Outpatient surgery has become more popular amongst patients with more complex morbidities as well as for more complex and more invasive procedures. In the same vein, we ought to stress the importance of improving postoperative recovery conditions in order to enable the patient's discharge and fast reintegration to his/her everyday activities. To that end, we must have wide control of the patient's physical condition from the preoperative stage. That is, to place patients in an optimal health status to the extent possible prior to procedure and search for more adequate anesthetic techniques to optimize surgical conditions, and thus try to ensure a fast recovery with minimum side effects and preventing possible postoperative complications.
In order to accomplish this, multidisciplinary work is required for the perioperative care, where anesthesiologists play a major role.
For all practical purposes, we can conceptualize outpatient surgery as a qualified surgery. That is, a true surgery conducted within the safety framework provided by an operating room. The term “outpatient” can be defined as any medical, organizational and administrative practice which allows for the patient to leave the clinic on the same day the procedure took place (hospital stay must be less than or equal to 12h).
According to the Mexican NOM-026-SSA3-2012 for the practice of major outpatient surgery, section 4.2 states that the patient's discharge from the Major Outpatient Surgery Unit will be made within a time lapse no longer than 12h, considering from the moment they were admitted, during which the surgical act took place and their post-anesthetic recovery had concluded.1 Around 40% of surgeries today are of this modality, leaving a considerable progression margin. The objective is to reach first world countries’ rates, which are close to 80%.
Institutions which have structures for outpatient surgery are subjected to regulation. Outpatient surgery is an alternative to a practice usually performed under traditional hospitalization and only concerns those patients who are to undergo medical intervention or a surgical procedure impracticable in the physician's office. Nevertheless, even though some external practices are conducted under the Outpatient Surgery Unit framework, these are not applicable to the regulations (safety, organization), resource assignation or relative rate fixation to outpatient surgery.1 Outpatient structure should ensure the patient and organization and function which contemplates all these imperatives.
The final choice regarding the selection of a patient, an operation or medical intervention of outpatient assistance is the responsibility of the anesthesiologist and the physician in charge of intervention, if the latter were to be involved. The competence of the physicians who administer anesthesia ought to be adapted to the patient's status, the procedure, and comorbidities.
The International Association for Ambulatory Surgery (IAAS) and the Association Française de Chirurgie Ambulatoire (AFCA by its French acronym)agree on the fact that the list of interventions where an outpatient treatment is justified are unnecessary. The decision of indicating a treatment of this sort is the responsibility of the surgeon and anesthesiologist, always according to the conditions or physical state of the patient, type of surgery and conditions of the place.2 However, it would be convenient to have a clear consensus amongst physicians with previously established rules and procedures, especially about conduct related to duration and follow-up.
