Intracranial aneurysms are a health problem affecting 5% of the general population. However, the frequency of ruptured aneurysms is much lower. Therefore, most aneurysms are asymptomatic or give rise to symptoms by means of other mechanisms, especially compression of adjacent structures.1,2
These lesions most commonly affect the anterior part of the circle of Willis, an area which is closely connected to the visual pathways. Aneurysms that are located in the supraclinoid region may cause progressive loss of visual acuity which is occasionally associated with ophthalmoplegia due to compression of the visual pathway or oculomotor nerves.2–5
We present the case of a patient with bilateral carotid aneurysm and progressive loss of visual acuity.
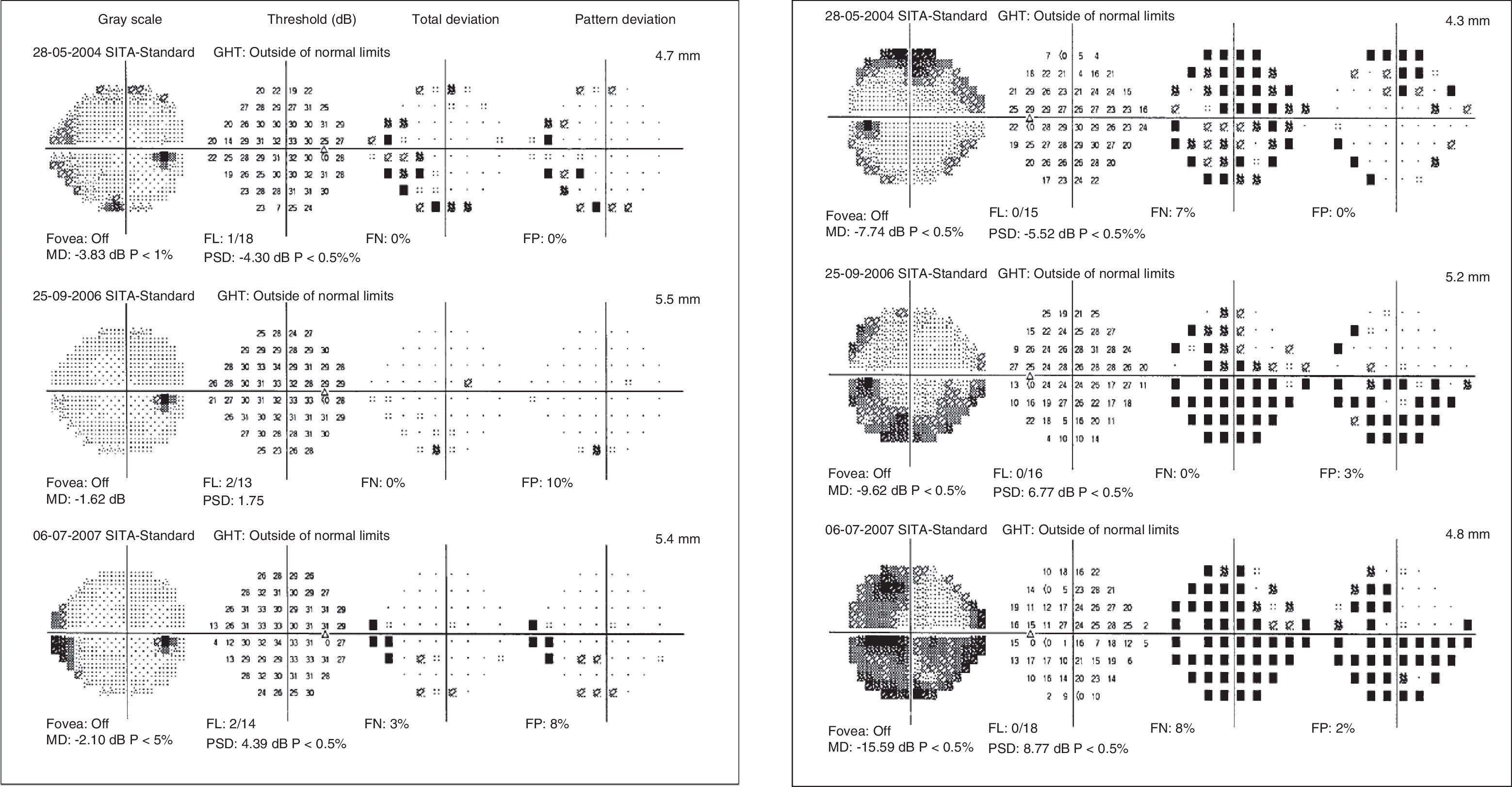
Our patient was a 49-year-old female with no relevant medical history who was referred to our neurology department. She had been experiencing slow, progressive impairment of visual acuity over the previous 5 years (Fig. 1). A few weeks before the scheduled consultation, the patient also presented right retro-orbital pain. The patient was initially diagnosed with glaucoma and treated with prostaglandin analogues.
Examination revealed bilateral papillary pallor and decreased visual acuity (RE: 0.8; LE: 0.5), and no evidence of oculomotor involvement or facial hypoaesthesia.
