Imaging diagnosis is essential for treatment planning in stroke patients. However, use of these techniques varies due to uncertainty about their effectiveness. Our purpose was to describe the use of CT and MRI in stroke and transient ischaemic attack (TIA) over 5 years in hospitals belonging to the Canary Islands Health Service and analyse interhospital variability based on routinely collected administrative data.
Patients and methodWe gathered the minimum basic dataset (MBDS) from patients diagnosed with stroke or TIA between 2005 and 2010 in 4 hospitals. Patients’ age, sex, procedures, secondary diagnoses, and duration of hospital stay were also recorded.
We conducted a descriptive analysis of patient characteristics and a bivariate analysis using the t test and the chi square test to detect differences between patients assessed and not assessed with MRI. Logistic regression was used to analyse unequal access to MRI.
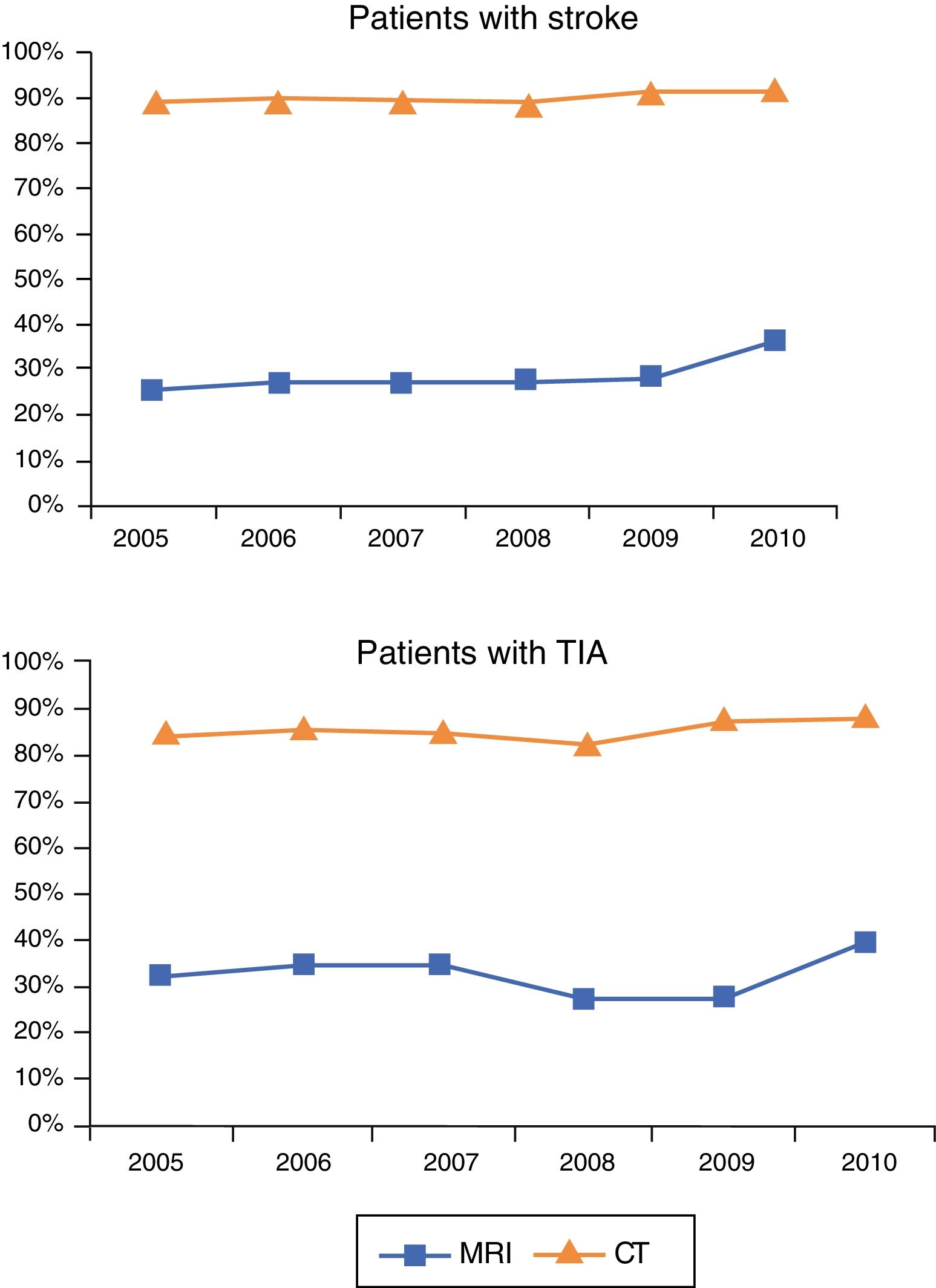
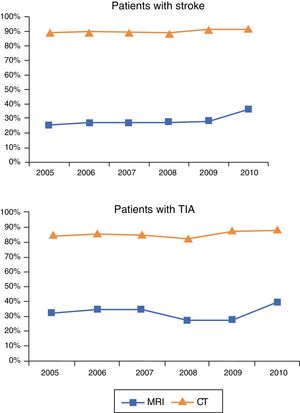
Results and conclusionsOur study included 10487 patients (8571 with stroke and 1916 with TIA). The percentage of stroke patients undergoing a CT scan increased from 89.47% in 2005 to 91.50% in 2010. In these patients, use of MRI also increased from 25.41% in 2005 to 36.02% in 2010. Among patients with TIA, use of CT increased from 84.64% to 88.04% and MRI from 32.53% to 39.13%. According to our results, female sex, younger age, and presence of comorbidities increase the likelihood of undergoing MRI.
