Brain death is generally accepted as a concept to indicate death. It was introduced about 40 years ago, and it was considered the ideal situation for donation of organs.
Material and methodsDuring this time, however, there have been problems in the understanding of this concept both in the medical profession and in the general population. University students from medical and non-medical schools were tested for their understanding of this concept.
ResultsOur results show that less than one third of the non-medical students identified brain death as death. The data from the medical students changed as they progressed through their studies, but only 2/3 of the graduating medical class believed that brain death is death.
ConclusionSimilar results have been seen in other universities around the world, and a renewed effort on the re-education of the concept of brain death may be worthwhile. Although we cannot extrapolate these results to the general population, the confusion is probably similar; hence an effort should be made to solve this problem.
“Muerte cerebral” es un término generalmente aceptado para indicar la muerte. Fue introducido hace más de 40 años, y, desde entonces, se considera la situación ideal para la donación de órganos. Sin embargo, existen serios problemas con respecto a la comprensión de este concepto, tanto en profesionales médicos como en la población general.
MétodosSe realizó una encuesta a estudiantes universitarios de facultades médicas y no médicas para comprobar la interpretación del concepto de muerte cerebral.
ResultadosMenos de un tercio de los estudiantes no médicos identificaron claramente muerte cerebral con muerte. Los datos en estudiantes de Medicina diferían a medida que los cursos eran más avanzados, pero sólo dos tercios de los alumnos de último curso de Medicina pensaban que la muerte cerebral equivalía a muerte. Resultados similares se han encontrado en universidades de otros países, siendo necesario un mayor esfuerzo en la docencia del concepto de muerte cerebral.
ConclusionesLos resultados de este trabajo muestran la confusión existente entre universitarios a la hora de interpretar el término “muerte cerebral”; aunque esta confusión no es extrapolable a la población general es probable que la confusión en la población no sea menor. Por ello, dada la importancia del tema, deberían plantearse soluciones para resolver esta confusión, bien explicando mejor el término o modificando la terminología.
“Brain death” is a term used to indicate death according to neurological criteria, even when the heart and other organs continue with their physiological function. It has traditionally been considered that “brain death” is synonymous with death, although for some people there would be an intermediate concept called “irreversible coma”, which in turn could also be synonymous with definitive death.1–3 At present, the term “brain death” has been accepted by the medical community as a synonym for death,4–6 although, as mentioned, there has been and currently still is criticism in this respect.7–11 In fact, other terms have been proposed, such as “total brain failure” or “global brain failure”.12 In a state of brain death, organs can continue to function for hours or days, allowing the transplantation of organs.
In Spain, the Royal Decree of January 2000 on the collection and use of organs and their use in transplantation refers to brain death as a state of death secondary to processes that primarily cause complete and irreversible damage of brain functions.13 This Royal Decree specifies that ‘the diagnosis and certification of death will be based on the irreversible cessation of cardiopulmonary functions or brain functions, as established in Article 10’; and this Article 10, entitled ‘Removal of organs from deceased persons: conditions and requirements’, explains the death criteria to confirm the irreversibility and complete cessation of either cardiopulmonary or brain functions. Annex 1 shows the diagnostic protocols of death, whether death by cardiac arrest or death by cessation of brain functions (brain death).
While it is true that the concept of brain death has generally been accepted by neurologists, there are some authors who differ in this respect.14,15 In general, the majority accept the term “brain death” (including the fact that it is definitive and there is a dysfunction of the brainstem), but it is clear that the disagreement exists and not all doctors share the same opinion.16–18 In contrast, the situation in other areas of sociology, including the media, is striking. Even in hospitals, physicians and nurses sometimes feel uncomfortable explaining to families the concept of brain death, although it is true that most, about 80%, are comfortable in handling the concept.8,19,20 Students at some medical schools were asked about this subject.14,15,21,22 The findings were striking, since a large proportion of the students believed that brain dead patients were in a coma or vegetative state. As a result, the authors of these studies have suggested that universities should take strong measures to improve the teaching and understanding of these terms.
Among the general population the use and understanding of this term is even worse. It is not unusual to hear in the media that “a person is brain dead” and several days or weeks later to hear them announce that that same person has died.11
Given such background, the objectives of this study were to show whether there is confusion among university students about brain death, and investigate whether teaching in medical schools could influence the concept of “brain death” held by students.
