Chronic fatigue syndrome (CFS) is characterised by the presence of intractable fatigue and non-restorative sleep, symptoms which are also very prevalent in multiple diseases and appear as side effects of different drugs. Numerous studies have shown a high prevalence of sleep disorders in patients with CFS. However, non-restorative sleep and fatigue are frequently symptoms of the sleep disorders themselves, so primary sleep disorders have to be ruled out in many cases of CFS.
DevelopmentThis review was performed using a structured search of the MeSH terms ([Sleep]+[Chronic fatigue syndrome]) in the PubMed database.
ConclusionIdentifying primary sleep disorders in patients meeting diagnostic criteria for CFS will allow for a more comprehensive treatment approach involving new diagnostic and therapeutic strategies that may improve quality of life for these patients.
El síndrome de fatiga crónica (SFC) se caracteriza por la presencia de fatiga intratable y sueño no reparador, síntomas con una alta prevalencia en múltiples enfermedades y/o como efecto secundario de diferentes fármacos. Diferentes trabajos demostraron una alta prevalencia de los trastornos del sueño asociados al SFC. Además, los síntomas de sueño no reparador y fatiga son síntomas frecuentes en los trastornos del sueño, lo que hace que en muchos pacientes con SFC haya que descartar un trastorno de sueño primario.
DesarrolloEste trabajo se ha realizado a través de una búsqueda sistematizada con términos MeSH ([Sleep]+[Chronic fatigue syndrome]) en la base de datos PubMed.
ConclusiónLa identificación de los diferentes trastornos primarios del sueño en los pacientes con criterios diagnósticos de SFC, nos permitiría realizar un abordaje del paciente más completo, con nuevas estrategias diagnósticas y terapéuticas que podrían mejorar la calidad de vida de estos pacientes.
Chronic fatigue syndrome (CFS) has sparked growing interest in recent decades, despite which the condition continues to be controversial. The main reason for this is the lack of objective evidence of the syndrome. CFS is a heterogeneous multisystem disorder of unknown origin characterised by generalised fatigue lasting over 6 months, worsening after exercise (98%), and associated with recurrent headache (90%) and concentration and/or memory problems (85%).1 These symptoms are usually associated with non-restorative sleep (94%), musculoskeletal pain (75%), swollen lymph nodes, and/or psychiatric disorders (65%).1 Prevalence of CFS is estimated at 0.007%-2.8% of the general adult population, predominantly affecting women (female-to-male ratio of 4:1).2
The current concept of CFS overlaps with such other syndromes as fibromyalgia, temporomandibular pain, irritable bowel syndrome, and sleep disorders (SD). According to the third edition of the International Classification of Sleep Disorders (ICSD-3),3 over 90 well-characterised SDs have been described. Some of these disorders are highly prevalent among the general population: insufficient sleep syndrome (40%), insomnia (20%), sleep-related breathing disorders (2%-5%), restless legs syndrome (RLS) (2%), periodic limb movement disorder (PLMD), delayed sleep-wake phase disorder, and parasomnia.3 SDs have also been associated with increased mortality; a higher prevalence of cardiovascular disease, workplace and traffic accidents, and psychiatric disorders; and poorer cognitive function and performance.4,5
SDs and CFS share several symptoms, such as fatigue and non-restorative sleep, both of which are subjective and currently impossible to quantify. Non-restorative sleep, one of the most common symptoms in patients with CFS (87%-95%),6,7 constitutes a key symptom for CFS diagnosis.8 The latest diagnostic guidelines for CFS include such other symptoms as excessive daytime sleepiness (EDS), difficulty falling asleep, and sleep fragmentation7; these symptoms are also very common in patients with SDs.3 The clinical overlap between SDs and CFS, combined with the current lack of knowledge of SDs, may explain the delayed diagnosis in these entities.
A comprehensive review of the topic was conducted in order to address the following questions: (1) what symptoms of SDs overlap with those of CFS? (2) what is the prevalence of SD in patients with CFS? (3) what polysomnographic alterations have been observed in CFS? and (4) how can SDs be diagnosed in patients with CFS and differentiated from the latter condition? To aid in clinical differentiation between these disorders, useful clinical guidelines for SD screening are provided, together with a diagnostic algorithm for SDs in patients with CFS, according to the sleep pattern they present. Identifying SDs in patients with suspected CFS will provide new diagnostic and treatment strategies to improve these patients’ quality of life.
MethodsA systematic literature search was conducted on MEDLINE (PubMed) using the MeSH terms [sleep]+[chronic fatigue syndrome]. Inclusion criteria were as follows: articles published in indexed journals, written in Spanish or English, and published prior to 31 December 2014. The study includes original articles reporting prospective and retrospective studies, systematic reviews, and meta-analyses. After reading the abstracts and selecting those articles that appeared to be relevant, the full texts of the selected articles, and the cited references, were reviewed.
