Dementia is characterised by cognitive deterioration and the manifestation of psychological and behavioural symptoms, especially changes in perception, thought content, mood, and conduct. In addition to drug therapy, non-pharmacological treatments are used to manage these symptoms, and one of these latter treatments is music therapy. Since this novel technique in non-verbal, it can be used to treat patients with dementia at any stage, even when cognitive deterioration is very severe. Patients’ responses to music are conserved even in the most advanced stages of the disease.
DevelopmentA literature research was carried out using the following databases: Academic Search Complete, PubMed, Science Direct y Dialnet. The period of publication was 2003 to 2013 and the search keywords were ‘Music Therapy, Dementia, Behaviour, Behaviour Disorders y Behavioural Disturbances’. Out of the 2188 studies that were identified, 11 studies met inclusion criteria for the systematic review.
ConclusionsMusic therapy is beneficial and improves behaviour disorders, anxiety and agitation in subjects diagnosed with dementia.
La demencia se caracteriza por un deterioro cognitivo y por la aparición de síntomas psicológicos y conductuales, entre los que destacan las alteraciones de percepción, del contenido del pensamiento, estado de ánimo y de conducta. Para tratar estos síntomas, además del tratamiento farmacológico, se utilizan intervenciones no farmacológicas, entre ellas la musicoterapia. Esta técnica novedosa, por sus características no verbales, puede ser usada en todas las fases del tratamiento de las personas con demencia ya que, aunque haya un gran deterioro cognitivo, las respuestas ante la música se mantienen hasta los estadios más avanzados de la enfermedad.
DesarrolloSe realizó una búsqueda bibliográfica con un intervalo temporal entre 2003 y 2013 en las bases de datos Academic Search Complete, PubMed, Science Direct y Dialnet. Los términos de búsqueda incluyeron la combinación de las palabras claves «music therapy, dementia, behaviour, behavioural disorders y behavioural disturbances». Se seleccionaron 11 registros de los 2188 localizados tras aplicar los criterios de inclusión.
ConclusionesEl tratamiento con musicoterapia es beneficioso para mejorar las alteraciones conductuales, la ansiedad y la agitación en pacientes con demencia.
Dementia is characterised by impairment of the cognitive functions and it leads to increasing difficulty in performing daily activities, fulfilling social functions, and remaining independent.1
Its symptoms can be categorised as loss of cognitive functions, symptoms associated with abnormal conduct or behavioural problems, changes in behaviour and personality, symptoms related to activities of daily living, and loss of ability to perform them.2
The social consequences of cognitive impairment include anxiety, sorrow, frustration, apathy, and irritability and lead to isolation and in many cases to depression, which in turn may cause behavioural alterations in these patients.1
In general, these behavioural changes exacerbate as the disease progresses.3 According to a study by Wragg, depression is present in 40% to 50% of all patients with Alzheimer disease (AD)4; the frequency of delirium and delusional ideation ranges between 10% and 73%; hallucinations, predominantly visual and auditory, can affect 15% to 50%; pacing or wandering is more pronounced at night as a consequence of nocturnal disorientation and affects approximately 60% of the patients with dementia; psychomotor uneasiness or agitation, which is sometimes accompanied by other exacerbating disturbances such as anxiety or insomnia, can manifest in intermediate and advanced stages of the disease.5
Medical evidence shows that behaviour problems in elderly patients with dementia are usually managed with drugs, but these pharmacological treatments are associated with adverse effects.1,6 Although these drugs are not able to resolve dementia, they are somewhat effective in delaying impairment progression, in addition to helping control associated mental illnesses.7 However, there is now a wide range of non-pharmacological strategies to treat behavioural problems. Among these strategies, music therapy is worth mentioning.8
According to the World Federation for Music Therapy (WFMT, 1996), music therapy is “the use of music and/or musical elements (sound, rhythm, melody and harmony) by a qualified music therapist, with a client or group, in a process designed to facilitate and promote communication, relationships, learning, mobilisation, expression, organisation, and other relevant therapeutic objectives, in order to meet physical emotional, mental, social and cognitive needs”.9
As in other healthcare disciplines, clinical practice standards for music therapy are aimed at establishing basic action procedures (AMTA Standards of clinical practice, 2007). According to these procedures, all music therapy intervention must comprise the following stages: patient referral (and acceptance) of therapy, initial evaluation, planning, therapy implementation, documentation, and termination/discharge.9
This therapy is applied in different settings and contexts to a wide variety of patient groups. In geriatric medicine, according to independence and functional levels of elderly patients, music therapy can be used in civic centres, retirement homes, day care centres, day hospitals, patient associations, geriatric residences, and private homes.9
Responsiveness to music may be preserved even in very late stages of dementia.2 While language deteriorates over the course of the disease, some musical skills are still preserved, such as the ability to play a previously learnt piece of music or a musical instrument.9
Music therapy can modulate the factors involved in cognition and conduct, call the patient's attention, provoke emotional responses and modulate them, draw on different cognitive functions, and evoke movement patterns.10
In light of the above, the aim of our review article is to ascertain the conclusions of scientific publications regarding the benefits of music therapy on behavioural problems in elderly patients with dementia.
