Our conception of the mind-brain relationship has evolved from the traditional idea of dualism to current evidence that mental functions result from brain activity. This paradigm shift, combined with recent advances in neuroimaging, has led to a novel definition of brain functioning in terms of structural and functional connectivity. The purpose of this literature review is to describe the relationship between connectivity, brain lesions, cerebral plasticity, and functional recovery.
DevelopmentAssuming that brain function results from the organisation of the entire brain in networks, brain dysfunction would be a consequence of altered brain network connectivity. According to this approach, cognitive and behavioural impairment following brain damage result from disrupted functional organisation of brain networks. However, the dynamic and versatile nature of these circuits makes recovering brain function possible. Cerebral plasticity allows for functional reorganisation leading to recovery, whether spontaneous or resulting from cognitive therapy, after brain disease.
ConclusionsCurrent knowledge of brain connectivity and cerebral plasticity provides new insights into normal brain functioning, the mechanisms of brain damage, and functional recovery, which in turn serve as the foundations of cognitive therapy.
La relación entre mente y cerebro ha evolucionado desde el clásico dualismo hasta los conocimientos actuales que ponen de manifiesto que las funciones mentales son el resultado de la actividad cerebral. Este cambio de paradigma, junto con los recientes avances en diferentes técnicas de neuroimagen, ha dado lugar a una novedosa concepción del funcionamiento cerebral en términos de conectividad estructural y funcional. El objetivo del presente trabajo es describir la relación entre conectividad, lesión cerebral, plasticidad cerebral y recuperación funcional.
DesarrolloSi la función cerebral surge de la organización en red del cerebro como un todo, la disfunción cerebral se puede producir por una alteración en la conexión de estas redes. Así, a partir del modelo conectivista, los trastornos cognitivos y del comportamiento que aparecen tras una afección cerebral se describen como consecuencia de una alteración en la organización funcional de las redes cerebrales. Sin embargo, la pérdida de funciones puede ser recuperada gracias a la capacidad de los circuitos de ser dinámicos y versátiles. La plasticidad cerebral permite una reorganización funcional que llevará a una recuperación, espontánea o potenciada con terapia cognitiva, después de algún tipo de enfermedad cerebral.
ConclusionesEl conocimiento de la conectividad y la plasticidad cerebrales proporciona una nueva perspectiva desde la que entender el funcionamiento cerebral en condiciones normales, los mecanismos del daño cerebral y los de la recuperación funcional, constituyendo las bases para el desarrollo de la terapia cognitiva.
For many years, mind and brain were regarded as distinct entities. This dualism, most famously defended by René Descartes in the 17th century, has long been a cornerstone of Western culture. Technology and the development of neuroscience as a discipline have since led to the emergence of a new conception of mind as the result of processes occurring in the brain. This new premise requires us to discover how the brain must work to produce such a complex system as the “mind”: as has previously been stated, “there can be brain without mind, but there can be no mind without brain” (E. Díez-Tejedor). Localisationist theories argued that each part of the brain is responsible for a specific function; according to this view, a localised brain lesion would selectively damage certain cognitive processes. However, these brain maps exclude many functions that have classically been attributed to the concept of mind: behaviour, personality, mood, and affect, among others. Although evidence already existed that specific brain injuries could cause behavioural alterations, it was the famous case of Phineas Gage in the mid-19th century that led to investigation into the biological basis of such mental processes as emotion management or decision-making.1 Moving beyond the localisationist approach, the brain was understood to function by means of complex, interconnected circuits involving both the cerebral cortex and the white matter.
However, it has long been known that the brain is able to modify itself in response to certain stimuli. Ramón y Cajal's assertion that “any man could, if he were so inclined, be the sculptor of his own brain” was without doubt a reference to brain plasticity. Nonetheless, several decades passed before the discovery would be made that the brain not only has this capability, but is also able to form new nerve cells; Cajal doubted this in his day.
This article reviews several aspects of brain disease and how it is related with connectivity and plasticity, as well as the fundamental aspects of cognitive therapy techniques based on these functions.
Connectivity and brain diseaseThe human brain is a complex network of structurally and functionally interconnected regions; brain function arises from the networked organisation of the organ as a whole. Brain lesions can therefore cause functional deficits by means of 2 basic mechanisms: local cortical dysfunction in the affected region, and spatially separate dysfunction caused by interruption of the connection between 2 areas.
Research into the circuits and networks constituting the highly complex organisation of the brain allows us greater insight into the structuring of the higher cognitive functions and their involvement in various neurological diseases. Indeed, we now know that the deficits associated with such disorders as Alzheimer disease, multiple sclerosis, traumatic brain injury (TBI), schizophrenia, depression, autism, etc., are accompanied by brain connectivity alterations.
