Neurofibromatosis type 1 (NF1) is a common neurocutaneous syndrome often associated with specific cognitive deficits that are rarely monitored during follow-up of these patients.
ObjectiveThe purpose of our study is two-fold. First, we aimed to describe the cognitive profile of patients with NF1 and detect disorders in higher brain functions associated with the disease.
Second, we identified the reasons for consultation associated with school performance in these patients.
MethodsWe conducted a descriptive cross-sectional study of 24 paediatric patients (ages 5–16) with NF1 who underwent neuropsychological assessment.
ResultsThe most frequent reasons for consultation were attention deficits (58.33%), learning disorders (25%), poor motor coordination (25%), and language impairment (0.8%). Although 96% of the patients displayed impairments in at least one of the assessed areas, only 83.34% of the parents had reported such impairments. Attention-deficit/hyperactivity disorder was present in 58.33% of the patients, whereas 33.33% had nonverbal learning disabilities, 20.83% had expressive language disorder, 8.33% had borderline intellectual functioning, 4.16% had mental retardation, and only 4.16% showed no cognitive impairment.
ConclusionHigher brain functions are frequently impaired in paediatric patients with NF1. Although many parents report such disorders, they can go undetected in some cases. Neuropsychological assessment is recommended for all paediatric patients with NF1 to detect cognitive impairment and provide early, effective rehabilitation treatment.
La neurofibromatosis tipo 1 (NF1) es un síndrome neurocutáneo frecuente que en muchos casos se asocia a dificultades cognitivas específicas que habitualmente no son tenidas en cuenta en el seguimiento médico de estos pacientes.
ObjetivoTrazar el perfil cognitivo de pacientes con NF1 detectando trastornos en funciones superiores asociados al mismo.
Identificar motivos de consulta de pacientes pediátricos con NF1 en relación con su desempeño escolar.
MétodosTrabajo descriptivo transversal. Se evaluó neuropsicológicamente a 24 pacientes con NF1 con edades comprendidas entre los 5 y los 16 años de edad.
ResultadosLos motivos de consulta más frecuentes fueron: problemas atencionales (58,33%), aprendizaje (25%), coordinación motora (25%) y lenguaje (0,8%). Si bien el estudio reveló que el 96% de los pacientes tenía compromiso en al menos una de las áreas evaluadas, solo el 83,34% de los padres las refirieron. El 58,33% presentó trastorno por déficit de atención con hiperactividad (TDAH), el 33,33% trastorno de aprendizaje no verbal (TANV), el 20,83% dificultades en aspectos expresivos del lenguaje, el 8,33% coeficiente intelectual (CI) limítrofe, el 4,16% retraso mental y el 4,16% no mostró dificultades.
ConclusionesExiste alta frecuencia de trastornos en funciones superiores en niños con NF1. Aunque muchos padres detectan dichos trastornos, se ha observado que otros son subestimados. Consideramos conveniente que todos los niños con NF1 cuenten con una evaluación neuropsicológica a fin de poder detectar dificultades existentes en cada caso y así poder elaborar una estrategia de rehabilitación cognitiva precoz y efectiva.
In 1882, Friedrich von Recklinghausen described neurofibromatosis type 1 (NF1) as a progressive, multisystem genetic disease of variable expression. It has an incidence of 1 case per 3000 population1–4 and affects men and women equally. The condition is caused by new mutations in 60% of cases.5 The NF1 gene, located on chromosome 17q11.2, encodes the protein neurofibromin; due to its large size, multiple different mutations are possible, resulting in a wide range of clinical phenotypes.