DevelopmentWe conducted a systematic review of randomised controlled trials and clinical trials on the benefits of music therapy for behavioural problems secondary to dementia. Inclusion criteria are articles published in English or Spanish from January 2003 to January 2013 that include patients diagnosed with dementia, aged 65 or older, who had participated in music therapy interventions and presented changes in their problematic behaviours, agitation, and anxiety in general. We excluded publications older than 10 years, literature reviews, and studies other than clinical trials.
Two independent reviewers (M.J. and M.G.) searched, selected, and reviewed the articles found. In cases of disagreement, results were put forward and consensus was reached.
We used the Academic Search Complete, PubMed, Science Direct, and Dialnet electronic databases.
For searching the Science Direct and Dialnet databases, we combined the following keywords: music therapy, dementia, behaviour, behavioural disorders, and behavioural disturbances (‘musicoterapia’, ‘demencia’, ‘conducta’, and ‘alteraciones conductuales’ in Spanish). In the Academic Search Complete database, we used the keywords ‘music therapy’, ‘dementia’, and ‘behaviour’ (‘musicoterapia’, ‘demencia’, ‘conducta’ in Spanish). Only keywords in English were used in the PubMed database.
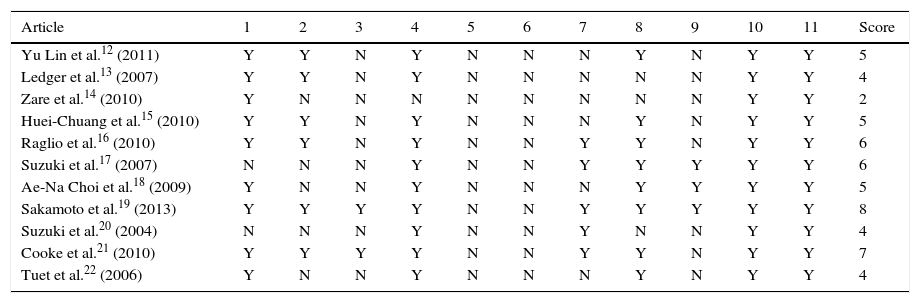
Methodological quality of the studies we included was measured on the PEDro (Physiotherapy Evidence Database)11 scale, which indicates trial quality. It includes 11 items which can be answered ‘yes’ (Y) or ‘no’ (N); total scores range from 0 to 10, which indicates low to excellent methodological quality. Criteria 2 to 9 are intended to determine whether the study has sufficient internal validity, criteria 10 and 11 assess whether statistical information is sufficient to interpret results, and the external validity is related to criterion 1. This last criterion is supplementary and cannot be used to calculate the score; the maximum score which can be obtained is therefore 10 and not 11.
The 11 criteria assessed with the PEDro scale are as follows:
1. Eligibility criteria; 2. random allocation; 3. concealed allocation; 4. baseline similarity; 5. blinding of subjects; 6. blinding of therapists; 7. blinding of assessors; 8. follow-up of subjects (at least 85% of total); 9. intention to treat analysis; 10. between-group statistical comparisons; 11. point measures and measures of variability.
According to the values on the scale, we can rate studies as follows:
High quality when the score obtained is higher than 5 (6–8: good, 9–10: excellent); moderate quality when the score is 4 or 5 (fair); and low quality when the score is lower than 4 (poor).
Study selectionAs a general rule, we preselected publications considering their potential suitability given the topic of this review.
We selected full versions of articles and read their abstracts to exclude those articles that did not fulfil the previously listed inclusion criteria.
The publications meeting the criteria were read so as to be subsequently analysed and included in our review article.