Symptoms of sleep disorders overlapping with chronic fatigue syndromeFatigue, EDS, and non-restorative sleep are very common symptoms of CFS.8 However, the diagnostic criteria for many SDs defined in the ICSD-33 (insomnia, sleep-related breathing disorders, central disorders of hypersomnolence, circadian rhythm sleep-wake disorders, and sleep-related movement disorders) greatly coincide with those of CFS, which makes it more difficult to differentiate the 2 conditions.
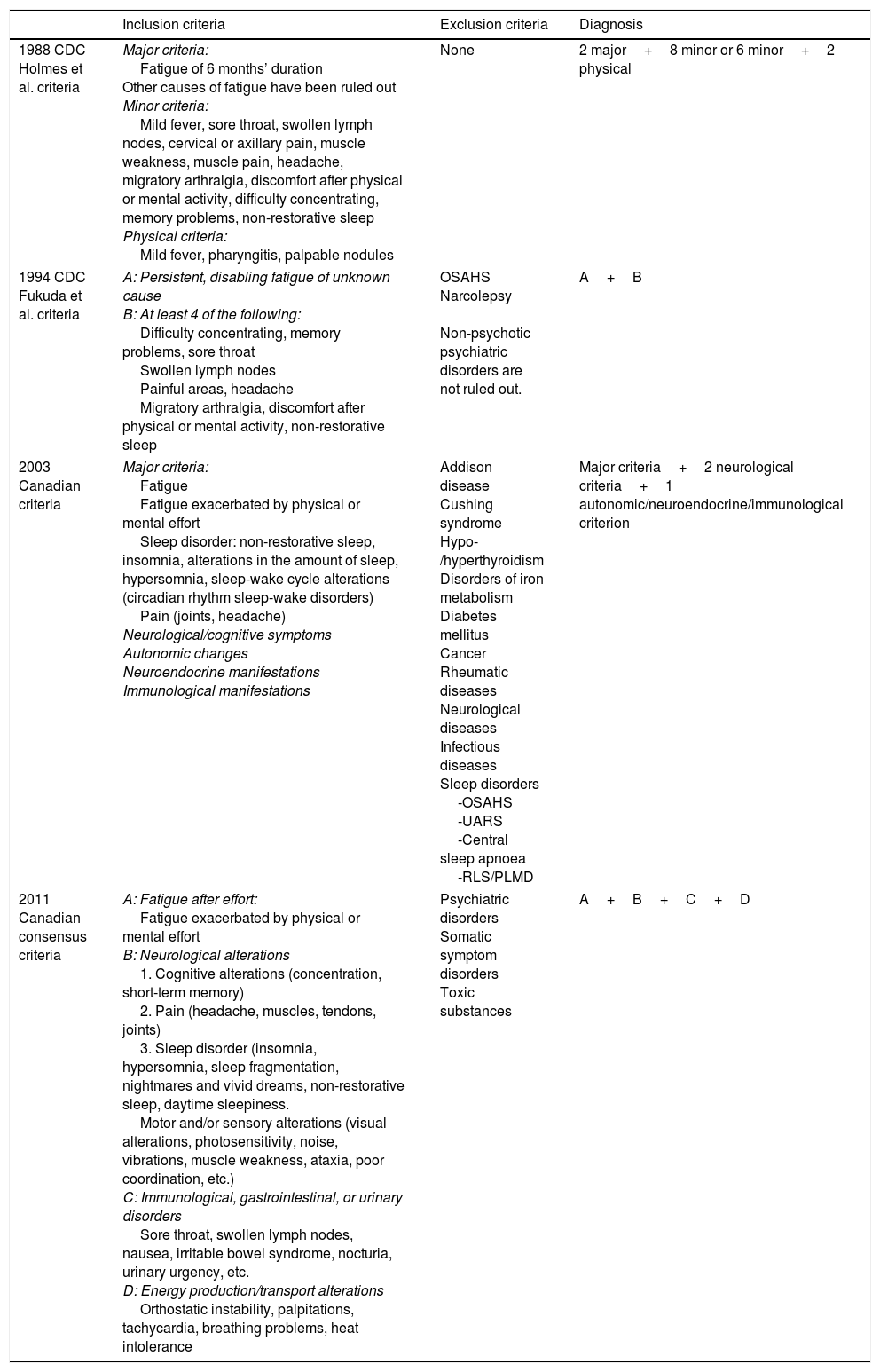
Since 1988, diagnostic criteria for CFS have always included very frequent symptoms of primary SDs (Table 1). The 1988 (Holmes et al.9) and 1994 (Fukuda et al.10) Centers for Disease Control and Prevention (CDC) criteria include non-restorative sleep as a minor symptom. Furthermore, the diagnostic criteria proposed by Fukuda et al. include obstructive sleep apnoea/hypopnoea syndrome (OSAHS) and narcolepsy as exclusion criteria for CFS. The Canadian criteria, published in 2003, list non-restorative sleep as a major diagnostic criterion, and also include such other symptoms as EDS, alterations in sleep duration, and sleep-wake cycle alterations.1 These criteria also list OSAHS, central sleep apnoea, RLS, and PLMD as exclusion criteria. Lastly, the 2011 International Consensus Criteria1 list sleep-related symptoms within the neurological alterations section; these include insomnia, EDS, non-restorative sleep, long naps, sleep fragmentation, nightmares, and vivid dreams. Although the 2011 International Consensus did not include any SD among the exclusion criteria, it emphasised that these disorders may be present and should be considered as a comorbidity of CFS, underscoring the importance of identifying and treating each entity independently.