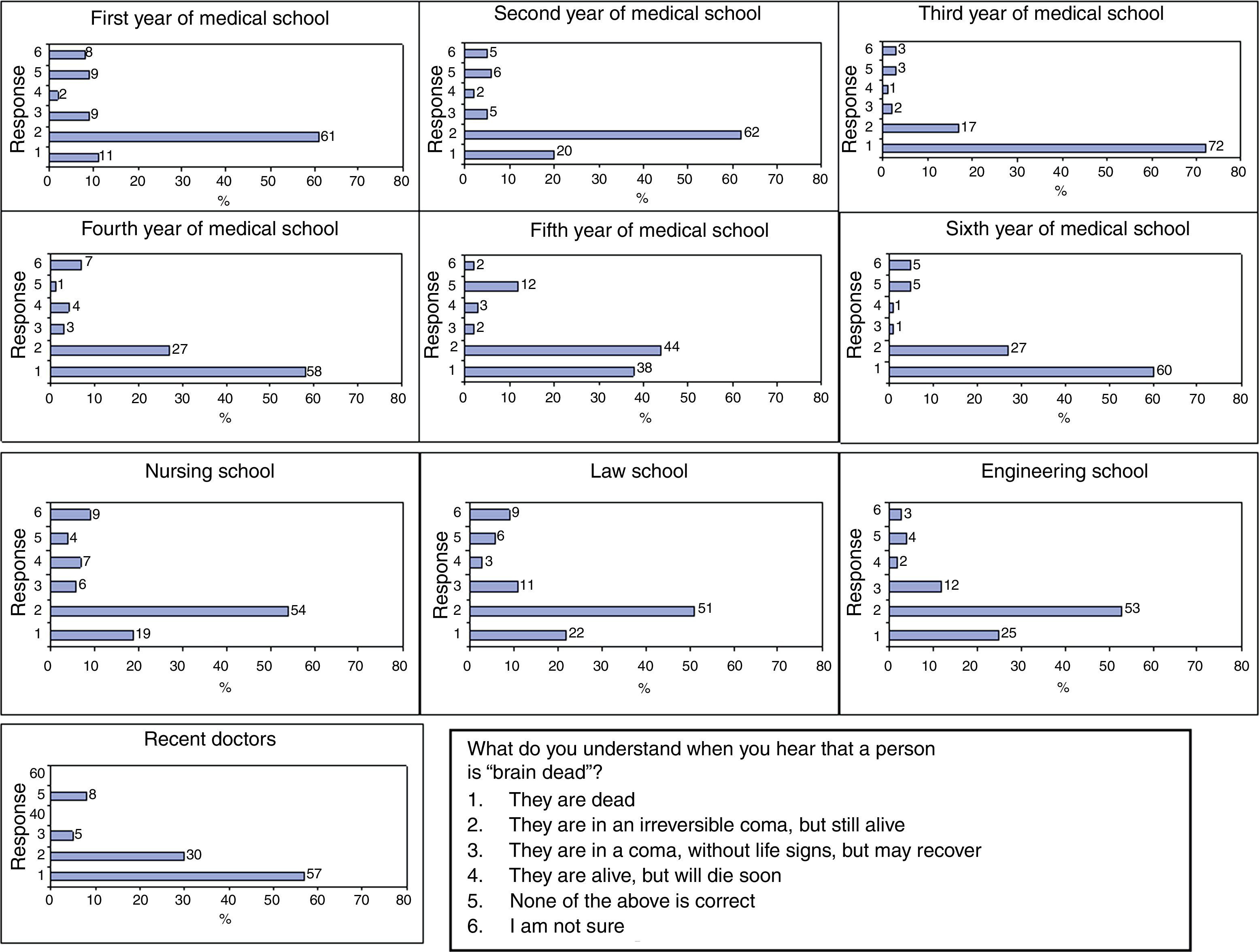
Material and methodsThe study consisted of an online survey for students in all courses from the schools of Engineering, Law and Journalism at the University of Navarra, students in their 2nd and 3rd years of Nursing school and from each of the 6 courses of Medicine, in addition to graduates from the previous June. The survey included a question about the meaning of “brain death” with 6 possible answers regarding brain death (Fig. 1). Upon responding, students were identified in the database as members of the corresponding school and, in the case of Medicine, their year was also recorded.