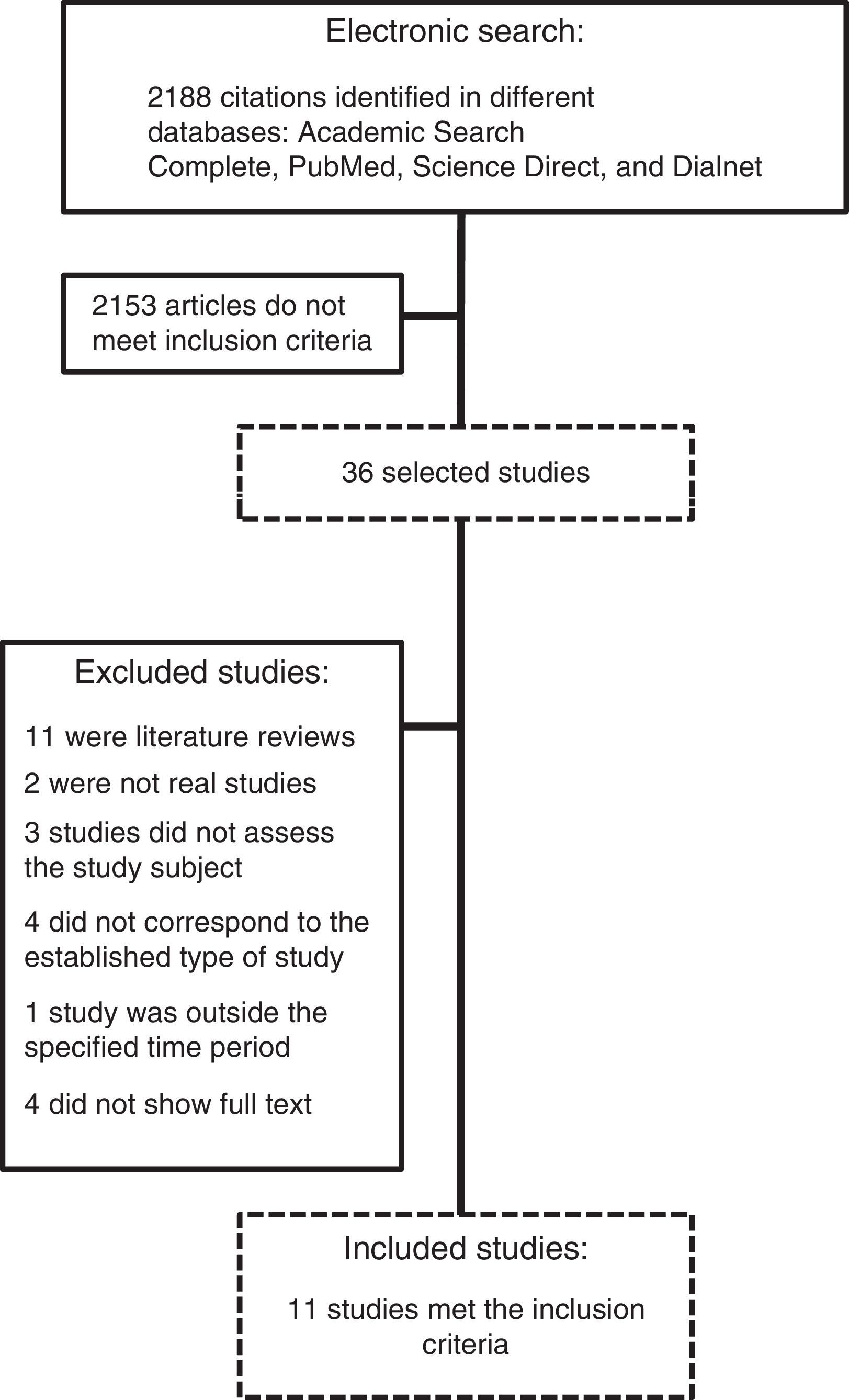
ResultsOf the 2188 articles identified during the literature search, 11 were selected according to the inclusion and exclusion criteria presented in the development section. The search process and the selection of the applicable studies is summarised in Fig. 1.
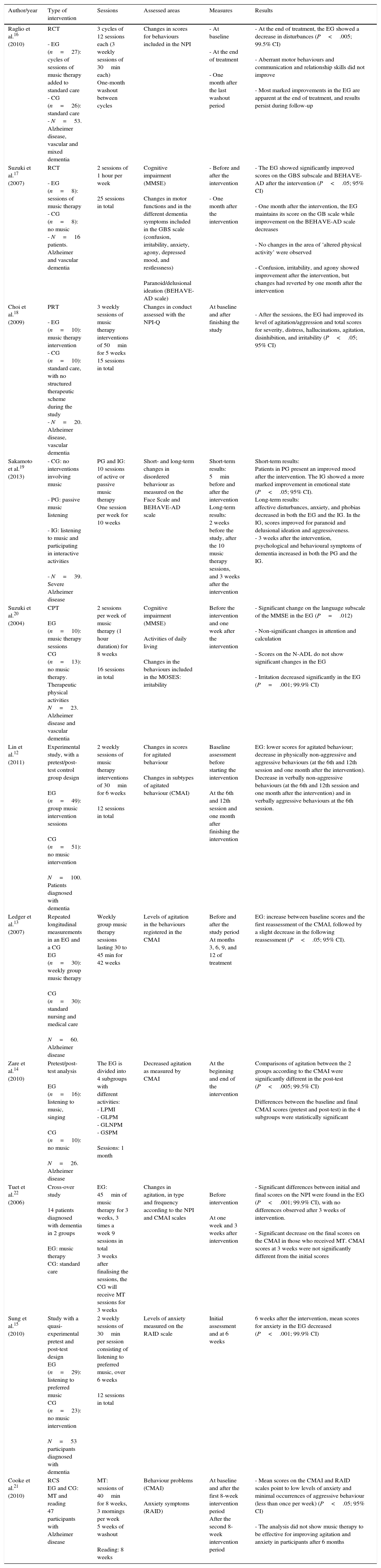
Description of studiesThe main characteristics of the studies included in this review are summarised in Table 1.