Diagnostic criteria for chronic fatigue syndrome.
| Inclusion criteria | Exclusion criteria | Diagnosis | |
|---|---|---|---|
| 1988 CDC Holmes et al. criteria | Major criteria: Fatigue of 6 months’ duration Other causes of fatigue have been ruled out Minor criteria: Mild fever, sore throat, swollen lymph nodes, cervical or axillary pain, muscle weakness, muscle pain, headache, migratory arthralgia, discomfort after physical or mental activity, difficulty concentrating, memory problems, non-restorative sleep Physical criteria: Mild fever, pharyngitis, palpable nodules | None | 2 major+8 minor or 6 minor+2 physical |
| 1994 CDC Fukuda et al. criteria | A: Persistent, disabling fatigue of unknown cause B: At least 4 of the following: Difficulty concentrating, memory problems, sore throat Swollen lymph nodes Painful areas, headache Migratory arthralgia, discomfort after physical or mental activity, non-restorative sleep | OSAHS Narcolepsy Non-psychotic psychiatric disorders are not ruled out. | A+B |
| 2003 Canadian criteria | Major criteria: Fatigue Fatigue exacerbated by physical or mental effort Sleep disorder: non-restorative sleep, insomnia, alterations in the amount of sleep, hypersomnia, sleep-wake cycle alterations (circadian rhythm sleep-wake disorders) Pain (joints, headache) Neurological/cognitive symptoms Autonomic changes Neuroendocrine manifestations Immunological manifestations | Addison disease Cushing syndrome Hypo-/hyperthyroidism Disorders of iron metabolism Diabetes mellitus Cancer Rheumatic diseases Neurological diseases Infectious diseases Sleep disorders -OSAHS -UARS -Central sleep apnoea -RLS/PLMD | Major criteria+2 neurological criteria+1 autonomic/neuroendocrine/immunological criterion |
| 2011 Canadian consensus criteria | A: Fatigue after effort: Fatigue exacerbated by physical or mental effort B: Neurological alterations 1. Cognitive alterations (concentration, short-term memory) 2. Pain (headache, muscles, tendons, joints) 3. Sleep disorder (insomnia, hypersomnia, sleep fragmentation, nightmares and vivid dreams, non-restorative sleep, daytime sleepiness. Motor and/or sensory alterations (visual alterations, photosensitivity, noise, vibrations, muscle weakness, ataxia, poor coordination, etc.) C: Immunological, gastrointestinal, or urinary disorders Sore throat, swollen lymph nodes, nausea, irritable bowel syndrome, nocturia, urinary urgency, etc. D: Energy production/transport alterations Orthostatic instability, palpitations, tachycardia, breathing problems, heat intolerance | Psychiatric disorders Somatic symptom disorders Toxic substances | A+B+C+D |
CDC: US Centers for Disease Control and Prevention; PLMD: periodic limb movement disorder; RLS: restless legs syndrome; UARS: upper airway resistance syndrome.
As mentioned previously, many of the diagnostic criteria for CFS include such symptoms as fatigue, EDS, and non-restorative sleep; however, these terms are often ill-defined or confusing. Therefore, the most standardised definition of each term is provided, with a view to using these terms correctly and uniformly.
FatigueFrom a clinical viewpoint, fatigue includes a physical component, manifesting as difficulty initiating an activity (perception of generalised weakness with no objective findings) and reduced ability to maintain activity, and a mental component, in the form of difficulty concentrating, memory problems, and emotional instability.
According to various population studies, fatigue has a high prevalence, affecting 6%-7.5% of the general population11–14 and representing 21%-33% of all complaints in primary care consultations.1,15,16 Fatigue is a frequent symptom associated with numerous factors and diseases (psychological, pharmacological, endocrine, metabolic, neoplastic, haematological, infectious, cardiopulmonary, inflammatory, and sleep-related). However, there is still a large group of patients in whom the cause of chronic fatigue is unidentifiable (37%)17; in these patients, diagnosis must be made by exclusion and consider idiopathic chronic fatigue, CFS, and/or fibromyalgia.18 Idiopathic chronic fatigue is defined as disabling fatigue lasting over 6 months, with no apparent medical or pharmacological cause, and meeting none of the diagnostic criteria for CFS. CFS, on the other hand, is defined as disabling fatigue lasting over 6 months and accompanied by certain symptoms (Table 1).