Question about brain death and possible answers. Responses among the different groups and students are shown in percentages. Medical students in their 1st and 2nd years responded similarly to students from other schools. However, the responses of the remaining medical students and recent graduates were discordant.
This survey was carried out via the University Intranet, with the ADI software application, with which all student information is managed. This application enables surveys of large groups of students to be conducted. It is possible to generate a survey and then the target students receive an email informing them that they have to answer it. The survey was active for two weeks, after which the study was closed. The study was conducted one month after the beginning of the academic year, in mid-October.
For the analysis of results, we considered comparing students by schools, except in the case of Medicine, where students were divided into groups that included students in each year (6 courses, as well as graduates from the previous year). We analysed frequency data from each of the answers, in absolute terms and in proportion, and carried out a comparison of results using the chi-square statistical test with the absolute values of the response “dead” compared to all other possibilities.
ResultsDescriptive results in non-medical schoolsOnly 7 students from the school of Journalism answered the questions, so they were excluded from this study. On the other hand, 103 Law students and 170 Engineering students answered the question. It is noteworthy that the 1st day after receiving the email, 130 engineering students (and only 1 from Law) had responded to the study.
The results are shown in Fig. 1. Up to 19% and 22% of students in Engineering and Law respectively believed that a brain dead patient was truly dead. Instead, 54% and 51% believed that the patient was “in a reversible coma, but alive”. About 15% of students thought that all answers were incorrect or had doubts about selecting a response. About 60% of non-medical students thought that a brain dead patient was not completely dead and only 20% knew that the patient was truly dead.
Descriptive results in Nursing schoolThe question was posed only to students in the 2nd and 3rd years of Nursing school who had already received some medical training and had completed some hospital training. A total of 85 students answered the question. Of these, 25% thought that a brain dead patient was really dead, 4% thought that all the answers were incorrect and 3% had doubts. In total, 67% of Nursing students believed that a brain dead patient was in a coma and still alive.
Descriptive results in medical schoolA total of 64 students in their 1st year, 64 in their 2nd year, 86 in their 3rd year, 74 in their 4th year, 64 in their 5th year, 78 in their 6th year and 40 doctors who had graduated the previous year and were preparing their internship exams responded to the survey.
The percentage of medical students who responded that the patient was truly dead had its peak in the 3rd year (72%) and gradually fell in the 4th year (58%) and 5th year (38%). A further increase was observed with students in their 6th year (60%). Out of the doctors who had graduated the previous year, 57% believed that a brain dead patient was truly dead.
These results confirm that 1st year medical students, after one year of basic courses, had the same idea of brain death as other university students from other non-medical disciplines. The greatest difference between students from medical and non-medical degrees was observed with 3rd year medical students (72% versus 20%).
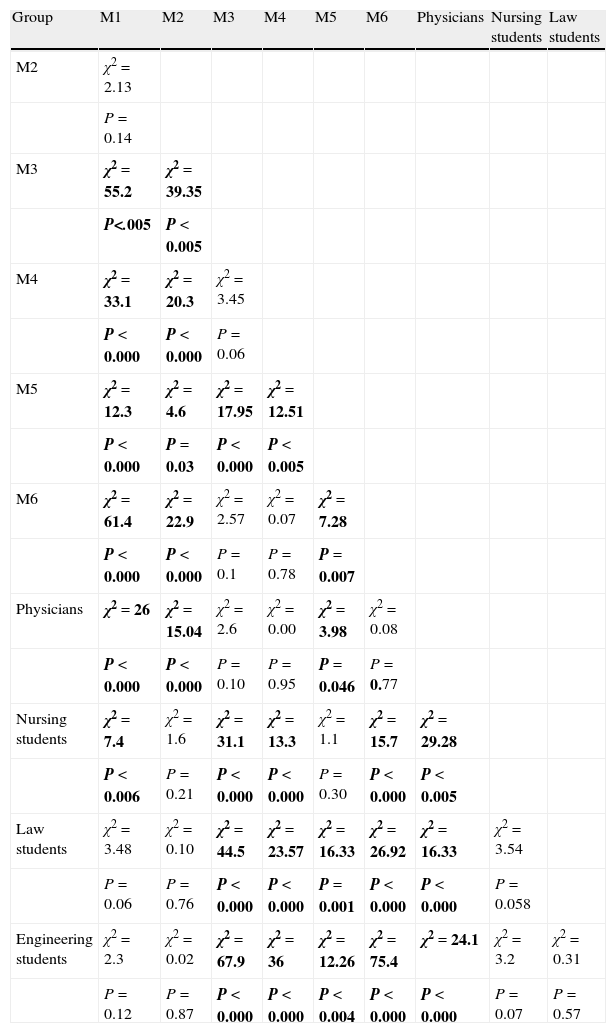
Statistical analysis of resultsThe chi-square analysis for comparison of the response “brain dead patients are truly dead against other options” made with all groups showed several significant differences. The full results of the results between each 2 groups with the corresponding Chi-square (χ2) and P values for statistical significance are shown in Table 1.