Characteristics of the studies included in our review article.
| Author/year | Type of intervention | Sessions | Assessed areas | Measures | Results |
|---|---|---|---|---|---|
| Raglio et al.16 (2010) | RCT - EG (n=27): cycles of sessions of music therapy added to standard care - CG (n=26): standard care - N=53. Alzheimer disease, vascular and mixed dementia | 3 cycles of 12 sessions each (3 weekly sessions of 30min each) One-month washout between cycles | Changes in scores for behaviours included in the NPI | - At baseline - At the end of treatment - One month after the last washout period | - At the end of treatment, the EG showed a decrease in disturbances (P<.005; 99.5% CI) - Aberrant motor behaviours and communication and relationship skills did not improve - Most marked improvements in the EG are apparent at the end of treatment, and results persist during follow-up |
| Suzuki et al.17 (2007) | RCT - EG (n=8): sessions of music therapy - CG (n=8): no music - N=16 patients. Alzheimer and vascular dementia | 2 sessions of 1 hour per week 25 sessions in total | Cognitive impairment (MMSE) Changes in motor functions and in the different dementia symptoms included in the GBS scale (confusion, irritability, anxiety, agony, depressed mood, and restlessness) Paranoid/delusional ideation (BEHAVE-AD scale) | - Before and after the intervention - One month after the intervention | - The EG showed significantly improved scores on the GBS subscale and BEHAVE-AD after the intervention (P<.05; 95% CI) - One month after the intervention, the EG maintains its score on the GB scale while improvement on the BEHAVE-AD scale decreases - No changes in the area of ‘altered physical activity’ were observed - Confusion, irritability, and agony showed improvement after the intervention, but changes had reverted by one month after the intervention |
| Choi et al.18 (2009) | PRT - EG (n=10): music therapy intervention - CG (n=10): standard care, with no structured therapeutic scheme during the study - N=20. Alzheimer disease, vascular dementia | 3 weekly sessions of music therapy interventions of 50min for 5 weeks 15 sessions in total | Changes in conduct assessed with the NPI-Q | At baseline and after finishing the study | - After the sessions, the EG had improved its level of agitation/aggression and total scores for severity, distress, hallucinations, agitation, disinhibition, and irritability (P<.05; 95% CI) |
| Sakamoto et al.19 (2013) | - CG: no interventions involving music - PG: passive music listening - IG: listening to music and participating in interactive activities - N=39. Severe Alzheimer disease | PG and IG: 10 sessions of active or passive music therapy One session per week for 10 weeks | Short- and long-term changes in disordered behaviour as measured on the Face Scale and BEHAVE-AD scale | Short-term results: 5min before and after the intervention Long-term results: 2 weeks before the study, after the 10 music therapy sessions, and 3 weeks after the intervention | Short-term results: Patients in PG present an improved mood after the intervention. The IG showed a more marked improvement in emotional state (P<.05; 95% CI). Long-term results: affective disturbances, anxiety, and phobias decreased in both the EG and the IG. In the IG, scores improved for paranoid and delusional ideation and aggressiveness. - 3 weeks after the intervention, psychological and behavioural symptoms of dementia increased in both the PG and the IG. |
| Suzuki et al.20 (2004) | CPT EG (n=10): music therapy sessions CG (n=13): no music therapy. Therapeutic physical activities N=23. Alzheimer disease and vascular dementia | 2 sessions per week of music therapy (1 hour duration) for 8 weeks 16 sessions in total | Cognitive impairment (MMSE) Activities of daily living Changes in the behaviours included in the MOSES: irritability | Before the intervention and one week after the intervention | - Significant change on the language subscale of the MMSE in the EG (P=.012) - Non-significant changes in attention and calculation - Scores on the N-ADL do not show significant changes in the EG - Irritation decreased significantly in the EG (P=.001; 99.9% CI) |
| Lin et al.12 (2011) | Experimental study, with a pretest/post-test control group design EG (n=49): group music intervention sessions CG (n=51): no music intervention N=100. Patients diagnosed with dementia | 2 weekly sessions of music therapy interventions of 30min for 6 weeks 12 sessions in total | Changes in scores for agitated behaviour Changes in subtypes of agitated behaviour (CMAI) | Baseline assessment before starting the intervention At the 6th and 12th session and one month after finishing the intervention | EG: lower scores for agitated behaviour; decrease in physically non-aggressive and aggressive behaviours (at the 6th and 12th session and one month after the intervention). Decrease in verbally non-aggressive behaviours (at the 6th and 12th session and one month after the intervention) and in verbally aggressive behaviours at the 6th session. |