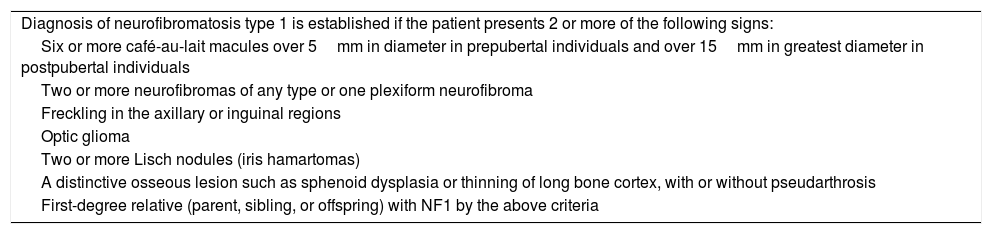
Diagnosis of NF1 is based on a set of clinical criteria proposed by the National Institutes of Health (Table 1). The most frequent manifestations include café au lait spots, neurofibromas, Lisch nodules, optic gliomas, and bone lesions.6,7
National Institutes of Health diagnostic criteria for neurofibromatosis type 1.
| Diagnosis of neurofibromatosis type 1 is established if the patient presents 2 or more of the following signs: |
| Six or more café-au-lait macules over 5mm in diameter in prepubertal individuals and over 15mm in greatest diameter in postpubertal individuals |
| Two or more neurofibromas of any type or one plexiform neurofibroma |
| Freckling in the axillary or inguinal regions |
| Optic glioma |
| Two or more Lisch nodules (iris hamartomas) |
| A distinctive osseous lesion such as sphenoid dysplasia or thinning of long bone cortex, with or without pseudarthrosis |
| First-degree relative (parent, sibling, or offspring) with NF1 by the above criteria |
Recent studies have shown that learning disorders and disruptive behaviours are more prevalent among patients with NF1 than in the general population.8–11 These studies report poor intellectual functioning,12–14 visual perception disorders,15 poor motor coordination,16,17 language disorders,18,19 and especially attention disorders; approximately 50% of patients with NF1 meet diagnostic criteria for attention-deficit/hyperactivity disorder (ADHD).20,21
Although some studies have reported neuropsychological alterations in patients with NF1, few have addressed parents’ concerns about these difficulties. This study establishes the cognitive profile of patients with NF1 and identifies neuropsychological disorders associated with the condition and the cognitive function alterations most frequently motivating consultation.
MethodsThis cross-sectional descriptive study included 24 patients diagnosed with NF1 according to the 1987 National Institutes of Health criteria (Table 1). Patients were aged 5 to 16 years and had visited the paediatric neurology department at Hospital Italiano de Buenos Aires (Argentina). We excluded patients with brain tumours, epilepsy, or pathological neurological examination findings (hemiplegia, quadriparesis, paraparesis, aphasia, cranial nerve dysfunction).
ADHD, language disorders, poor motor coordination, and intellectual disability were diagnosed according to the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders. Diagnosis of nonverbal learning disorder was established using Rourke’s criteria.
Participants completed a thorough neuropsychological test battery, administered by neuropsychologists from our hospital’s paediatric neurology department. The battery included the following tests: 1) Wechsler Intelligence Scale (Wechsler Preschool and Primary Scale of Intelligence [WPPSI-III] or Wechsler Intelligence Scale for Children [WISC-IV], depending on the patient’s age)22; 2) NEPSY II neuropsychological test battery (tower, inhibition, visual attention, statue, and design copying subtests), developed by M. Korkman, U. Kirk, and S. Kemp and adapted to the Spanish language by the University of Seville, the FIVAN Neurological Rehabilitation Centre, and the Pearson Clinical & Talent Assessment R&D department; 3) Rey-Osterrieth Complex Figure Test; 4) Grooved Pegboard Test (developed by Dr Ronald Trites from Royal Ottawa Hospital, Canada); and 5) Conners’ Continuous Performance Test II (CPT-II), developed by Dr C. Keith Conners (version 5.2 for Windows®). Parents completed the Child Behaviour Checklist (CBCL), Conners’ Parent Rating Scale, and the Behaviour Rating Inventory of Executive Function (BRIEF).
