring intensive care unit (ICU) admissions. In the case of milder forms, which make up the largest proportion of hospitalised patients, the course is unknown.4,5 If the existence of chronic lung lesions is confirmed in this group of patients, it would be essential to identify risk factors and early markers to implement preventive strategies and appropriate treatments.
This study assesses the radiological evolution in a medium-term follow-up of patients with a clinical-radiological diagnosis of COVID-19 pneumonia who required hospitalization but not ICU admission. The aim is to identify possible indicators of residual lung lesions assessed by chest radiographs (CXR), analysing epidemiological factors, comorbidities, radiological patterns and treatments applied to these patients.
Patients and methodThe cases were retrospectively selected by reviewing the computerised medical records of consecutive patients requiring admission for COVID-19 pneumonia at the Navarra Hospital Complex from 15 March to 1 April 2020. The study was submitted to the ethics committee of our centre, which authorised the study under reference number PI_2020/72.
The inclusion criteria were: patients with a clinical-radiological diagnosis of COVID-19 pneumonia who required hospital admission and who had a baseline CXR and a follow-up CXR. A follow-up CXR was defined as the X-ray performed at least 30 days after the first CXR at the onset of symptoms.
Patients who could not undergo follow-up due to death or other reasons, those who did not have a follow-up CXR (fCXR) and those admitted to ICU were excluded. The latter were not included because we only wanted to assess residual lesions due to COVID-19 and ICU patients might have had other causes of residual lesions, such as respiratory distress, superinfections or mechanical ventilation. CXR was selected as the imaging technique for assessment, as it is the most widely used in routine practice in our setting for initial diagnosis and follow-up, with computed tomography (CT) being reserved for only a few cases.
Diabetes mellitus, hypertension, obesity, chronic obstructive pulmonary disease-asthma and the existence of ischaemic heart disease were assessed as comorbidities and the treatments received were recorded.
Onset and acute course radiological patterns and the persistence of residual lesions in the fCXR were defined by consensus between 2 chest radiologists. The radiological review was done separately, and any discrepancies were resolved by consensus.
The following were considered as radiological patterns at the onset of symptoms: Normal CXR, single opacity, multiple opacities, reticular pattern, interstitial-alveolar pattern and as radiological patterns of acute course: radiological stability, radiological improvement, radiological progression, pyramid (radiological worsening and improvement in that period). Uni or bilateral involvement and the existence of peripheral consolidations in the acute course were identified, as these are a distinctive feature of these pneumonias.
For the present study, a radiological residual lesion is defined as any visible opacity on the CXR that is considered a persistent lesion of previous COVID-19 pneumonia. At follow-up, patients with residual lesions, regardless of extent, were considered to have partial radiological resolution (PR) and those with no residual lesions were considered to have complete radiological resolution (CR).
The data on the respiratory symptoms of the patients in the follow-up visits were reviewed.
Statistical analysisThe association of the variables studied with the presence of residual lesions was analysed using the Chi-square test or Fisher's test for categorical variables and Student's t-test for comparison of means for the age variable.
In all cases the univariate odds ratio was estimated together with its 95% confidence interval. A multivariate logistic model was estimated including all comorbidities, sex and age variables, the effects of treatments were adjusted for all comorbidities and finally a model was estimated with the radiological variables together with sex and age. All contrasts were bilateral, with a significance level of α=0.05. All analyzes were performed with IBM SPSS Statistics v.24 software.
ResultsThe initial sample was 231 cases, with 88 patients being excluded due to not meeting the inclusion criteria. The study population included 143 patients (52 women, 91 men) with a mean age of 64 years (standard deviation [SD]: 13). The mean delay of the fCXR was 67 days (SD: 36). 104 cases (73%) experienced CR and 39 cases (27%) experienced PR. The detailed CR and PR data according to all the variables analyzed and the statistical analysis are collected in Tables 1–4.