| Ledger et al.13 (2007) | Repeated longitudinal measurements in an EG and a CG EG (n=30): weekly group music therapy CG (n=30): standard nursing and medical care N=60. Alzheimer disease | Weekly group music therapy sessions lasting 30 to 45 min for 42 weeks | Levels of agitation in the behaviours registered in the CMAI | Before and after the study period At months 3, 6, 9, and 12 of treatment | EG: increase between baseline scores and the first reassessment of the CMAI, followed by a slight decrease in the following reassessment (P<.05; 95% CI). |
| Zare et al.14 (2010) | Pretest/post-test analysis EG (n=16): listening to music, singing CG (n=10): no music N=26. Alzheimer disease | The EG is divided into 4 subgroups with different activities: - LPMI - GLPM - GLNPM - GSPM Sessions: 1 month | Decreased agitation as measured by CMAI | At the beginning and end of the intervention | Comparisons of agitation between the 2 groups according to the CMAI were significantly different in the post-test (P<.005; 99.5% CI) Differences between the baseline and final CMAI scores (pretest and post-test) in the 4 subgroups were statistically significant |
| Tuet et al.22 (2006) | Cross-over study 14 patients diagnosed with dementia in 2 groups EG: music therapy CG: standard care | EG: 45min of music therapy for 3 weeks, 3 times a week 9 sessions in total 3 weeks after finalising the sessions, the CG will receive MT sessions for 3 weeks | Changes in agitation, in type and frequency according to the NPI and CMAI scales | Before intervention At one week and 3 weeks after intervention | - Significant differences between initial and final scores on the NPI were found in the EG (P<.001; 99.9% CI), with no differences observed after 3 weeks of intervention. - Significant decrease on the final scores on the CMAI in those who received MT. CMAI scores at 3 weeks were not significantly different from the initial scores |
| Sung et al.15 (2010) | Study with a quasi-experimental pretest and post-test design EG (n=29): listening to preferred music CG (n=23): no music intervention N=53 participants diagnosed with dementia | 2 weekly sessions of 30min per session consisting of listening to preferred music, over 6 weeks 12 sessions in total | Levels of anxiety measured on the RAID scale | Initial assessment and at 6 weeks | 6 weeks after the intervention, mean scores for anxiety in the EG decreased (P<.001; 99.9% CI) |
| Cooke et al.21 (2010) | RCS EG and CG: MT and reading 47 participants with Alzheimer disease | MT: sessions of 40min for 8 weeks, 3 mornings per week 5 weeks of washout Reading: 8 weeks | Behaviour problems (CMAI) Anxiety symptoms (RAID) | At baseline and after the first 8-week intervention period After the second 8-week intervention period | - Mean scores on the CMAI and RAID scales point to low levels of anxiety and minimal occurrences of aggressive behaviour (less than once per week) (P<.05; 95% CI) - The analysis did not show music therapy to be effective for improving agitation and anxiety in participants after 6 months |
CMAI: Cohen-Mansfield agitation inventory (physically non-aggressive behaviour, physically aggressive behaviour, verbally non-aggressive behaviour, and verbally aggressive behaviour); GSPM: group singing of preferred music; RCS: randomised crossover study; RCT: randomised controlled trial; GLNPM: group listening to non-preferred music; GLPM: group listening to preferred music; LPMI: listening to preferred music individually; PRT: pilot randomised trial; CG: control group; EG: experimental group; IG: interactive group; PG: passive group; min: minutes; MT: music therapy; NPI: neuropsychiatric index (hallucinations, delusions, depression, agitation, euphoria, anxiety, apathy, disinhibition, irritability, aberrant motor behaviour, appetite and eating change, sleep and night-time behaviour change).
Seven studies12–18 compare music therapy to a control intervention to treat behaviour disorders: 3 of them12–14 focus on agitation by comparing music therapy to the basic care provided to patients (2 of them focused on patients with AD)13,14; another article15 compares the group undergoing music therapy to a control group to determine its benefits on anxiety in adults with dementia; the other 3 articles, which do not compare therapies, describe the effects of music on behaviour disorders in general.16–18 The study by Sakamoto et al.19 distinguishes between active music therapy and passive music therapy. The passive group listened to music on a CD player and the active group participated in interactive activities (clapping, singing, and dancing), while control group individuals spent time with a carer in their own rooms.
One of the 11 selected studies compares the benefits of music therapy to those of physical activity with regard to behaviour disorders.20
Two authors propose crossover studies to study the benefits of music therapy vs reading21 and vs no therapy.22
Outcome measures in the selected studies are based on changes in behavioural disturbances, agitation, and anxiety.