Fatigue should be distinguished from EDS (see following section), dyspnoea, and muscle weakness; these symptoms may also be associated with fatigue, however.
The ICSD-3 includes the symptom of fatigue as one of the diagnostic criteria for insomnia, sleep-related breathing disorders, circadian rhythm sleep-wake disorders, RLS, and PLMD. Other sleep disorders do not rank fatigue as a diagnostic criterion; however, fatigue may also present as a secondary or associated symptom in these cases. This is the case with central disorders of hypersomnolence (primary hypersomnia and insufficient sleep syndrome) and parasomnia (somnambulism, nightmares, and REM sleep behaviour disorder).
Excessive daytime sleepinessEDS is defined as the need to sleep despite the absence of mental and/or physical fatigue. Unlike patients with fatigue, those with EDS avoid passive or sedentary activities, given that these situations cause sleepiness. Patients with fatigue, in contrast, prefer to remain at rest, as physical or mental activity worsens their fatigue. In patients with no primary SD, sleepiness only improves with sleeping.
Sleepiness may be present in up to 30% of the general population.3 Likewise, many patients with CFS (30%-50%) may also present EDS according to subjective (Epworth Sleepiness Scale)7,19–22 and objective tests (Multiple Sleep Latency Test [MSLT]).23,24 This increases the difficulty of diagnosing CFS and differentiating it from central disorders of hypersomnolence, especially if the physician is not familiar with these entities. We must also consider the clinical challenge involved in differentiating fatigue and EDS. According to a study by Neu et al.,25 80% of patients cannot differentiate sleepiness from fatigue. Despite this difficulty, several authors insist that an effort should be made to assess each of these conditions separately and independently.25,26
To date, no test has been developed to objectively evaluate and detect fatigue as a symptom; the only assessment tools available are subjective questionnaires (Multidimensional Fatigue Inventory [MFI-20], Chalder Fatigue Scale, Fatigue Severity Scale). For sleepiness, however, in addition to a number of subjective tools (Epworth Sleepiness Scale, Stanford Sleepiness Scale, sleep diary), several objective tools are available for the evaluation of EDS; these include the MSLT, the Maintenance of Wakefulness Test, and actigraphy. According to the American Academy of Sleep Medicine,3 the MSLT is indicated for diagnosing narcolepsy and primary hypersomnia and studying those cases where fatigue and EDS are difficult to distinguish.
Non-restorative sleepNon-restorative sleep, an ambiguous and poorly defined symptom, has traditionally been assessed as a dichotomous variable (yes/no). Current studies aim to provide a more accurate description of this term. Stone et al.27 define non-restorative sleep as a feeling of being unrefreshed upon awakening, despite having slept sufficient hours and in the absence of any other primary SD: some studies conclude that 50% of patients with non-restorative sleep may also have a primary SD.28
Non-restorative sleep is a very frequent symptom in the general population, with an estimated prevalence of 1.4%-35%27 and manifesting with fatigue as an associated symptom in up to 20% of cases.29 It is also a very frequent symptom in CFS (87%-95%),7 constituting one of the diagnostic criteria for this condition and for multiple primary SDs defined by the ICSD-3.3
Non-restorative sleep has been associated with the worsening of daytime symptoms in patients with CFS.29 Despite the current lack of evidence about the process of psychophysiological recovery during sleep, sleep deprivation (whether acute or chronic) and sleep fragmentation have been found to increase sleepiness and fatigue and to cause neurocognitive alterations.30
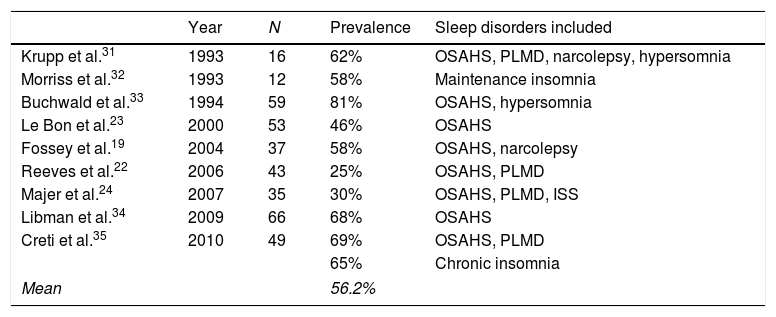
Prevalence of sleep disorders in chronic fatigue syndromeAccording to the published evidence, the mean prevalence of sleep disorders in patients with CFS is estimated at 56% (range 18%-81%) (Table 2).8,19,21–24,31–36 Some authors also describe a greater level of functional impairment in patients with CFS plus an associated primary SD.32
Prevalence of sleep disorders in patients with chronic fatigue syndrome.