In order to compare full-scale, verbal, and performance IQ scores of the Wechsler Intelligence Scale, these were converted to T-scores; the average score was set at 100, with scores below 70 considered to indicate poor intellectual functioning. We used scaled scores to analyse NEPSY II and Wechsler Intelligence Scale subtests; a score of 10 indicated average intellectual functioning and scores ≤ 7 indicated poor intellectual functioning. We set a typical score of 50 for the CBCL, Conners’ Parent Rating Scale, and BRIEF. CPT-II scores were expressed as percentiles, with 50 as the cut-off point.
Further data were gathered by administering a semistructured interview to parents, including questions about prenatal and perinatal medical history, acquisition of developmental milestones, general health, school performance, presence of disruptive behaviour, concerns about behaviours displayed in the family setting, and developmental progression. Parents also completed the CBCL, Conners’ Parent Rating Scale, and BRIEF.
Our study complies with the standards established by the research ethics committee of the Hospital Italiano de Buenos Aires and the Declaration of Helsinki of 1975, whose current, revised version can be accessed at http://www.wma.net/s/policy/b3.htm. Parents gave written informed consent, and children of sufficient age and understanding also expressed their consent to participate in the study.
ResultsWe included 24 patients with NF1; mean age was 9.88 years, and 58.33% (14) were boys. Parents expressed concerns about their children’s school performance and behaviour, reporting attention problems (58.33%), poor academic performance (25%), fine motor coordination disorders (25%), and language disorders (0.8%). One-third of parents reported 2 or more of the difficulties mentioned above, and 16.66% reported no problems.
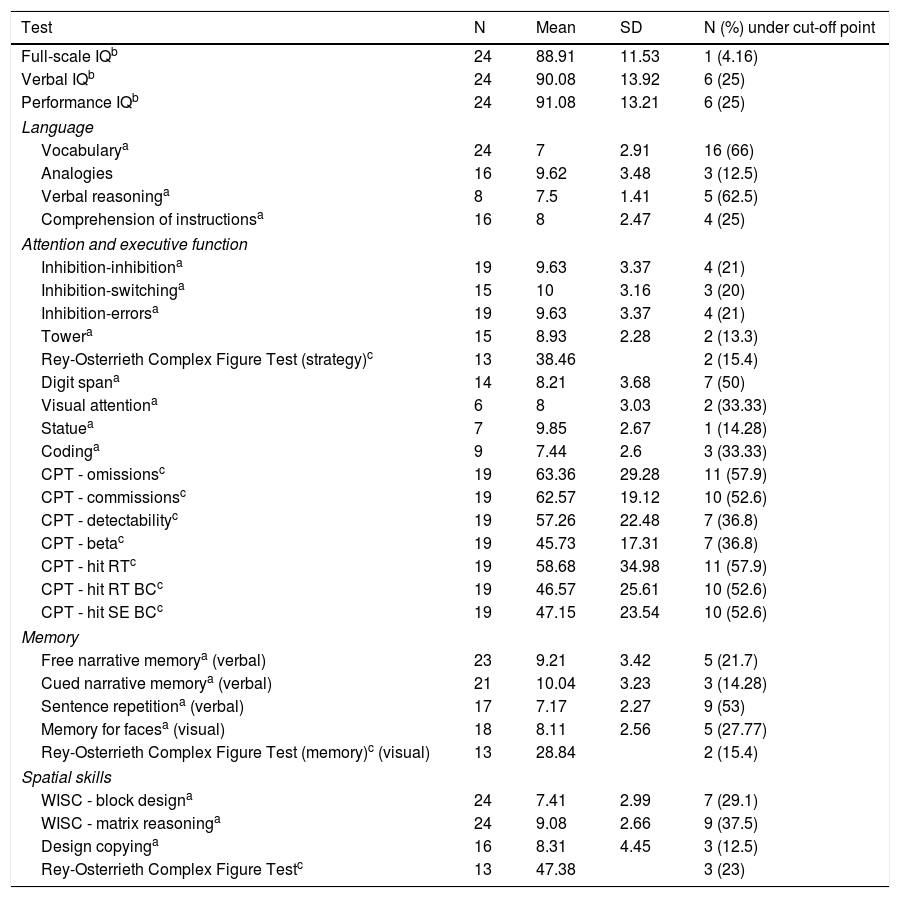
Mean full-scale, verbal, and performance IQ scores were normal. Although no discrepancies were seen between mean verbal and performance IQ scores, a considerable percentage of patients (37.50%) showed significant differences between the 2 (over 10 scaled points). One patient (4.16%) scored below 70 for full-scale IQ (Table 2).