Behaviour disordersFive studies compared the effects of music therapy on reducing behaviour problems with a control intervention or no intervention.16–20
In the study by Raglio et al.16, all patients received standard care, consisting of such educational and leisure activities as reading a newspaper or engaging in physical exercise. The music therapy group also received 3 cycles of music therapy sessions. Each cycle includes 12 sessions, 3 per week. Every cycle of treatment was followed by one month of washout. An improvement in general scores on the Neuropsychiatry Inventory (NPI) was observed in both the control group and the experimental group (P<.001), but with a large difference (P<.05) since the experimental group presented a more pronounced decrease in disturbances at the end of treatment (P<.001). Illusions, agitation, and apathy only improved in the experimental group, while depression, anxiety, and irritability improved in both groups. The experimental group did not show any improvement in aberrant motor behaviours, communication skills, or interpersonal ability. The final analysis shows that the main improvements in the experimental group manifest at the end of treatment, and remain during the follow-up stage (a month later).
The study by Suzuki et al.17 also provides data on the effects of long-term intervention. Here, 8 patients underwent 25 sessions of music therapy. Unlike in the previously mentioned study, improvements in certain behaviours measured on the Gottfries–Brane–Steen subscale, ‘symptoms common in dementia’, are not observed in the follow-up stage.
The experimental group does show a significant improvement in cognitive impairment (P<.05) one month after the intervention. The control group showed a decrease on the Mini–Mental State Examination (MMSE) score from 15.50 to 13.88 one month after the intervention.
The Gottfries–Brane–Steen scale focuses on the qualitative differences of dementia and is divided into several subscales. The assessment of the music therapy group using this scale shows that scores on the ‘symptoms common in dementia’ subscale improve significantly after the intervention (from 10.75 to 4.65); however, scores remain the same during the follow-up stage. There is a progressive decrease in scores in the control group.
The subscale ‘paranoid or delusional ideation’ of the scale Behaviour Pathology in Alzheimer's Disease (BEHAVE-AD), which assesses effects of medication on AD, shows improvement by the end of treatment (1.75–0.88); however, this score also decreased one month after the end of the intervention (0.52). In the control group, initial scores (0.88) increased once the intervention had finished (2.00) and again one month after that (2.75).
The study also shows cognitive changes according to the MMSE; the music therapy group obtained better scores at the end of the intervention and one month later. The control group's decreased score indicates impairment. Levels of chromogranin A (CgA) and secretory immunoglobulin A (IgA) were also recorded.
In the study by Choi et al.18, music therapy sessions consisted of singing songs, analysing lyrics, making and playing musical instruments, and drawing and writing songs. Each session lasted 50 minutes and 10 patients diagnosed with dementia participated. After 15 sessions, significant differences between the experimental group and the control group were found for agitation and aggressiveness, and in the total scores for severity and anxiety. The music therapy group improved in the areas of hallucination, aggressiveness/agitation, disinhibition, and irritability/lability (P<.05), while the control group did not show significant differences.
There were no intergroup differences in results on the MMSE. The music therapy group showed improved scores on both the Geriatric Depression Scale (GDS) and the Global Quality of Life Scale (GQoL).
Sakamoto et al.19 compared a music therapy group with a no-music group. In this case, interventions were divided into active and passive music therapy.
Scores on the Faces Scale (symptoms affecting emotions and stress level) indicate a lack of differences in the control group before and after the intervention (Z –1.9, P=.6). In contrast, patients in the passive group were significantly more comfortable in their surroundings after the intervention compared with before the intervention (P<.01); patients in the interactive group exhibited the greatest improvement in emotional state among the 3 groups (P<.01). The passive therapy group showed a reduction in affective disturbances (P<.025) and in anxiety and phobias, whereas the interactive group exhibited reductions in affective disturbances, anxiety and phobias, paranoid and delusional ideation, aggressiveness, and activity disturbances. In the control group, only activity disturbances and affective disturbances increased. Three weeks after the intervention, behavioural and psychological symptoms had increased in the passive and interactive groups, whereas no changes were observed in the control group.
The other study by Suzuki et al.20 compares music therapy to therapeutic physical activities (playing games, drawing, and pasting pictures) as treatment for behavioural problems. Using the Multidimensional Observation Scale for Elderly Subjects, they observed that scores for irritability (indicating patients’ degree of aggressiveness) decreased significantly (12.00–9.90, P=.0001) in the music therapy group; however, no changes were observed in the control group (P=.490).
Scores on the MMSE subscales ‘language’ and ‘attention and calculation’ improved in the music therapy group. Chromogramin A levels were also studied.
AgitationTo assess the effect of music therapy on agitation in patients with dementia, 3 of the studies used in this review article12–14 compare music therapy with no therapy, dividing participants into 2 groups (therapy group and control group).
