Death and unexpected readmission are frequent among heart failure patients. We aimed to assess 30-day readmission and mortality rate as well as to identify predictive factors for patients discharged from a first HF related hospital admission.
Methods and resultsRetrospective, single-center, cohort study, using administrative data from a tertiary care hospital in Barcelona, Spain. Patients discharged alive from a first HF related admission from 2010 to 2014 were assessed for 30-day death, readmission and adverse outcome rate. A Linear Logistic Regression Model was fitted for each outcome.
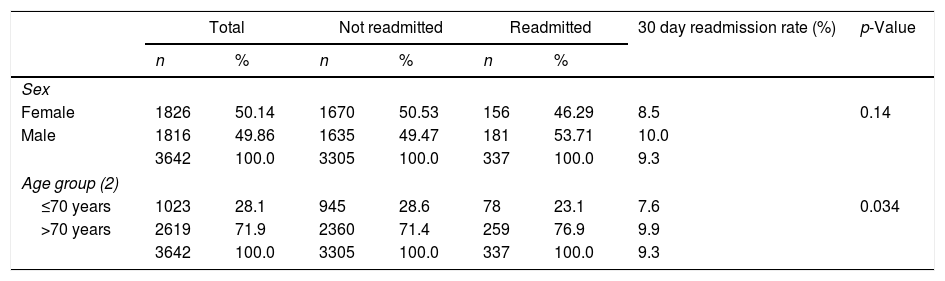
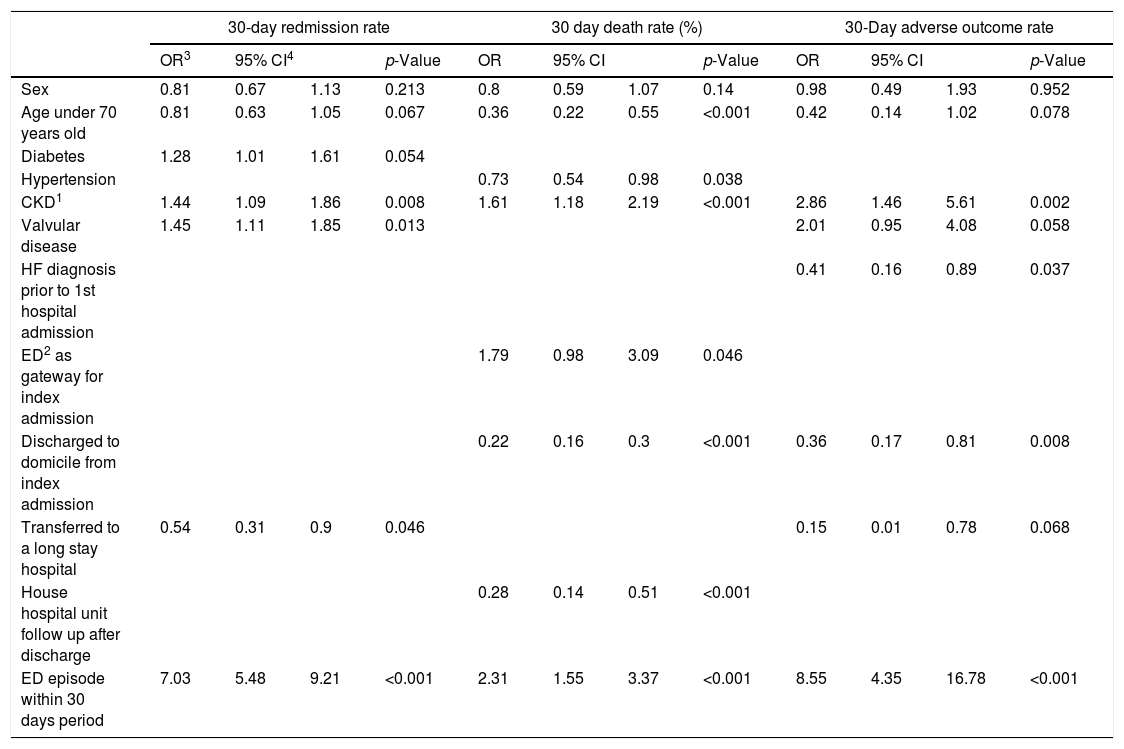
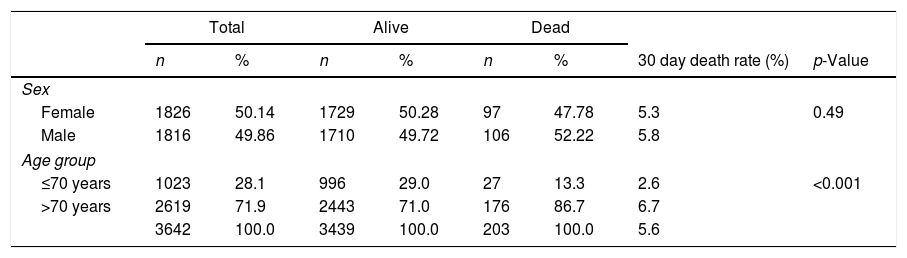
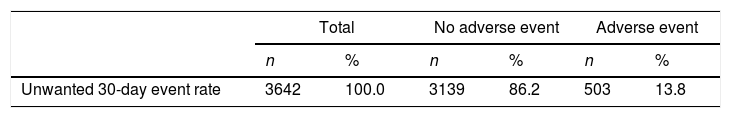
The set accounted for 3642 patients; 50.1% female and 49.9% male. Mean age was 76 years (SD=12). 30-Days rates were 9.2% for readmission, 5.6% for death and 13.8% for adverse outcome. Admission to an ED within 30 days was strongly linked to readmission (OR=6.97), death (OR=2.31) and adverse outcome (OR=8.55), as well as chronic kidney disease (OR=1.44/1.61/2.86 respectively). Discharge to a Long Stay Care (LSC) facility was linked to lower readmission and adverse event rates (OR=.57 and OR=.15).
ConclusionPre and post-index discharge use of health care resources is related to adverse outcome rates. Our findings point out the potential benefit for a more tailored approach in the management of HF patients.
La muerte y readmisión no programada son frecuentes en pacientes con insuficiencia cardiaca (IC). En este estudio evaluamos las tasas y los factores predictivos de muerte y readmisión a 30 días tras el alta de una primera hospitalización por IC.
Métodos y resultadosSe trata de un estudio de cohorte retrospectivo, unicéntrico, que utiliza datos administrativos de un hospital de tercer nivel en Barcelona, España. Para los pacientes dados de alta vivos, tras un primer episodio de hospitalización por IC descompensada, entre 2010 y 2014, se calcularon las tasas de muerte, readmisión y evento adverso durante los 30 días tras el alta. Para cada variable de interés se ajustó un modelo de regresión logística.
La muestra constaba de 3.642 pacientes: 50,1% mujeres y 49,9% varones con una edad media de 76 años (DE=12). Las tasas a los 30 días fueron del 9,2% para la readmisión, 5,6% para la muerte y 13,8% para el evento adverso. Haber sido visitado un servicio de urgencias en el periodo de estudio se asoció a una mayor tasa de readmisión (OR=6,97), muerte (OR=2,31) y evento adverso (OR=8,55), del mismo modo que la insuficiencia renal crónica (OR=1,44/1,61/2,86, respectivamente). El traslado al alta a un centro de larga estancia se asoció a una menor tasa de admisiones y eventos adversos (OR=0,57 y OR=0,15).
ConclusionesEl uso de servicios sanitarios pre y postalta guarda una clara relación con la tasa de eventos adversos. Nuestros resultados indican el beneficio potencial de un manejo personalizado de los pacientes con IC.