Cervical artery dissections account for over 20% of cases of stroke in patients younger than 65, with an annual incidence of 2.6 to 2.9 cases per 100000 population.1 It predominantly affects men, with 45 years being the mean age of affected patients.2,3 The main risk factors include arterial hypertension, low cholesterol levels, hyperhomocysteinaemia, and migraine with aura,4–6 as well as genetic diseases predisposing to an intrinsic weakness of the vessel wall.7 Trigger factors include trauma and cervical manipulation, as well as some types of infection.8
Cervical artery dissections may be classified according to the artery affected (carotid or vertebral) and the location (intracranial or extracranial). The location most frequently described is the extracranial internal carotid artery, at 2 to 3cm from bifurcation.9
Anatomical factors include elongation of the styloid processes, and their proximity to the cervical vessel bundle.10,11 Eagle syndrome refers to 2 entities. The first and more frequent, known as classic Eagle syndrome, refers to elongated styloid process accompanied by throat pain, dysphagia, tinnitus, otalgia, neck pain, or unilateral facial pain. Patients may also report the sensation of a foreign object in the throat. The second and far less frequent entity is known as stylocarotid syndrome, a vascular variant of Eagle syndrome, in which there is contact between the styloid process and the extracranial segment of the internal carotid artery, causing arterial compression or dissection, potentially leading to transient ischaemic attack or ischaemic brain lesions. A recent article proposed proximity of the C1 transverse process to the styloid process (regardless of its length) as a cause of classic Eagle syndrome.12
We present the case of a patient with extracranial carotid dissection secondary to a giant C1 transverse process.
Clinical caseOur patient is a 53-year-old man, a mechanic by trade, with no vascular risk factors or known history of disease, who attended the emergency department due to sudden onset of left-sided limb weakness while he was working. The initial assessment revealed right cortical hemispheric syndrome.
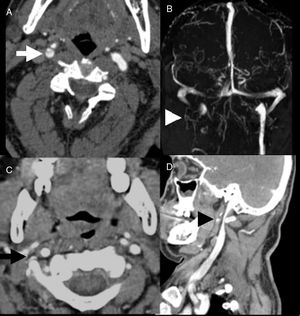
A multimodal brain CT scan was performed due to suspicion of ischaemic stroke. The simple CT scan showed no alterations. Perfusion-weighted sequences revealed delayed time to peak in the superficial territory of the right middle cerebral artery (RMCA), with a decrease in relative cerebral blood flow in the deep territory but with preserved relative blood flow volume. The CT angiography (Fig. 1A) revealed an intimal flap, with absence of flow in the right internal carotid artery. The intracranial study revealed an occlusion of the proximal M2 segment of the RMCA and persistent flow through the anterior and posterior communicating arteries. We placed 2 carotid stents and performed mechanical thrombectomy for intracranial thrombus extraction, using a Trevo® device; this achieved partial recanalisation due to persistent occlusion of the angular branch. Dual antiplatelet therapy was started immediately after the procedure, and the patient showed almost complete recovery of the motor symptoms.
(A) CT angiography (axial) showing right internal carotid artery dissection (arrow). (B) Venous MRI angiography showing absence of flow in the right jugular vein (arrowhead). (C and D) CT angiography sequences revealing bilateral extrinsic compression of the vessel bundle by a giant C1 transverse process (arrow and arrowhead).
Follow-up neuroimaging consisted in a brain MRI scan and MRI angiography, revealing acute ischaemic lesions in temporal and frontoparietal cortical regions and in the right basal ganglia. Venous angiography (Fig. 1B) revealed absence of flow in the right jugular vein. A neck CT scan (Fig. 1C and D) showed bilateral extrinsic compression of the vessel bundle (predominantly affecting the jugular veins, and more pronounced in the right side) due to a giant C1 transverse process. The patient subsequently reported that his work involved vigorous rotations of the head, although he had no history of neck trauma or previous symptoms suggestive of local compression.
DiscussionArterial dissections are responsible for up to 20% of strokes in patients younger than 65. The main cause is trauma, and the main clinical manifestation is lateral cervical pain. Possible associated factors include elongation of the styloid processes, and their proximity to the internal carotid artery, leading to classic Eagle syndrome or stylocarotid syndrome. However, the literature includes few descriptions of elongated styloid process as the cause of carotid dissection.13 Elongation of the hyoid bone has also been proposed as a possible cause.14 It has recently been suggested that the C1 transverse process may be another cause of classic Eagle syndrome, with some of the reported cases also presenting internal jugular vein compression.12 Other authors have described jugular vein compression due to giant C1 transverse process as an extrinsic cause of chronic cerebrospinal venous insufficiency.15
In our patient, whose work demanded repeated, vigorous rotations of the head, we suspect a compression mechanism similar to that observed in patients with giant styloid process, given the proximity to the neck vessel bundle; this hypothesis is supported by the ipsilateral internal jugular vein compression. In a recently described series of 5 cases, styloid/C1 transverse process juxtaposition was reported as the cause of a case of classic Eagle syndrome associated with internal jugular vein compression.12 This series and the ipsilateral jugular vein compression observed in our patient support the hypothesis of compression of cervical vessels by a giant C1 transverse process as the cause of dissection.
FundingThis study has received no funding.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Vicente Pascual M, Fortuny Garrido L, Olondo Zulueta ML, Llull Estrany L. Disección carotídea secundaria a traumatismo carotídeo por apófisis transversa gigante de C1. Neurología. 2019;34:485–487.