| Year | N | Prevalence | Sleep disorders included | |
|---|---|---|---|---|
| Krupp et al.31 | 1993 | 16 | 62% | OSAHS, PLMD, narcolepsy, hypersomnia |
| Morriss et al.32 | 1993 | 12 | 58% | Maintenance insomnia |
| Buchwald et al.33 | 1994 | 59 | 81% | OSAHS, hypersomnia |
| Le Bon et al.23 | 2000 | 53 | 46% | OSAHS |
| Fossey et al.19 | 2004 | 37 | 58% | OSAHS, narcolepsy |
| Reeves et al.22 | 2006 | 43 | 25% | OSAHS, PLMD |
| Majer et al.24 | 2007 | 35 | 30% | OSAHS, PLMD, ISS |
| Libman et al.34 | 2009 | 66 | 68% | OSAHS |
| Creti et al.35 | 2010 | 49 | 69% | OSAHS, PLMD |
| 65% | Chronic insomnia | |||
| Mean | 56.2% | |||
PLMD: periodic limb movement disorder; OSAHS: obstructive sleep apnoea/hypopnoea syndrome; ISS: insufficient sleep syndrome.
These studies reporting a higher prevalence of SD, however, have a number of limitations: they all include a small number of patients, and tend only to describe subjective clinical manifestations and to rule out only primary SD (OSAHS and/or narcolepsy and/or PLMD); and the patients included were referred to a sleep unit for assessment. These limitations may have affected the accuracy of the findings regarding SD prevalence.
These studies mainly follow the diagnostic criteria established by Fukuda et al.,10 according to which OSAHS and narcolepsy must be excluded for CFS to be diagnosed; despite this, however, these 2 disorders are highly prevalent among the populations included in these studies. Other relatively frequent primary SDs include chronic insomnia, primary hypersomnia, insufficient sleep syndrome, poor sleep hygiene, and circadian rhythm sleep-wake disorders. However, some studies have reported pathological levels of EDS (<8min in MSLT findings) in 22%-41% of patients,23,24,31,33 which suggests that these patients have such conditions as primary hypersomnia, insufficient sleep syndrome, or poor sleep hygiene. The same is true for chronic insomnia, with an estimated prevalence of 68%-86%, according to some studies.19,35
This explains the current debate around the association between SDs and CFS. According to some researchers, presence of SDs should rule out CFS; others, however, regard SDs and CFS as concomitant disorders. There is insufficient evidence to confirm the hypothesis that SDs are concomitant to CFS. Firstly, Nisenbaum et al.8 conducted a population study into CFS over the course of 3 years. According to their results, diagnostic criteria for CFS persisted throughout the study period in 20%-33% of the patients and fully or partially remitted in 56%; 23% received alternative diagnoses (SDs in 20%: OSAHS and narcolepsy). Secondly, the concomitant disease hypothesis was introduced by Libman et al.34 in a study including patients with CFS and associated OSAHS. These authors compared patients displaying good compliance with CPAP to non-compliant patients, finding no significant differences in CFS symptoms. This study included a very small sample and did not provide an objective definition of treatment compliance. However, it did find non-significant improvements; more promising results may have been achieved if treatment compliance had been monitored more thoroughly and the sample had been larger. In another study describing 4 patients with OSAHS and CFS who received treatment with CPAP, compliant patients displayed total symptom resolution, whereas non-compliant and partially compliant patients displayed no improvements.37 Despite the small sample size, the results of the latter study are more in line with those published by Tomfohr et al.,38 who conducted a randomised placebo-controlled study of patients diagnosed with OSAHS, finding that patients treated with CPAP manifested significant improvements in fatigue compared to those receiving placebo CPAP.
According to the Canadian diagnostic criteria for CFS, identifying SDs is essential in patients with suspected CFS, since the presence of these disorders should be regarded as an exclusion criterion for CFS. It is therefore logical to consider that the different SDs associated with fatigue and CFS may improve significantly with adequate treatment. Only in the event that SDs do not improve and/or residual symptoms meeting the criteria for CFS persist should patients be re-evaluated and SDs be considered as a comorbidity of CFS.
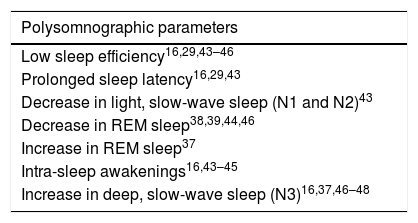
Polysomnographic alterations in chronic fatigue syndromePolysomnographic findings of sleep architecture in patients with chronic fatigue syndromePolysomnographic findings of sleep architecture in these patients vary between studies (Table 3). Some studies have found no differences in sleep architecture between patients with CFS and controls.22,39,40 A noteworthy study by Whichita et al.22 found no polysomnographic alterations in patients with CFS compared to controls; in fact, values were within normal ranges. Patients with CFS, in contrast, reported poorer sleep quality and higher levels of somnolence and fatigue.24 Another study including a series of monozygotic twin pairs where one twin had CFS while the co-twin did not41 reported a greater percentage of deep slow-wave sleep and REM sleep, although differences were not clinically relevant. In another study of CFS-discordant twin pairs, however, twins with CFS reported more sleepiness, fatigue, and poorer sleep quality.21 This led to the hypothesis that patients with chronic fatigue had a distorted perception of sleep rather than an abnormal sleep architecture.