Results of the comparison of the frequency of the response “brain death is equal to death”, comparing each group of students with all the others using the Chi-square test.
| Group | M1 | M2 | M3 | M4 | M5 | M6 | Physicians | Nursing students | Law students |
| M2 | χ2=2.13 | ||||||||
| P=0.14 | |||||||||
| M3 | χ2=55.2 | χ2=39.35 | |||||||
| P<.005 | P<0.005 | ||||||||
| M4 | χ2=33.1 | χ2=20.3 | χ2=3.45 | ||||||
| P<0.000 | P<0.000 | P=0.06 | |||||||
| M5 | χ2=12.3 | χ2=4.6 | χ2=17.95 | χ2=12.51 | |||||
| P<0.000 | P=0.03 | P<0.000 | P<0.005 | ||||||
| M6 | χ2=61.4 | χ2=22.9 | χ2=2.57 | χ2=0.07 | χ2=7.28 | ||||
| P<0.000 | P<0.000 | P=0.1 | P=0.78 | P=0.007 | |||||
| Physicians | χ2=26 | χ2=15.04 | χ2=2.6 | χ2=0.00 | χ2=3.98 | χ2=0.08 | |||
| P<0.000 | P<0.000 | P=0.10 | P=0.95 | P=0.046 | P=0.77 | ||||
| Nursing students | χ2=7.4 | χ2=1.6 | χ2=31.1 | χ2=13.3 | χ2=1.1 | χ2=15.7 | χ2=29.28 | ||
| P<0.006 | P=0.21 | P<0.000 | P<0.000 | P=0.30 | P<0.000 | P<0.005 | |||
| Law students | χ2=3.48 | χ2=0.10 | χ2=44.5 | χ2=23.57 | χ2=16.33 | χ2=26.92 | χ2=16.33 | χ2=3.54 | |
| P=0.06 | P=0.76 | P<0.000 | P<0.000 | P=0.001 | P<0.000 | P<0.000 | P=0.058 | ||
| Engineering students | χ2=2.3 | χ2=0.02 | χ2=67.9 | χ2=36 | χ2=12.26 | χ2=75.4 | χ2=24.1 | χ2=3.2 | χ2=0.31 |
| P=0.12 | P=0.87 | P<0.000 | P<0.000 | P<0.004 | P<0.000 | P<0.000 | P=0.07 | P=0.57 |
Comparisons with statistically significant differences in chi-square and P values are shown in bold. M1: 1st Medicine students; M2: 2nd year Medicine students; M3: 3rd year Medicine students; M4: 4th year Medicine students; M5: 5th year Medicine students; M6: 6th year Medicine students.
As shown in the table, numerous significant differences were found among students according to their schools and years. Students in the 3rd, 4th and 6th years of Medicine, as well as graduates from the previous year, predominantly responded that the patient was dead. In contrast, students in the 1st, 2nd and 5th years of Medicine responded the opposite. For most of them, as well as for Law and Engineering students, it was less frequent to respond that the patient was dead. Nursing students, in their 2nd and 3rd years, responded in an intermediate manner. The percentage of students who said that brain death was equivalent to death increased, but without reaching the values of Medicine students in higher courses. Particularly striking is the response of 5th year Medicine students, who behaved as non-medical students, responding more frequently than the patient was dead.