In Alzheimer disease, we observe reduced density of dendritic spines in cortical pyramidal cells and structural alterations to inhibitory circuits; this leads to a disconnection between different regions of the brain, such as the posterior cingulate and the hippocampus. These changes can be detected in the prodromal stage of the disease, and are correlated with the degree of cognitive impairment in later stages.2 The progression of neurodegeneration is accompanied by reduced connectivity of the default mode network caused by deposition of β-amyloid peptide3; due to this, reduced connectivity has been found even in patients with mild cognitive impairment, compared to controls.4
Both cognitive deficits and emotional and behavioural alterations have been associated with the interruption of brain networks in patients with multiple sclerosis5,6; functional neuroimaging studies have also demonstrated alterations in brain activation and functional connectivity patterns.7,8 More recently, the introduction of graph theory has revealed structural changes in network topology in these patients, with modifications in the architecture of “small-world” networks9 impairing the efficiency of information transmission, leading to significant reductions in network efficiency.10
Another disease shown to involve a connection disorder is schizophrenia, which features an underlying alteration of the functional connections between different brain regions.11,12 The disease involves a disruption in the connection between different nodes of the default mode network, specifically the medial frontal cortex and the precuneus, which are key areas of the network,13,14 and frontoparietal and fronto-striato-temporal circuitry.15,16
Altered synchronisation has also been described in various brain networks in patients with autism spectrum disorders. In a study including patients with autism, Just et al.17 found reduced functional connectivity between different brain areas (underconnectivity) during a sentence comprehension task. This has been confirmed by several functional magnetic resonance imaging (fMRI) studies.18–20 However, other studies have also found evidence of this functional connectivity alteration in patients with autism who were at rest.21–24
Traumatic brain injury also involves the interruption of brain networks, which causes considerable cognitive and behavioural disorders. The diffuse axonal damage caused by such a lesion affects white matter tracts connecting the nodes of widely distributed neural networks.25 The most studied examples are the default mode network and the salience network; abnormal interaction between the 2 has been observed following TBI.26,27 Specifically, the functioning of the default mode network appears to be predicted by the degree of damage to the salience network which connects the right anterior insula, the presupplementary motor area, and the dorsal anterior cingulate cortex. These findings support the hypothesis that salience network integrity is necessary for the efficient functioning of the default mode network, and that a failure of communication between the networks can lead to disorders of inhibitory control.28
This new connectivity-based approach brings new ways of understanding the mechanisms underlying the deficits that appear following brain injury and the changes to connectivity that occur during recovery.
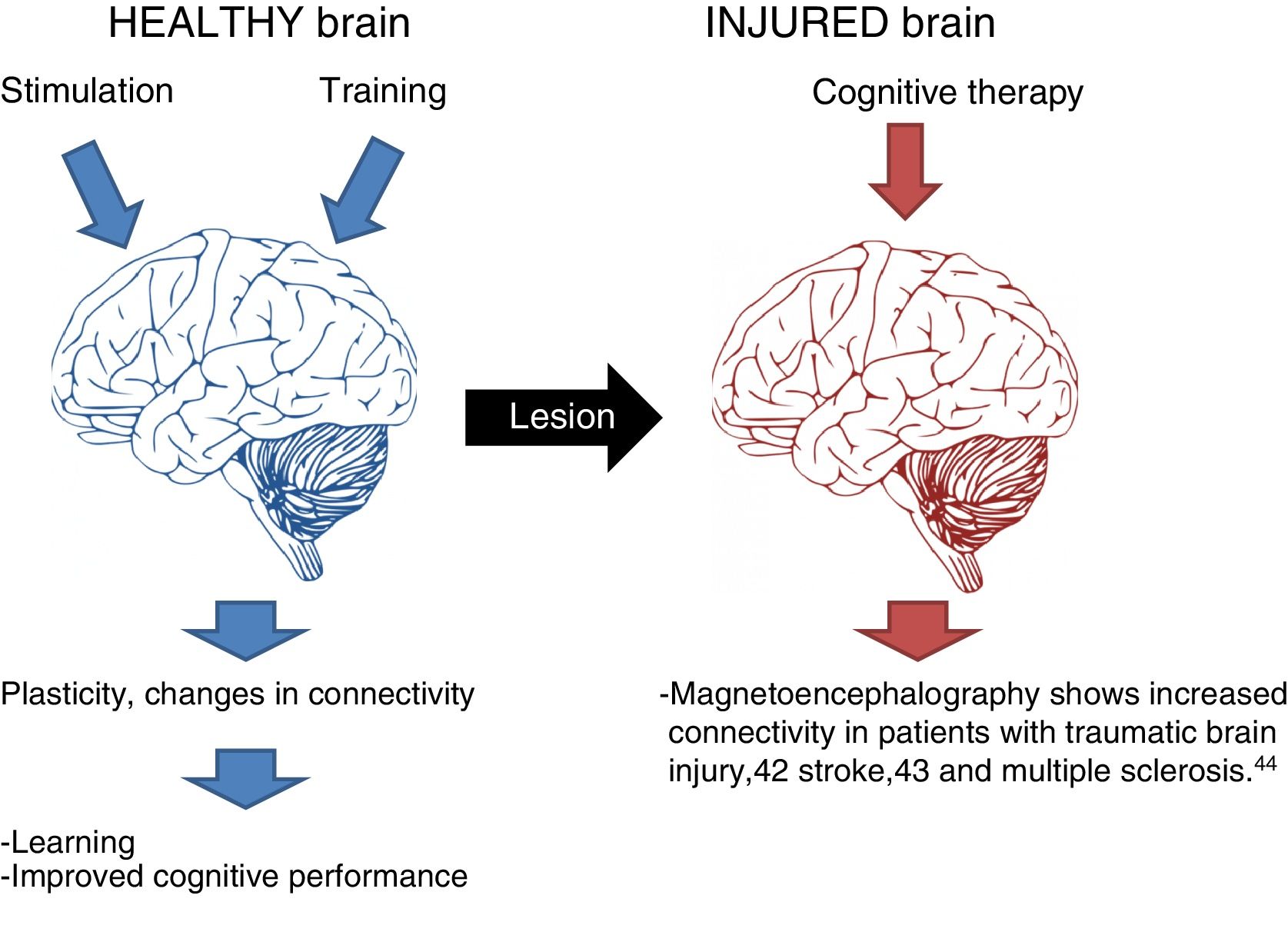
Plasticity and brain repairThe great advantages of the brain's network-based functioning are the resulting plasticity and mutability. Over 50 years ago, Hebb29 proposed that experience may give rise to a reorganisation of neural connections in the cortex; since then, cortical plasticity has been a field of extensive study, both in relation to learning30 and to the brain's response to injury.31 Given the existence of functional networks, reorganising these would enable the functional recovery of the brain; therefore, the phenomenon of neuroplasticity, together with the brain's networked structure and connectivity, enables all the necessary changes to take place for the system to be repaired following injury.32