We performed a complete analytical study including haemogram, biochemical analysis, coagulation study, vitamins and folic acid, thyroid function, and immunology tests. Results were negative or normal. We also performed a visual evoked potential test revealing severe bilateral visual impairment at all locations in the left eye and the peripheral region of the right eye, and a genetic study which was negative for Leber optic atrophy.
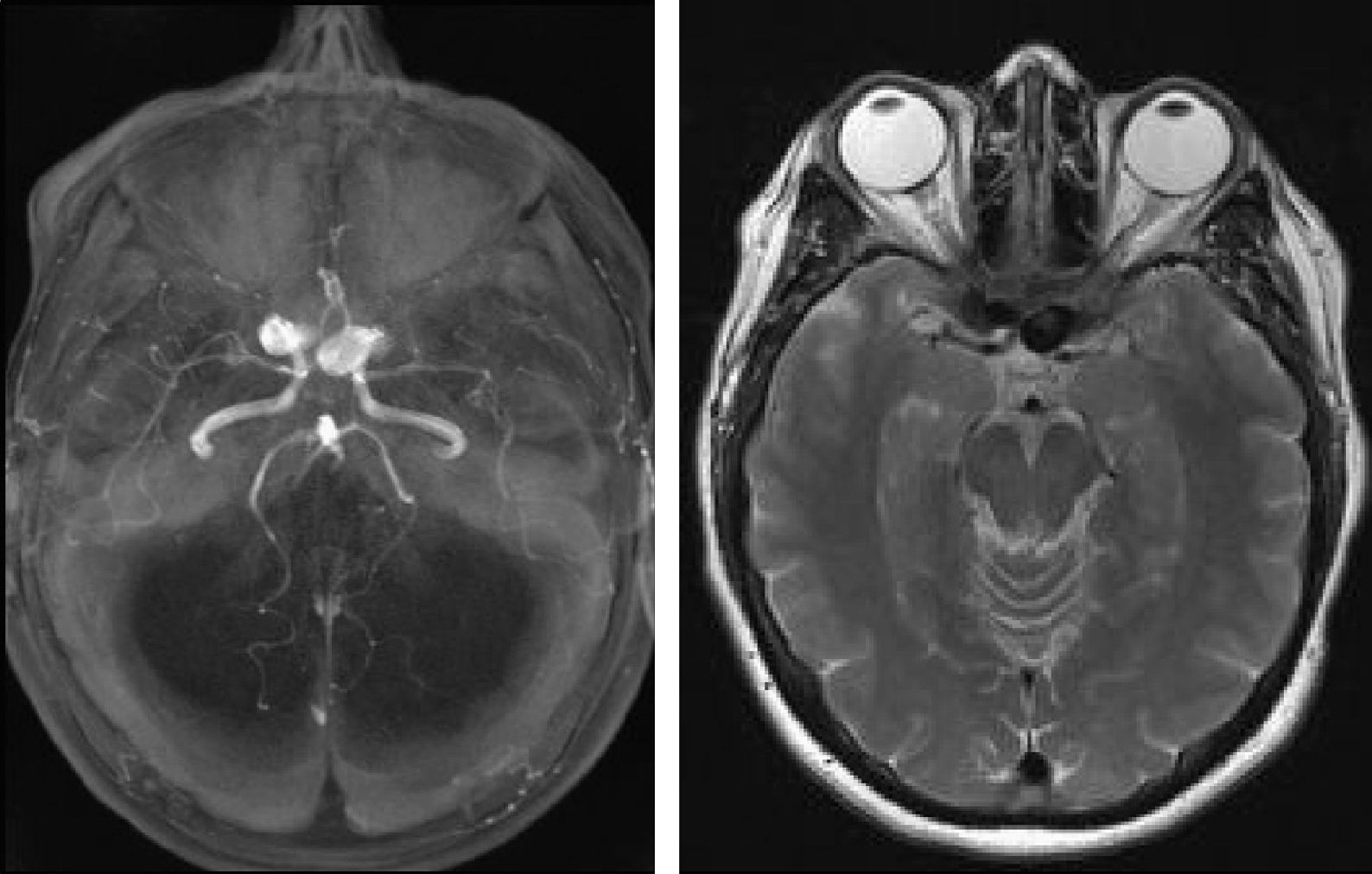
Brain MRI showed dilation of the carotid arteries in the supraclinoid segment with compression of the optic nerves. MR angiography confirmed the presence of bilateral aneurysms. Cerebral arteriography revealed the location of these aneurysms at the emergence of the right ophthalmic artery (approximate size: 16mm×12mm, neck 8.38mm) and the left ophthalmic artery (approximate size: 17mm, neck 12mm) (Fig. 2).
Supraclinoid aneurysms of the carotid artery are a potentially treatable cause of progressive visual impairment. Approximately 10% of these aneurysms present neurological signs associated with a mass effect, such as headache, ophthalmoparesis, and the visual impairment mentioned here.
Examination of the visual pathways is very important in the diagnosis of neurological illnesses. Although it is infrequent, intracranial compression of the optic nerve by a carotid artery should be considered when performing differential diagnosis of a patient with progressive or unexplained unilateral or bilateral optic neuropathy.4,6
MRI is the diagnostic method of choice for those patients who are suspected of having visual pathway compression, especially around the optic chiasm.7