Summary of polysomnographic parameters in patients with chronic fatigue syndrome.
| Polysomnographic parameters |
|---|
| Low sleep efficiency16,29,43–46 |
| Prolonged sleep latency16,29,43 |
| Decrease in light, slow-wave sleep (N1 and N2)43 |
| Decrease in REM sleep38,39,44,46 |
| Increase in REM sleep37 |
| Intra-sleep awakenings16,43–45 |
| Increase in deep, slow-wave sleep (N3)16,37,46–48 |
REM: rapid eye movement.
The study of sleep microstructure evaluates small variations in electroencephalographic (EEG) activity during sleep. The most frequently studied parameters are alpha intrusions into slow-wave sleep, quantitative EEG analysis (Fourier transform), and the cyclic alternating pattern.
Alpha intrusions into slow-wave sleep: presence of alpha waves (8-12Hz), which are typical of wakefulness, during deep sleep (N3 stage). This represents an intrusion of wakefulness into sleep and may explain the feeling of non-restorative sleep. This concept, however, is no longer widely accepted in CFS, for 2 main reasons: firstly, conflicting results have been obtained32,42–45; and secondly, the presence of alpha intrusions is a parameter also described in such other entities as fibromyalgia, rheumatoid arthritis, systemic lupus erythematosus, insomnia, OSAHS, and PLMD, and even in healthy individuals.3 In a study conducted by Ball et al.,41 which included a series of CFS-discordant twin pairs, alpha intrusions were found in both groups; this suggests that they are caused by genetic factors rather than by CFS itself.
Quantitative EEG analysis: also known as power spectral analysis, this system is based on the Fourier transform and analyses different frequency bands of EEG signal. Quantitative EEG analysis has also been unsuccessful in detecting alpha intrusions (increase in alpha frequencies) into slow-wave sleep. Armitage et al.40 analysed a cohort of CFS-discordant homozygotic twin pairs with quantitative EEG, finding no differences between twins with and without CFS. Other studies have described a decrease in alpha frequency bands in the CFS group46,47 and an increase in delta frequency bands, that is, deep slow-wave sleep (N3 stage); these findings are normally associated with restorative sleep.20,40,46,47
Cyclic alternating pattern: this parameter is regarded as a sign of sleep instability.48 Only one study has analysed this pattern, reporting a significant increase in the cyclic alternating pattern rate compared to the control group, which suggests greater sleep instability.47
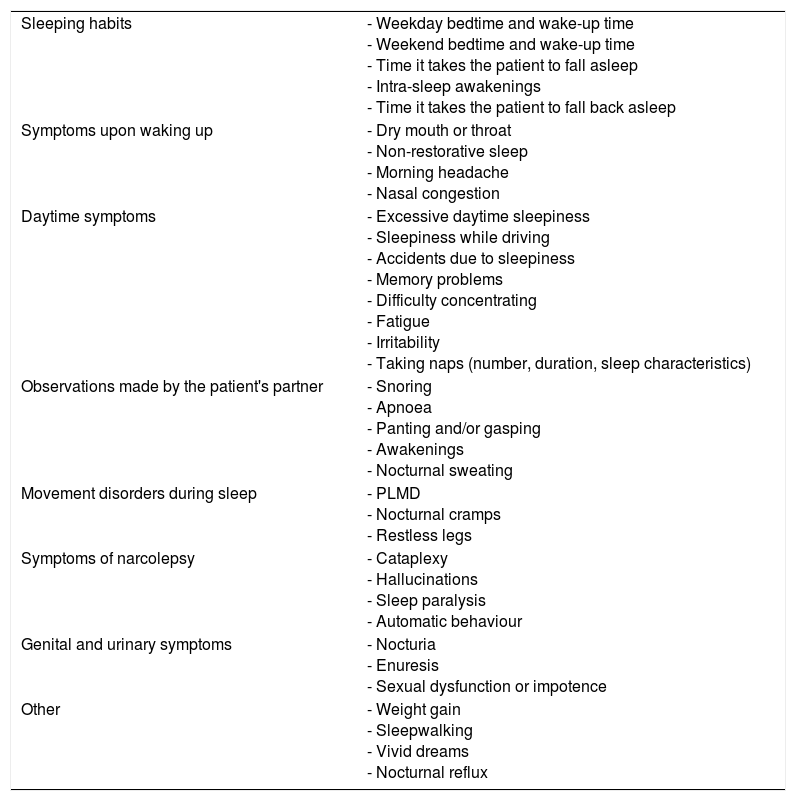
The above suggests high prevalence of primary SDs among patients with CFS and that symptoms of CFS overlap to a great extent with those of SDs. Patients with CFS normally have poor sleep quality, reported as a feeling of non-restorative sleep. This is a rather ambiguous concept; presence of non-restorative sleep should not be described in binary terms of presence/absence. Physicians should aim to gather as much information as possible in order to better define and manage the underlying SDs. In view of this, physicians should ask patients whether they would describe their sleep as non-restorative and enquire into their sleep-wake schedule, number of hours of sleep, number of intra-sleep awakenings, intra-sleep wakefulness time, and subjective sleep efficiency. They should also enquire about the impact of non-restorative sleep on daytime activity, gathering data on fatigue, feelings of excessive daytime sleepiness, the need to take naps, and the number and duration of these naps. Other relevant data include snoring, sleep apnoea, movements during sleep, nightmares, nocturnal sweating, nocturia, and/or nocturnal reflux (Table 4).