Plasticity is expressed in varying forms in brain injuries, ranging from functional modifications of existing structures to the growth and proliferation of new structures and neurons.33 In this way, the brain seeks ways of repairing itself, beginning a cascade of regenerative events by creating synapses (synaptogenesis) in perilesional areas and neurons (neurogenesis) in the subgranular zone of the dentate gyrus and the subventricular zone.34 The cells produced in the neurogenic niches are able to migrate towards the damaged tissue, guided by the presence of specific proteins or chemotactic factors.35 Certain trophic factors also mediate the processes of cell and fibre regeneration. Examples are brain-derived neurotrophic factor, neuropsin (involved in neural growth), and the Nogo-A and LINGO-1 proteins (which inhibit the growth of nerve fibres).
Plasticity as the basis of cognitive and behavioural therapyPlasticity mechanisms are triggered at the moment of brain injury, enabling some amount of spontaneous recovery and repair. This is limited, however: recovery is most evident in the first 3 to 6 months following the injury, and while it does continue for several years after this, it occurs at a “negatively accelerating” rate. The implication of this is that as time progresses, changes become more difficult to observe. Cognitive and behavioural therapy has been proposed as a possible non-pharmacological intervention that may strengthen recovery.
Cognitive therapy acts on the alterations that occur following brain injury, with a view to restoring or compensating for the damaged function in order to improve the patient's abilities and promote reincorporation into work and everyday activities (Fig. 1).36
The effectiveness of this therapy is a complex issue, although sufficient data is available to recommend specific types of cognitive rehabilitation for problems with attention, information processing speed, memory, and language.37,38
Various fMRI studies have found evidence that the brain reorganises itself during the recovery period following a brain injury; however, they do not describe the cooperation of adjacent or distant brain regions.39 The white matter is also involved in the restructuring associated with recovery.40 It is therefore appropriate to consider the observable changes in the interaction between different brain areas, rather than only local modifications to functional activation patterns.41 In other words, the neural network–based functioning of the brain improves our understanding of the relationship between observable plasticity and recovery mechanisms. Magnetoencephalography studies of patients with TBIs have shown increased connectivity after patients participated in an intensive programme of cognitive therapy.42
An fMRI study into patients with stroke revealed increased connectivity in regions functionally related to the hippocampus after 3 months of computer-assisted cognitive therapy.43
A similar phenomenon occurs in patients with multiple sclerosis; one study found increased resting-state functional connectivity in the anterior cingulate and inferior parietal cortices after 8 weeks of the same treatment.44
ConclusionThe brain functions holistically by means of an extensive network of circuits which are responsible for all sensorimotor, vegetative, and mental processes. Understanding of the brain's connectivity and plasticity offers a new perspective from which to approach brain functioning and disease and the repair and recovery mechanisms that constitute the basis of cognitive and behavioural therapy.
Conflicts of interestThe authors have no conflicts of interest to declare.
We are grateful to Dr Frank García for her critical reading of the manuscript and for her suggestions.
Please cite this article as: Lubrini G, Martín-Montes A, Díez-Ascaso O, Díez-Tejedor E. Enfermedad cerebral, conectividad, plasticidad y terapia cognitiva. Una visión neurológica del trastorno mental. Neurología. 2018;33:187–191.