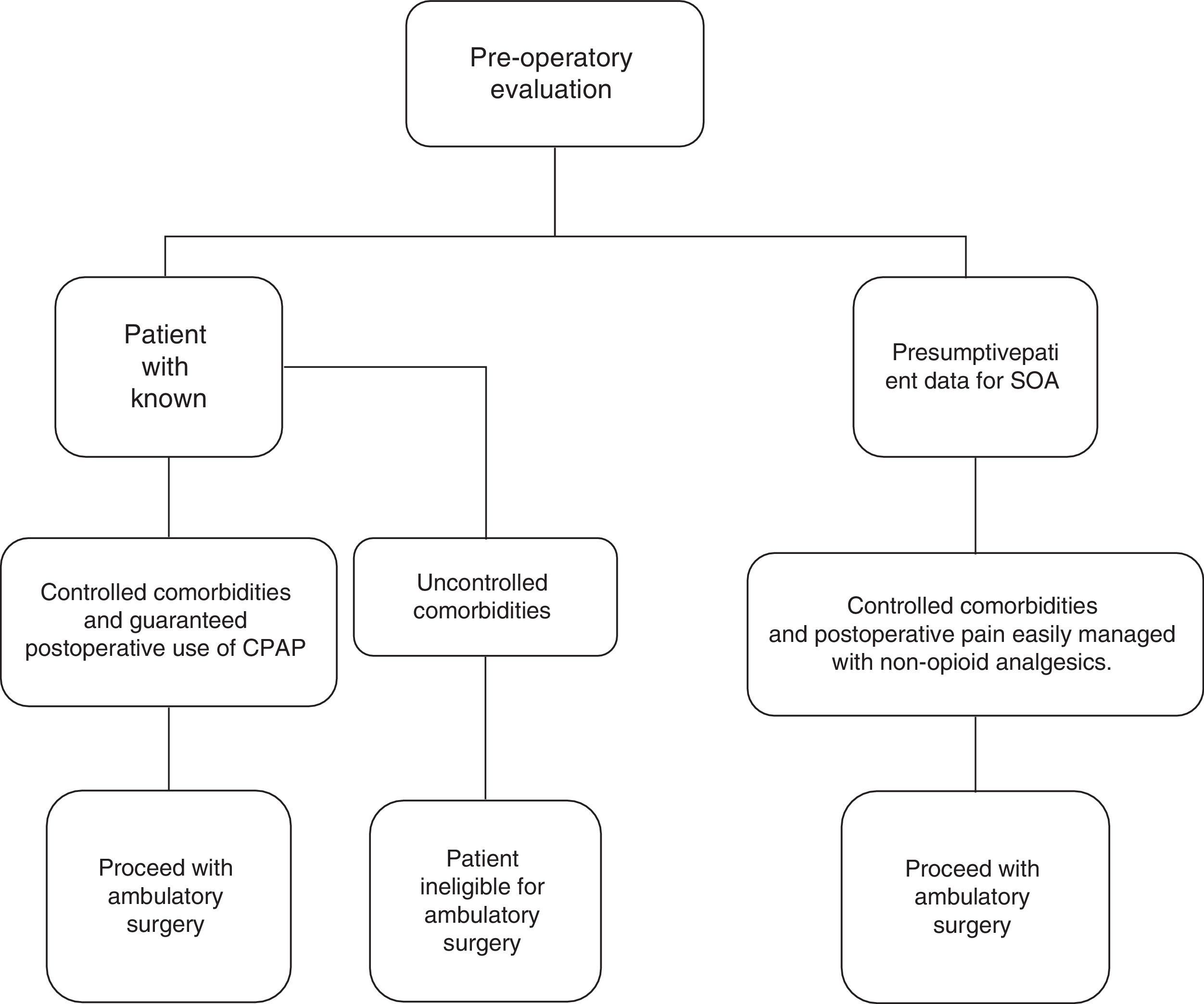
The Society for Ambulatory Anesthesia conducted a consensus for the elaboration of an algorithm in the selection of adult patients with sleep obstructive apnea syndrome (SOA) programed for outpatient surgery (Fig. 1), which is guided according to comorbidities and the use of CPAP and other factors, thus facilitating the specialists’ decision whether or not to proceed to outpatient surgery with these kinds of patients.
Society for Ambulatory Anesthesia Consensus Statement on Preoperative Selection of Adult. Patients with Obstructive Sleep Apnea Scheduled for Ambulatory Surgery Girish P. Joshi, MBBS, MD, FFARSCI,* Saravanan P. Ankichetty, MD, DA, MBA,† Tong J. Gan, MD, MHS, FRCA,‡ and Frances Chung, MBBS, FRCPC†.
On the other hand, the American Society of Anesthesiologists (ASA), using a different consensus, established a series of criteria through which we are able to guide the selection of cases and patients. Below are the criteria:
Selection criteria for patients for outpatient anesthesia- •
American Society of Anesthesiologists (ASA) class I, II or III stabilized.
- •
Age: no children under six months of age; advanced age is not a contraindication.
- •
Urgency contraindication (with certain restrictions).
- •
The patient ought to be accompanied during his return home.
- •
A responsible person ought to accompany the patient during the night following intervention.
- •
The patient must have a working phone line.
- •
The patient's address must be less than 1h from the health center (or at least from a care unit)
- •
It is indispensable for the patient to have a good comprehension level.
Today, the most severe complications (respiratory failure, severe myocardium infarct, pulmonary thromboembolism) and mortality in outpatient surgery are not frequent. Mortality is reported to be as low as 1 in every 11,273 patients, and adverse effects rate is 0.08%.
ComorbiditiesMost diseases do not represent a contraindication for outpatient modality. However, some should be taken into account according to their severity, due to the potential risks (essentially respiratory or cardiocirculatory): morbid obesity, sleep apnea syndrome, coronaropathy, asthma, renal failure, etc. Regarding ASA III patients, Ansell et al. have retrospectively evaluated the evolution in these types of patients after an outpatient surgery. Out of the 30,000 patients treated in outpatient modality between 1998 and 2002, 3.3% were classified as ASA III.
AgeSeveral studies have evaluated the influence of age on outpatient surgery perioperative complications. Some results are contradictory. A cohort studywith over 15,000 patients reveals that age is not predictive of hospitalization after outpatient surgery. However, Chung et al. have demonstrated an association between an age over 65 and a rise in the risk of intraoperative complications, especially cardiovascular ones. On the other hand, incidence of postoperative adverse occurrences (PONV, pain, vertigo) was significantly lower in patients of advanced age. Fleisher et al. analyzed death and hospitalization risk factors after an outpatient surgery. For death risk or hospital readmission within seven days after surgery, the most significant factorsrelated to the patient, were an age over 85 years and a hospitalization in the months previous to surgery.