Screening questionnaire for sleep disorders.
| Sleeping habits | - Weekday bedtime and wake-up time - Weekend bedtime and wake-up time - Time it takes the patient to fall asleep - Intra-sleep awakenings - Time it takes the patient to fall back asleep |
| Symptoms upon waking up | - Dry mouth or throat - Non-restorative sleep - Morning headache - Nasal congestion |
| Daytime symptoms | - Excessive daytime sleepiness - Sleepiness while driving - Accidents due to sleepiness - Memory problems - Difficulty concentrating - Fatigue - Irritability - Taking naps (number, duration, sleep characteristics) |
| Observations made by the patient's partner | - Snoring - Apnoea - Panting and/or gasping - Awakenings - Nocturnal sweating |
| Movement disorders during sleep | - PLMD - Nocturnal cramps - Restless legs |
| Symptoms of narcolepsy | - Cataplexy - Hallucinations - Sleep paralysis - Automatic behaviour |
| Genital and urinary symptoms | - Nocturia - Enuresis - Sexual dysfunction or impotence |
| Other | - Weight gain - Sleepwalking - Vivid dreams - Nocturnal reflux |
PLMD: periodic limb movement disorder.
Primary SDs have been reported to be highly prevalent among patients with CFS. Sleep-related breathing disorders are highly prevalent in the general population (2%-5%)4; this rules out OSAHS, for which a highly effective treatment is available, in all patients with CFS. These patients may also present other less well-known but also highly prevalent primary SDs whose specific treatment may improve patients’ quality of life; these include chronic insomnia, PLMD, RLS, circadian rhythm sleep-wake disorders (delayed or advanced sleep-wake phase disorder and/or irregular sleep-wake rhythm disorder), parasomnias (sleepwalking, REM sleep behaviour disorder, and nightmares), poor sleep hygiene, insufficient sleep syndrome, narcolepsy, and/or idiopathic hypersomnia. Gathering basic data on patients’ sleeping habits and history of SDs is therefore essential in screening for any underlying SD (Table 4).
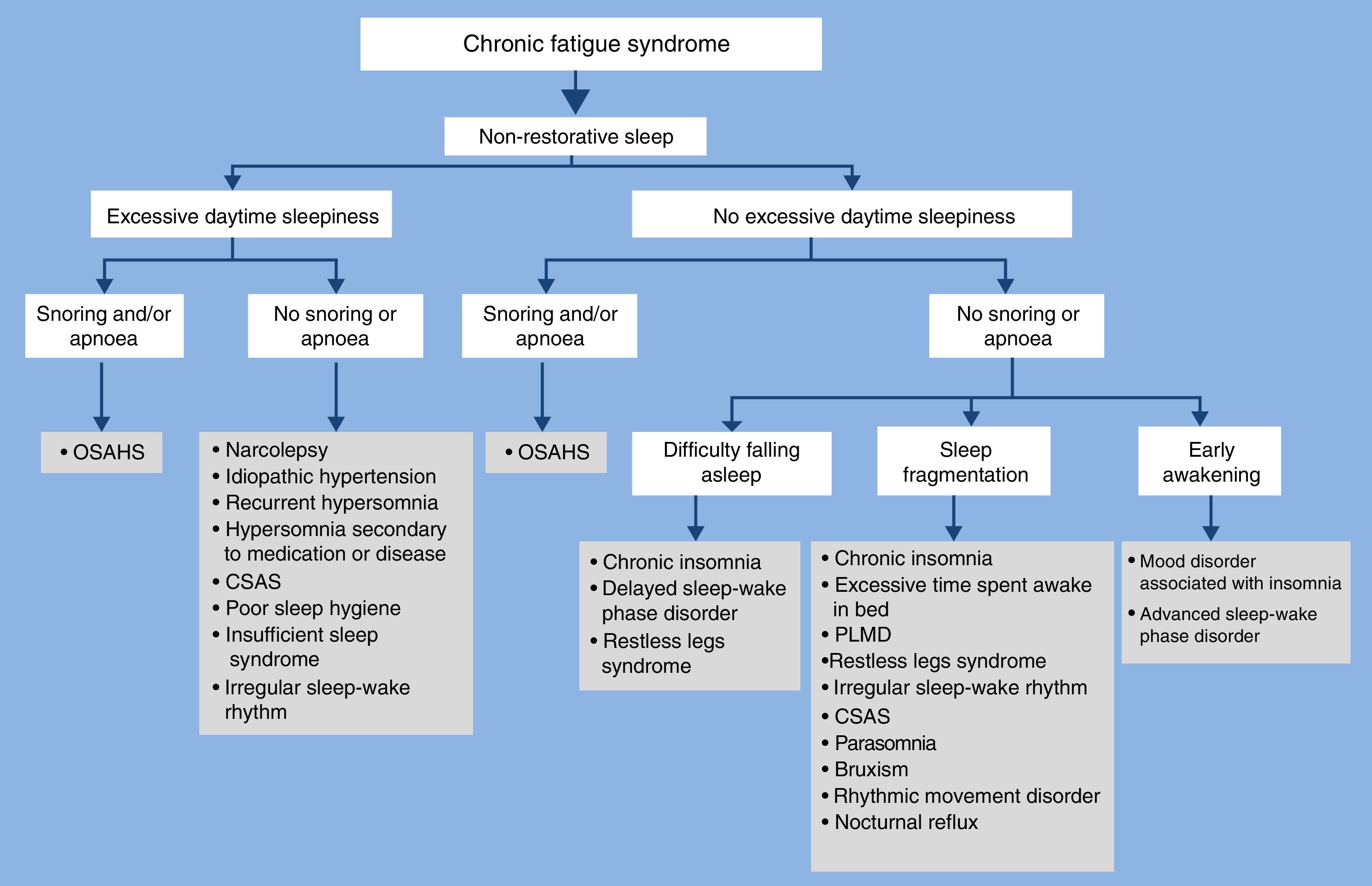
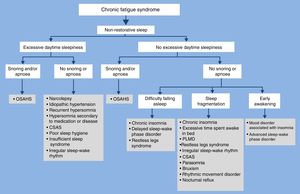
Gotts et al.36 described 4 sleep phenotypes in patients with CFS: deep sleepers, light sleepers, light sleepers with daytime activities affected, and insomniacs (conciliation, maintenance, and/or early awakening). Based on these data, a diagnostic algorithm is proposed for the differential diagnosis of SDs in patients with CFS (Fig. 1).