Neuropsychological test scores.
| Test | N | Mean | SD | N (%) under cut-off point |
|---|---|---|---|---|
| Full-scale IQb | 24 | 88.91 | 11.53 | 1 (4.16) |
| Verbal IQb | 24 | 90.08 | 13.92 | 6 (25) |
| Performance IQb | 24 | 91.08 | 13.21 | 6 (25) |
| Language | ||||
| Vocabularya | 24 | 7 | 2.91 | 16 (66) |
| Analogies | 16 | 9.62 | 3.48 | 3 (12.5) |
| Verbal reasoninga | 8 | 7.5 | 1.41 | 5 (62.5) |
| Comprehension of instructionsa | 16 | 8 | 2.47 | 4 (25) |
| Attention and executive function | ||||
| Inhibition-inhibitiona | 19 | 9.63 | 3.37 | 4 (21) |
| Inhibition-switchinga | 15 | 10 | 3.16 | 3 (20) |
| Inhibition-errorsa | 19 | 9.63 | 3.37 | 4 (21) |
| Towera | 15 | 8.93 | 2.28 | 2 (13.3) |
| Rey-Osterrieth Complex Figure Test (strategy)c | 13 | 38.46 | 2 (15.4) | |
| Digit spana | 14 | 8.21 | 3.68 | 7 (50) |
| Visual attentiona | 6 | 8 | 3.03 | 2 (33.33) |
| Statuea | 7 | 9.85 | 2.67 | 1 (14.28) |
| Codinga | 9 | 7.44 | 2.6 | 3 (33.33) |
| CPT - omissionsc | 19 | 63.36 | 29.28 | 11 (57.9) |
| CPT - commissionsc | 19 | 62.57 | 19.12 | 10 (52.6) |
| CPT - detectabilityc | 19 | 57.26 | 22.48 | 7 (36.8) |
| CPT - betac | 19 | 45.73 | 17.31 | 7 (36.8) |
| CPT - hit RTc | 19 | 58.68 | 34.98 | 11 (57.9) |
| CPT - hit RT BCc | 19 | 46.57 | 25.61 | 10 (52.6) |
| CPT - hit SE BCc | 19 | 47.15 | 23.54 | 10 (52.6) |
| Memory | ||||
| Free narrative memorya (verbal) | 23 | 9.21 | 3.42 | 5 (21.7) |
| Cued narrative memorya (verbal) | 21 | 10.04 | 3.23 | 3 (14.28) |
| Sentence repetitiona (verbal) | 17 | 7.17 | 2.27 | 9 (53) |
| Memory for facesa (visual) | 18 | 8.11 | 2.56 | 5 (27.77) |
| Rey-Osterrieth Complex Figure Test (memory)c (visual) | 13 | 28.84 | 2 (15.4) | |
| Spatial skills | ||||
| WISC - block designa | 24 | 7.41 | 2.99 | 7 (29.1) |
| WISC - matrix reasoninga | 24 | 9.08 | 2.66 | 9 (37.5) |
| Design copyinga | 16 | 8.31 | 4.45 | 3 (12.5) |
| Rey-Osterrieth Complex Figure Testc | 13 | 47.38 | 3 (23) | |
CPT: Conners’ Continuous Performance Test II; Hit RT: hit reaction time; Hit RT BC: hit reaction time block change; Hit SE BC: hit standard error block change; SD: standard deviation.