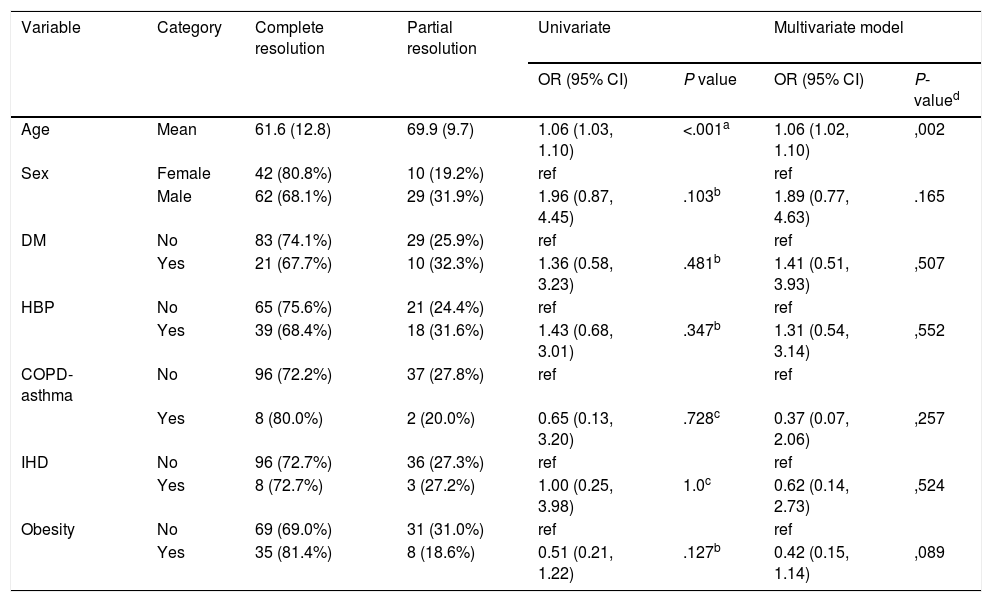
Association of risk factors with the existence of residual lesions. Univariate and multivariate analysis.
| Variable | Category | Complete resolution | Partial resolution | Univariate | Multivariate model | ||
|---|---|---|---|---|---|---|---|
| OR (95% CI) | P value | OR (95% CI) | P-valued | ||||
| Age | Mean | 61.6 (12.8) | 69.9 (9.7) | 1.06 (1.03, 1.10) | <.001a | 1.06 (1.02, 1.10) | ,002 |
| Sex | Female | 42 (80.8%) | 10 (19.2%) | ref | ref | ||
| Male | 62 (68.1%) | 29 (31.9%) | 1.96 (0.87, 4.45) | .103b | 1.89 (0.77, 4.63) | .165 | |
| DM | No | 83 (74.1%) | 29 (25.9%) | ref | ref | ||
| Yes | 21 (67.7%) | 10 (32.3%) | 1.36 (0.58, 3.23) | .481b | 1.41 (0.51, 3.93) | ,507 | |
| HBP | No | 65 (75.6%) | 21 (24.4%) | ref | ref | ||
| Yes | 39 (68.4%) | 18 (31.6%) | 1.43 (0.68, 3.01) | .347b | 1.31 (0.54, 3.14) | ,552 | |
| COPD-asthma | No | 96 (72.2%) | 37 (27.8%) | ref | ref | ||
| Yes | 8 (80.0%) | 2 (20.0%) | 0.65 (0.13, 3.20) | .728c | 0.37 (0.07, 2.06) | ,257 | |
| IHD | No | 96 (72.7%) | 36 (27.3%) | ref | ref | ||
| Yes | 8 (72.7%) | 3 (27.2%) | 1.00 (0.25, 3.98) | 1.0c | 0.62 (0.14, 2.73) | ,524 | |
| Obesity | No | 69 (69.0%) | 31 (31.0%) | ref | ref | ||
| Yes | 35 (81.4%) | 8 (18.6%) | 0.51 (0.21, 1.22) | .127b | 0.42 (0.15, 1.14) | ,089 | |
IHD: ischemic heart disease; DM: diabetes mellitus; COPD: chronic obstructive pulmonary disease; HBP: high blood pressure; OR: odds ratio; Ref: reference category.
Association treatments with the existence of residual lesionsa.
| Variable | Category | Complete resolution | Partial resolution | OR (95% CI) | P-value |
|---|---|---|---|---|---|
| Hydroxychloroquine Rx | No | 12 (85.7%) | 2 (14.3%) | Ref. | |
| Yes | 92 (71.3%) | 37 (28.7%) | 2.41 (0.51, 11.3) | .251b | |
| Kaletra Rx | No | 57 (78.1%) | 16 (21.9%) | Ref. | |
| Yes | 47 (67.1%) | 23 (31.9%) | 1.74 (0.83, 3.68) | .142b | |
| Tocilizumab Rx | No | 88 (76.5%) | 27 (23.5%) | Ref. | |
| Yes | 16 (57.1%) | 12 (42.9%) | 2.44 (1.03, 5.80) | .039b | |
| Glucocorticoid Rx | No | 73 (81.1%) | 17 (18.9%) | Ref. | |
| Yes | 31 (58.5%) | 22 (41.5%) | 3.05 (1.43, 6.51) | .003b | |
| Anakinra Rx | No | 98 (73.7%) | 35 (26.3%) | Ref. | |
| Yes | 6 (60.0%) | 4 (40.0%) | 1.87 (0.50, 7.01) | .461c | |
| Other Rx | No | 94 (73.4%) | 34 (26.6%) | Ref. | |
| Yes | 10 (66.7%) | 5 (33.3%) | 1.38 (0.44, 4.34) | .553c |
OR: odds ratio; ref: reference category; Rx: treatment.