The therapy group in the study by Lin et al.12 received music therapy in 12 group sessions during 6 weeks, and the control group continued with their normal daily activities. Four evaluations on the Cohen-Mansfield Agitation Inventory (CMAI) scale were performed, one before the intervention, 2 during the intervention (at the 6th and 12th sessions) and the last, one month after cessation of the intervention. The results show a significant decrease in scores for agitated behaviour in the experimental group for all 3 assessments after baseline: at the 6th session, the group score was 0.47 points less (P<.001), at the 12th session, 0.44 points less (P<.001), and post-intervention, 0.47 points less (P<.001). Physically aggressive and non-aggressive behaviours and verbally non-aggressive behaviours improved across all 3 assessments compared to the baseline evaluation. Verbally aggressive behaviours only showed improvement at the 6th session; better scores were not apparent at the 12th session or post-intervention. Data show lower CMAI scores in the experimental group than in the control group.
Unlike in the previous study, the results reported by Ledger and Baker13 seem to indicate that music therapy has an immediate effect only on agitated behaviours in patients with AD. They performed an assessment before the intervention and at months 3, 6, 9, and 12. There were no significant differences between the 2 groups in the range and frequency of agitated behaviours over time. Control groups showed a significant decrease on the baseline CMAI score at the first reassessment and a considerable increase at the following reassessment, followed by a decrease in agitation by the end of the study. The experimental group shows higher scores at baseline and the first CMAI reassessment, followed by a small decrease at the following reassessment.
There are no significant differences between the 2 groups regarding time of manifestation of any of the 4 agitation subtypes. The control group did not manifest a lesser level of non-aggressive behaviours. In the experimental group, agitation displayed a more stable course in the case of verbally aggressive behaviours than for other agitation subtypes.
The study by Zare et al.14 aims to determine how the type of music listened to or the activity performed might impact results of comparing music therapy to no interventions. Two measurements were made on the CMAI: one at the start of the intervention and another at one month once the intervention had ended.
Differences in post-intervention scores for agitation between the control group and the experimental group were statistically significant (P<.005). Differences between mean CMAI scores were also significant (P<.005). Differences between mean CMAI scores in the pretest and post-test periods are statistically significant for all 4 music therapy groups: the group listening to non-preferred music, the group singing preferred music, the group listening to preferred music on an individual basis, and the group listening to preferred music together. Although these data cannot be generalised, music therapy seems to have positive effects for reducing agitation.
In the study by Tuet et al.22, all participants received basic care and music therapy sessions. Participants were divided into 2 groups: one received music therapy sessions and the other received basic care only during 3 weeks; there was a washout period of 3 weeks and then both groups changed interventions. Three measurements were made to record any changes in agitation: one before starting sessions, one measurement a week after ending sessions, and the last one 3 weeks after ending treatment.
Significant differences were observed between previous and final NPI scores (P<.001) in the music therapy group. These differences were not observed at 3 weeks. The control group did not show any significant changes between initial and final overall NPI scores; in contrast, NPI scores significantly decreased immediately after the music therapy sessions.
CMAI scores at 3 weeks showed no significant differences with regard to the initial scores. There were no significant changes in the total CMAI scores at baseline and at 3 weeks in the 2 groups. However, there was a significant decrease in the final CMAI scores among patients who received music therapy.
AnxietyResults of the study by Sung et al.15 focused on the benefits of music therapy for anxiety in patients with dementia. The experimental group received music therapy sessions while the control group received basic care. Anxiety was measured using the Rating Anxiety in Dementia scale. After 6 weeks of listening to preferred types of music, the experimental group's mean score for anxiety decreased from 10.93 at baseline to 8.93 at the final evaluation. The control group showed no significant decreases. Data analysis indicates that participants who received music therapy sessions presented lower anxiety levels after cessation of interventions than did patients undergoing an intervention with no music.
Cooke et al.21 base their outcome measures on anxiety and agitation in patients with dementia. This study has a cross-over design: participants received music therapy and reading test sessions for 8 weeks, and after 5 weeks of washout, they changed activities.
The CMAI and the Rating Anxiety in Dementia scores indicate low levels of anxiety and minimal levels of aggressive behaviours. In both groups, sessions were held at least once a week. Three control measurements were taken and revealed low scores for all 4 agitation subtypes. Researchers observed low levels of anxiety and agitation in patients, but music therapy was not observed to have an overall effect on improving agitation and anxiety at 6 months.
Assessment of methodological qualityRegarding methodological quality, we determined whether or not studies met the 11 quality criteria (‘yes’ or ‘no’ answers), as listed in Table 2. A ‘no’ answer does not necessarily mean that the study lacks the indicated characteristic; it could also mean that the text does not mention that characteristic.