Patients’ vocabulary and concept formation ability were below the population average. Five patients (20.83%) presented alterations at the phonological level of language, with phoneme omissions and substitutions.
Abstract reasoning from visual information was in line with the population average.
Fine motor coordination, evaluated with the block test, was affected in 29.1% of the sample (7/24) and in 26.08% of the patients with normal intellectual functioning (6/23).
Regarding executive function, we found no alterations in inhibition (evaluated with the NEPSY II inhibition subtest), planning (tower subtest), or strategy (Rey-Osterrieth Complex Figure Test). We observed difficulties in performing the digit span test in 50% of cases and in sentence repetition in 53% of cases, which reveals working memory impairment. In attention tests, especially the CPT-II, we observed an above-average number of omissions and commissions, as well as sustained attention deficits.
We also observed that 4.16% of patients met diagnostic criteria for intellectual disability, 33.33% for non-verbal learning disorder (NVLD), and 58.33% for ADHD. Thirty percent of patients with NF1 and ADHD had another neuropsychological disorder, with NVLD (21%) and expressive language disorder (8%) being the most frequent. Some 96% of patients experienced difficulties in at least one of the areas evaluated, 29.16% had some comorbidity, and only one patient (4%) achieved normal neuropsychological test scores.
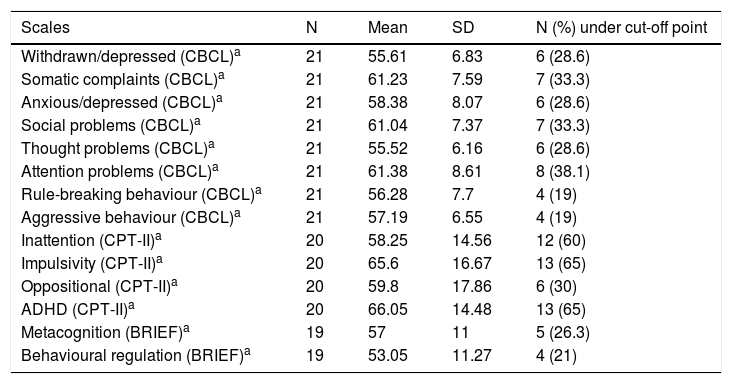
Tables 2 and 3 shows patients’ mean scores on the neuropsychological tests and scales administered.
Scale scores.
| Scales | N | Mean | SD | N (%) under cut-off point |
|---|---|---|---|---|
| Withdrawn/depressed (CBCL)a | 21 | 55.61 | 6.83 | 6 (28.6) |
| Somatic complaints (CBCL)a | 21 | 61.23 | 7.59 | 7 (33.3) |
| Anxious/depressed (CBCL)a | 21 | 58.38 | 8.07 | 6 (28.6) |
| Social problems (CBCL)a | 21 | 61.04 | 7.37 | 7 (33.3) |
| Thought problems (CBCL)a | 21 | 55.52 | 6.16 | 6 (28.6) |
| Attention problems (CBCL)a | 21 | 61.38 | 8.61 | 8 (38.1) |
| Rule-breaking behaviour (CBCL)a | 21 | 56.28 | 7.7 | 4 (19) |
| Aggressive behaviour (CBCL)a | 21 | 57.19 | 6.55 | 4 (19) |
| Inattention (CPT-II)a | 20 | 58.25 | 14.56 | 12 (60) |
| Impulsivity (CPT-II)a | 20 | 65.6 | 16.67 | 13 (65) |
| Oppositional (CPT-II)a | 20 | 59.8 | 17.86 | 6 (30) |
| ADHD (CPT-II)a | 20 | 66.05 | 14.48 | 13 (65) |
| Metacognition (BRIEF)a | 19 | 57 | 11 | 5 (26.3) |
| Behavioural regulation (BRIEF)a | 19 | 53.05 | 11.27 | 4 (21) |
BRIEF: Behaviour Rating Inventory of Executive Function; CBCL: Child Behaviour Checklist; CPT-II: Conners’ Continuous Performance Test II.