The surgeon is the one who decides the indication of outpatient surgery for any given surgical intervention, and the anesthesiologist is the one who confirms the feasibility of the procedure during the anesthetic consultation. The NOM-026-SSA3-2012 for the practice of major outpatient surgery section 6.1.2 states that pre-anesthetic assessment and the medical specialties which result, ought to take place within five days prior to surgery. Also, the patient ought to be in an ASA I or II physical status as stated in section 6.1.3.
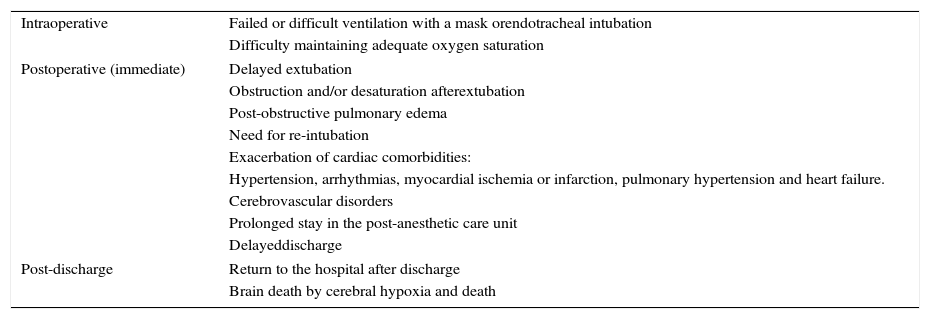
Sleep obstructive apnea syndrome (SOA)Sleep obstructive apnea syndrome is a common problem which is being detected more and more frequently. However, there is a lack of research culture in the patient as well as in the physician, a culture of intentionally searching for clinical data which leads us to a diagnosis for it, especially prior to a surgical procedure. This is linked to somnolence during the day, cognitive dysfunction, and cardiovascular problems such as hypertension, ischemic cardiac disease, arrhythmias, pulmonary hypertension and congestive heart failure, as well as metabolic dysfunction and a decrease in quality of life.3 (Table 1)
Considerations for patients with sleep obstructive apnea syndrome in ambulatory surgery.
| Intraoperative | Failed or difficult ventilation with a mask orendotracheal intubation |
| Difficulty maintaining adequate oxygen saturation | |
| Postoperative (immediate) | Delayed extubation |
| Obstruction and/or desaturation afterextubation | |
| Post-obstructive pulmonary edema | |
| Need for re-intubation | |
| Exacerbation of cardiac comorbidities: | |
| Hypertension, arrhythmias, myocardial ischemia or infarction, pulmonary hypertension and heart failure. | |
| Cerebrovascular disorders | |
| Prolonged stay in the post-anesthetic care unit | |
| Delayeddischarge | |
| Post-discharge | Return to the hospital after discharge |
| Brain death by cerebral hypoxia and death | |
A clinical practical guide for perioperative patients with sleep obstructive apnea syndrome indicates that patients with SOA have an elevated morbidity and mortality risk due to the potential difficulty of airway management. The ASA states the evaluation allow for a timely identification of patients with SOA, including (1) research of medical background, (2) interview with the patient and relative, (3) physical examination.
During the scrutiny of patients with probable SOA diagnosis, we must interrogate the patient and his/her family, focused on a history of snoring, apnea episodes, sudden awakenings during the night, morning headaches and sleepiness throughout the day. Physical examination should include airway evaluation as well as characteristics of the nasopharynx and tongue size. The anesthesiologist and surgeon must decide whether to handle the patient perioperatively based solely on clinical criteria or to complement it with more extensive studies and begin treatment. In any case, the patient and their relatives should be informed of the potential complications during the procedure in a patient with SOA. Regarding preoperative preparation recommendations, it is recommended to use a CPAP device or any device for non-invasive ventilation, and the use of a mandibular advance device and weight loss if necessary.
In patients with diagnosed SOA, perioperative complications have been linked to a relationship between comorbidities and the use of opioids. Patients who do not maintain a proper medical control are not candidates for outpatient surgery. Among the complications which have been linked to this disease are hypoxemia, arrhythmias, myocardium ischemic damage, unanticipated admittance to the intensive care unit and sudden death.
Advanced age itself does not necessarily represent a contraindication for outpatient surgery, taking into account the patient's comorbidities, general functional state and physiological reserves. Nevertheless, there is a statistically significant increased risk of perioperative mortality.4
FundingNo financial support was provided.