Association of radiological factors and delayed symptoms with the existence of residual lesions.
| Variable | Category | Complete resolution | Partial resolution | OR (95% CI) | P value |
|---|---|---|---|---|---|
| Initial X-ray | Normal | 17 (70.8%) | 7 (29.2%) | ref | |
| Single opacity | 14 (82.4%) | 3 (17.6%) | 0.52 (0.11, 2.39) | ||
| Multiple opacities | 23 (67.6%) | 11 (32.4%) | 1.16 (0.37, 3.62) | .835a | |
| Reticular pattern | 27 (71.1%) | 11 (28.9%) | 0.99 (0.32, 3.05) | ||
| Interstitium-alveolar | 23 (76.7%) | 7 (23.3%) | 0.74 (0.22, 2.51) | ||
| Laterality | Unilateral | 23 (79.3%) | 6 (20.7%) | ref | |
| Bilateral | 64 (71.1%) | 26 (28.9%) | 1.56 (0.57, 4.26) | .386b | |
| Acute course one month | Progression | 32 (60.4%) | 21 (39.6%) | ref | |
| Pyramid | 26 (68.4%) | 12 (31.6%) | 0.70 (0.29, 1.69) | ||
| Stable | 24 (82.8%) | 5 (17.2%) | 0.32 (0.11, 0.96) | .004b | |
| Improvement | 20 (100.0%) | 0 (0.0%) | -- | ||
| Peripheral consolidations | No | 58 (82.9%) | 12 (17.1%) | ref | |
| Yes | 44 (62.9%) | 26 (37.1%) | 2.86 (1.30, 6.26) | .008b | |
| Delayed symptoms | Normal | 70 (70.0%) | 30 (20.0%) | ref | |
| Symptomatic | 20 (76.9%) | 6 (23.1%) | 0.70(0.26,1.92) | .486b |
OR: odds ratio; ref: reference category; Rx: chest x-ray.
Of the risk factors, only age clearly appears to be related to the variable of residual lesions during follow-up (OR: 1.06; 95% CI: 1.02–1.10). The other variables showed no significant differences. Notably, obesity appears to have a protective effect, but not statistically significant (OR: 0.42 [0.15–1.14]).
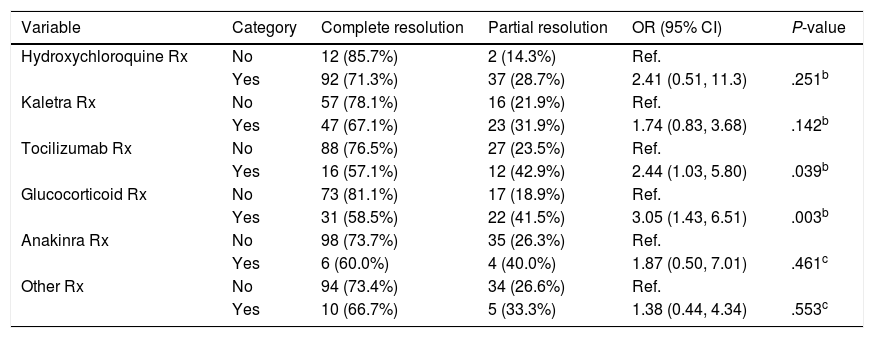
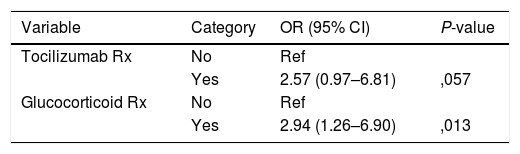
In relation to the treatments, significant differences were found in the treatments with tocilizumab and glucocorticoids, where the treated patients had a higher risk of residual lesions (OR: 2.44 [1.03–5.80] and 3.05 [1, 43–6.51]) respectively.