Parents generally had a good perception of their children’s attention disorders: the percentage of parents reporting attention difficulties coincides with that of children meeting diagnostic criteria for ADHD. The same is true for motor coordination disorders: poor motor coordination was reported by 25% of parents and detected in 26.08% of patients with normal intellectual functioning. However, parents tend to underestimate language difficulties; these were the reason for consultation in only 0.8% of cases, whereas 20.83% of patients in our sample presented language disorders.
According to the literature, the prevalence of intellectual disability is slightly higher in patients with NF1 than in the general population, although it is observed in a small percentage of patients (6%-8%).23–25 Global intellectual functioning in patients with NF1 is slightly below the population average.13 We observed significant differences between verbal and performance IQ scores in 37.50% of patients; this finding is consistent with previous studies.26 These differences are observed in both directions, with different patients scoring higher on one scale or the other.27 This is probably one of the reasons for the great variability of cognitive phenotypes in NF1, with verbal deficits observed in some cases and non-verbal deficits in others.28–30
According to the literature and our own results, prevalence estimates for ADHD in children with NF1 are more controversial.31,32 Although Hyman et al.12 report a lower incidence of ADHD (38.3%), they found that approximately 63% of children with NF1 have difficulties with sustained attention; this percentage is similar to that reported in our study. Interestingly, patients with NF1 did not show significant executive function difficulties. The difficulties observed in planning the response to complex stimuli were not explained by the presence of ADHD. These findings suggest that ADHD in NF1 may present with diverse clinical characteristics and may have a different neurocognitive basis to that of ADHD in patients without NF1.
Most studies report visuospatial and perceptive deficits, as in our sample. Fine motor deficits have been observed in the dominant upper limb.33 Despite these findings, few studies report NVLD in this population, perhaps due to underdiagnosis. This association should be kept in mind, given that one in every 3 patients in our sample had NVLD.
Regarding language skills, patients with NF1 had poorer vocabulary and concept formation ability.34 We found no deficits in verbal reasoning, ability to establish verbal analogies, or verbal memory. Our results highlight the need for neurolinguistic assessment of these patients, especially since language disorders are frequently underdetected by their parents.
Finally, it should be stressed that 96% of the patients displayed difficulties in at least one of the areas evaluated, 29.16% had some comorbidity, and only 4% achieved normal neuropsychological test scores. This suggests a high prevalence of neuropsychological disorders in patients with NF1; while parents do detect some difficulties, others are underestimated. Given the high frequency of cognitive disorders in patients with NF1, neurological assessment should include a neuropsychological evaluation, enabling early detection and treatment of cognitive disorders.
Author contributionsEVP, CP, ALB, and MJGB participated in the conception and design of the study.
ALB, MJGB, and FB conducted all psychometric tests.
ALB, MJGB, FB, EVP, and CP collected data.
EVP and CP performed the statistical analysis.
EVP, CP, RI, GA, and ALB interpreted the results.
EVP, ALB, and RI drafted the manuscript.
All authors reviewed the manuscript.
Conflicts of interestThe authors have no conflicts of interest to declare.
We wish to thank the Argentinian Association of Neurofibromatosis for their collaboration.
Please cite this article as: Vaucheret Paz E, López Ballent A, Puga C, García Basalo MJ, Baliarda F, Ekonen C, et al. Pacientes con neurofibromatosis tipo 1: perfil cognitivo y trastornos en funciones cerebrales superiores en la edad pediátrica. Neurología. 2019;34:353–359.
This study was presented at the Argentinian Congress of Paediatric Neurology.