DiscussionThe use of the term “brain death” as a criterion to define death was introduced over 40 years ago in the field of Neurology.1,23 It has been widely accepted and only a few authors have problems with its use.4,24 In Spain it was accepted and published as such in the Official State Bulletin (BOE).13 Errors have probably arisen from an improper use of neurological criteria for determining brain death, if anything more pronounced in cases involving children.25 In medical terms, brain death is considered a synonym for death. For this reason, brain dead patients with intact cardiac function and artificial respiration are candidates for organ transplant without any ethical objections; the patients are already dead and therefore cannot be damaged by extracting their organs for transplantation.
Our objective was to test whether a sample of university students properly understood the concept of brain death or had doubts about it. We did not intend to extrapolate the results to the general population, even to other university populations, but we do believe that we could obtain an idea of the confusion over this term.
The results are clear. With a sample of over 800 students, we believe the figure is significant, and that the results may indirectly reflect a problem that probably exists among the general population. Our main conclusion is that after high school and during non-medical university studies, the percentage of individuals who do not correctly interpret the term “brain death” can be high, given that it exceeds 70% of the sample in our groups. We suspect that this figure would be lower in population groups of different ages or environments, although confirming this would require a larger study, which exceeds the scope of this work.
The situation in Nursing school was quite similar but not identical to that of non-medical schools, which could be explained on the grounds that the concept of brain death is not adequately explained in any subject during the 1st and 2nd years of Nursing. Our study also highlighted the confusion among Medicine students; this confusion varied throughout the 6 years of the degree. In fact, there was a significant change after the 2nd year, probably due to the subjects whose syllabus includes anatomy and physiology of the nervous system, taught in the 2nd year. In the following years, neurophysiology is not studied again, so the percentage of students who interpreted the term “brain death” correctly decreased and, surprisingly, the results of 5th year Medicine students were similar to those of 2nd year Medicine or Nursing students. In the last year of Medicine, this percentage increased to only 60%. Recent studies conducted at other Medicine schools have found results similar to ours.14,15,21,26 These studies also included additional questions about the vegetative state or about clinical data in brain death, as well as questions about definitive death and brain death.
A study conducted in Japan showed that only 46% of medical students and 39% of non-medical students accepted brain death as death and that 71% and 57%, respectively, would accept transplanted organs extracted from brain-dead donors.26
The withdrawal of life support systems is another fact illustrating the existing conflict: if patients themselves were surveyed, 63.7% would remove the support; if the patient were a relative, 46.8% would remove it; 52.4% of students would withdraw artificial respiration if the patient were not related to them.21 The authors of this study mentioned their surprise at the poor understanding of brain death among medical students and recommended taking urgent measures to prevent such confusion.21
These results were consistent with other studies conducted among the general population to address the issue of organ donation.19,27,28 Similarly, our results in the group of recent medical graduates were compatible with the fact that only 20% of physicians and nurses working in the environment of intensive care units (ICUs) reported feeling “uncomfortable” with the situation of brain death and organ transplantation.8 In other studies, the results were striking, in the sense that a high percentage of respondents (58% of physicians and nurses) used the concept of death incorrectly.29
Our own impression is that it is difficult to eradicate this confusion (some people believe that the patient is dead while others do not) if the term continues to be used. A solution proposed by other neurologists is the use of the terms “brainstem death”, “total brain death” or “encephalic death”,30 although there are no studies that confirm the suitability of such proposals. During the preparation of the Harvard Declaration on brain death in 1968,4 Dr. Murray manifested: ‘the term “brain death” should be eliminated. We are talking about death, and adding the word “brain” implies some restriction on the term as if it were an incomplete death’. The final position of the Declaration was to accept the redefinition of death, but the terms “brain death” and “irreversible coma” were finally used as synonyms in the definitive statement.
Our intention with this article is only to draw attention to the existing confusion. We believe that these data are probably not isolated; instead, this confusion will surely exist to a greater or lesser extent among the general population. Some studies should be conducted on how to convey this concept adequately to the general population and, even more so, to medical staff given that, as in other countries, there is still some confusion on the topic and the consequences are of great importance.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Iriarte J, et al. Muerte cerebral: ¿es un término adecuado? Neurología. 2011;27:16–21.