Methodological quality of included studies.
| Article | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | Score |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yu Lin et al.12 (2011) | Y | Y | N | Y | N | N | N | Y | N | Y | Y | 5 |
| Ledger et al.13 (2007) | Y | Y | N | Y | N | N | N | N | N | Y | Y | 4 |
| Zare et al.14 (2010) | Y | N | N | N | N | N | N | N | N | Y | Y | 2 |
| Huei-Chuang et al.15 (2010) | Y | Y | N | Y | N | N | N | Y | N | Y | Y | 5 |
| Raglio et al.16 (2010) | Y | Y | N | Y | N | N | Y | Y | N | Y | Y | 6 |
| Suzuki et al.17 (2007) | N | N | N | Y | N | N | Y | Y | Y | Y | Y | 6 |
| Ae-Na Choi et al.18 (2009) | Y | N | N | Y | N | N | N | Y | Y | Y | Y | 5 |
| Sakamoto et al.19 (2013) | Y | Y | Y | Y | N | N | Y | Y | Y | Y | Y | 8 |
| Suzuki et al.20 (2004) | N | N | N | Y | N | N | Y | N | N | Y | Y | 4 |
| Cooke et al.21 (2010) | Y | Y | Y | Y | N | N | Y | Y | N | Y | Y | 7 |
| Tuet et al.22 (2006) | Y | N | N | Y | N | N | N | Y | N | Y | Y | 4 |
N: criterion not present; Y: criterion present; 1. eligibility criteria; 2. random allocation; 3. concealed allocation; 4. baseline similarity: groups were similar at the beginning with regard to the main prognostic indicators; 5. blinding of subjects; 6. blinding of therapists; 7. blinding of assessors; 8. follow-up of subjects (at least 85% of them); 9. intention to treat analysis; 10. inter-group statistical comparisons; 11. point measures and measures of variability.
One of the studies by Zare et al.14 obtained an overall score of 2 (low). The highest scores were assigned to the studies by Sakamoto et al.19 and Cooke et al.21, which were 7 and 8 respectively (good). The remaining studies obtained scores of 4, 5, and 6 (Table 2).
All studies met criteria number 10 (intergroup statistical comparisons) and 11 (point measures and measures of variability); none of the studies met criteria number 5 (‘blinded’ patient), and 6 (‘blinded’ therapist).
DiscussionAlthough many studies have been conducted to assess treatment effectiveness in elderly patients with dementia, published studies assessing the benefits of music therapy as a non-pharmacological treatment for elderly patients with dementia are limited. According to results from this review, only a low number of clinical trials and controlled trials have attempted to analyse the effects of music therapy on behaviour problems present in dementia patients.
If results from a study are to be extrapolated to the general population, the sample must be large and representative. In the different studies included in this review,15,19 the sample was very limited (n=8, n=10, n=16); therefore, results obtained with these interventions cannot be extrapolated to the whole population of patients with dementia.
Changes in conduct take some time to manifest. Most of the studies in this review article12,14,15,17,18,20–22 include interventions held for a very short period (3–8 weeks) and low numbers of sessions (9–12); therefore, the changes observed may not be very significant.
The limitation we encountered, and which made completing this review more challenging, is the scarcity of scientific articles addressing the benefits of music therapy as a non-pharmacological alternative for treating behaviour. The results of the study focus on the long-term changes assessed before and after the intervention, but studies do not include reassessments beyond one month after the intervention.
If we consider the internationally recognised models in the 9th World Congress of Music Therapy (1999), none of the studies in this review mentions the music therapy models used in their interventions. Five of the studies12,18,20–22 use active techniques of music therapy (singing, playing instruments, drawing, etc.), and 3 of them based their activities on passive listening to music.14,15,19 Several studies also use 2 combined techniques during a single session.13,16,17
The definition of music therapy specifies that sessions must be guided by a qualified music therapist; however, we have found studies in our review in which music activities were directed by musicians17,21 or occupational therapists.22 In other studies including listening sessions, music was provided by nurses and therefore cannot be considered music therapy in a strict sense.14
We should highlight that 7 of the 11 selected studies12,15,17–20,22 were conducted by Asian researchers, which means that the tools used in the interventions (songs, instruments, etc.) belong to Eastern culture; therefore, data from these studies cannot be extrapolated to the whole population due to cultural differences.
Conclusions expressed in this article have been drawn based on the studies delivered by our search and the inclusion and exclusion criteria that were applied. Nevertheless, we must consider the possibility that some studies may have not been included in this review due to the restrictiveness of our search criteria.
ConclusionOver the past few years, few controlled trials and randomised controlled trials have addressed music therapy as a technique used for treating behaviour problems in patients with dementia.
Results from this review article suggest that music therapy is beneficial for improving behaviour problems, anxiety, and agitation in patients with dementia.
However, due to the limited number of patients included in the studies and the low numbers of studies, further research in this field will be needed to improve quality of life in the elderly.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Gómez-Romero M, Jiménez-Palomares M, Rodríguez-Mansilla J, Flores-Nieto A, Garrido-Ardila EM, González-López-Arza MV. Beneficios de la musicoterapia en las alteraciones conductuales de la demencia. Revisión sistemática. Neurología. 2017;32:253–263.