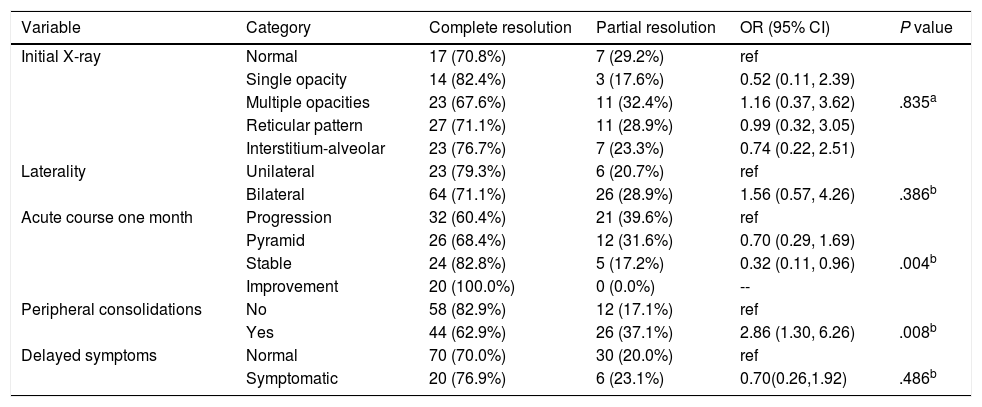
The radiological findings analysis detailed in the Table 4 found no differences in the persistence of residual lesions according to the different initial radiological involvement patterns (normal CXR, single or multiple opacity, reticular pattern, interstitial-alveolar pattern), and no differences were found regardless of whether the initial radiological involvement was unilateral or bilateral. Significant differences were found according to the type of radiological progression in the initial acute period (progression, pyramid, stability or improvement). Patients with radiological progression or worsening in the first few days had more residual lesions on the follow-up CXR, up to 39.6% of cases, as did patients with peripheral consolidation during progression, who had residual lesions in 37.15% of cases, compared to 17.1% of those who did not have them.
There was no evidence of a relationship between the existence of residual lesions and respiratory symptoms in the assessment of the latter. Of the patients who presented residual lesions, 83% had no symptoms.
DiscussionLong-term follow-up of patients with COVID-19 pneumonia remains to be established. There are already some guidelines in the literature6 that propose different patient follow-ups depending on the severity of COVID-19 pneumonia. It should be noted that in this follow-up, CXR is the initial basic imaging test to assess residual lesions.
This study adds to the current scientific literature preliminary data on the course of COVID-19 pneumonias that did not require ICU admission, showing complete radiological resolution in 73% of cases at one-month follow-up, a finding previously described in SARS and MERS cases at 12 weeks6 and similar to the 70% resolution rate at one month in community-acquired pneumonia.7
Radiological resolution was slower in older patients, a fact that coincides with that described in the literature.4,8,9 A slower resolution was also observed in patients treated with tocilizumab and glucocorticoids, which could be justified by the bias derived from the indication of these treatments due to increased laboratory parameters of inflammation and severity of pneumonia.
With regard to the radiological analysis, radiological progression in the acute control and the existence of peripheral consolidations were significantly related to the persistence of lesions, constituting possible radiological indicators of residual lesions.
A clinical-radiological dissociation was evident in our series, as there was no relationship between the existence of residual radiological lesions and the persistence of respiratory symptoms, which could lead to questioning the clinical significance of these residual lesions.
Our study has certain limitations, the most important of which are the limited number of patients analysed, the retrospective nature of the study, the fact that the existence of residual lesions is determined with CXR and not with CT, that there is no correlation with respiratory function tests and that there is no long-term follow-up.
From the data obtained, we conclude that COVID-19 pneumonias that did not require admission to the ICU may have a slow radiological improvement in older patients and with radiological progression and peripheral consolidation in the acute phase, but this does not necessarily entail persistence of respiratory symptoms; we also observed a rate of complete radiological resolution similar to other pneumonias, so progression to pulmonary fibrosis in this group of patients is unlikely. Further long-term studies with a larger number of patients are needed to confirm these conclusions.
FundingThis article has not received any type of funding.
Conflict of interestsThe authors declare that they have no conflict of interest.
Please cite this article as: Gómez Herrero H, Galbete A, Álvarez Galván B, Caballero García P, Vicaría Fernández I. Lesiones residuales en radiografía simple de tórax tras neumonía por SARS-CoV-2: identificación de factores de riesgo. Med Clin (Barc). 2022;158:418–421.