ConclusionsSymptoms of CFS overlap with those of many other disorders, particularly SDs; this explains why CFS is frequently misdiagnosed as other conditions. Multiple researchers now apply the Fukuda et al. criteria, despite which a high prevalence of primary SDs has been reported. Therefore, with a view to enabling differentiation between CFS and SDs, greater effort should be made to properly define such symptoms as fatigue, EDS, and non-restorative sleep in order to avoid confusion and overlap between symptoms. The concept of non-restorative sleep, which is widely used in CFS, should only be applied to patients who do not feel refreshed upon awakening despite sleeping sufficient hours, after primary SDs have been ruled out. SDs frequently associated with CFS (OSAHS and narcolepsy) must be ruled out in these patients. The presence of other highly prevalent SDs should also be assessed; these include insomnia, insufficient sleep syndrome, poor sleep hygiene, primary hypersomnia, circadian rhythm sleep disorders, PLMD, rhythmic movement disorder, and parasomnias, all of which are very frequently associated with CFS (Fig. 1). Several tools are currently available to diagnose these disorders, including polysomnography and the MSLT; likewise, a number of effective treatments have been developed to improve patients’ quality of life and reduce morbidity and mortality.
Some researchers have suggested that SDs are comorbidities of CFS; it is this author's view, however, that SDs should be regarded as primary disorders, distinct from CFS, and considered an exclusion criterion for CFS diagnosis. Nonetheless, an SD may be considered a comorbidity of CFS when diagnostic criteria for CFS persist despite treatment in a patient with a diagnosis of a primary SD; a re-evaluation is necessary in these cases.
Studies of sleep in patients with CFS are scarce, heterogeneous, and provide conflicting results. Future research should aim to improve patient selection by better identifying concomitant primary SDs and providing a more detailed, uniform description of symptoms. This would produce more homogeneous, conclusive data.
FundingNone declared.
Conflicts of interestThe author has no conflicts of interest to declare. This study has received no funding.
I wish to thank Dr José Alegre Martín, rheumatologist and head of the chronic fatigue syndrome unit at Hospital Universitari Vall d’Hebron, who sparked my interest in this topic.
Please cite this article as: Ferré A. Síndrome de fatiga crónica y los trastornos del sueño: relaciones clínicas y dificultades diagnósticas. Neurología. 2018;33:385–394.