El radiodiagnóstico es esencial para precisar la planificación terapéutica de las personas con ictus, pero la incertidumbre sobre su efectividad puede contribuir a la variabilidad en su indicación. Este estudio tiene por objetivo describir la evolución del uso de TAC y RM en el manejo del ictus a lo largo de 5 años en la red hospitalaria del Servicio Canario de Salud y analizar la variabilidad interhospitalaria mediante el uso de datos administrativos recogidos rutinariamente.
Pacientes y métodoSe explotó el CMBD de los pacientes con diagnóstico de ictus o AIT (2005-2010) en 4 hospitales. Además, se incluyó la edad y el sexo del paciente, los procedimientos realizados, los diagnósticos secundarios y la estancia.
Se realizó un análisis descriptivo de las características de los pacientes y un análisis bivariante mediante t de Student o Chi-cuadrado para detectar diferencias entre los pacientes según recibieran o no RM. Las desigualdades en el acceso a RM se analizaron mediante regresión logística.
Resultados y conclusionesSe incluyeron 10.487 pacientes adultos (8.571 con ictus y 1.916 con AIT). El porcentaje de pacientes con ictus que recibieron TAC aumentó desde el 89,47% en 2005 al 91,50% en 2010; en ellos, la RM aumentó desde el 25,41% en 2005 al 36,02% en 2010. Entre los pacientes con AIT el uso de TAC creció desde el 84,64 al 88,04%, y el de RM, desde el 32,53 al 39,13%. Nuestros resultados sugieren que ser mujer, joven y presentar mayor comorbilidad aumentan las probabilidades de recibir RM.
Stroke continues to be the second leading cause of death in developed countries, despite progressive decreases over the past 20 years.1 Due to its high incidence; its impact on morbidity, mortality, and quality of life; and the healthcare costs associated with loss of independence, the socioeconomic cost of stroke in Spain is estimated at €2.5 billion per year.2,3 This justifies the need for efficient, cost-effective procedures for the prevention, early diagnosis, and treatment of stroke.4 Imaging techniques are essential for diagnosis and for predicting medium- to long-term treatment response. Clinical guidelines on stroke management stress the usefulness of CT and MRI in diagnosis and follow-up.5,6
Despite evidence on the cost-effectiveness of immediate CT scanning in patients with suspected stroke,7 MRI has been found to have similar sensitivity for detecting acute bleeding and higher sensitivity for distinguishing chronic haemorrhages.6,8 MRI appears to be more precise than CT for diagnosing acute ischaemia and has similar validity for detecting intracerebral haemorrhage.9 MRI also has higher sensitivity for detecting subtle haemorrhagic changes,10 localising the lesion,11 and determining the aetiopathogenic mechanism of stroke.12,13 However, there is no conclusive evidence that the advantages of MRI lead to substantial differences in stroke management or outcomes.14,15
This study describes the use of CT and MRI in the management of ischaemic stroke and transient ischaemic attack (TIA) between 2005 and 2010 in hospitals of the Canarian Health Service and aims to analyse any variations between hospitals using routine administrative data. We also aimed to identify profiles of patients with reduced access to neuroimaging techniques.
Patients and methodsWe used the minimum basic dataset (MBDS) system to collect demographic data and information on hospital activity, such as main diagnosis at admission, relevant risk factors, comorbidities and complications during hospitalisation, diagnostic techniques, and relevant treatment interventions. The MBDS also provides the date and the circumstances surrounding admission and discharge. Diagnoses and procedures are coded according to the ninth revision of the International Classification of Diseases (ICD-9).16
We used the MBDS to gather data on patients hospitalised with a main diagnosis of ischaemic stroke or TIA between 1 January 2005 and 31 December 2010 at the 4 reference hospitals of the Canarian Health Service (referred to in this article as A, B, C, and D). We used the following ICD-9 codes for diagnosis: 434.00, 434.01, 434.10, 434.11, 434.90, and 434.91 for ischaemic stroke and 435.0, 435.1, 435.2, 435.3 435.8, and 435.9 for TIA. In addition to the main diagnosis at admission, we recorded the year of admission, hospital, age, sex, circumstances of discharge and hospital department discharging the patient, procedures performed, secondary diagnoses (which were used to calculate the Charlson Comorbidity Index [CCI]), and hospitalisation time. We excluded the patients who had a stroke or TIA during hospitalisation for other conditions as we were unable to determine whether CT/MRI scans were performed for stroke diagnosis or for assessing other conditions. Data were stored in Microsoft Access and managed and analysed with SPSS v. 12 and Microsoft Excel.
CT and MRI studies were described with ICD-9 codes 87.03 (head CT) and 88.91 (brain and brainstem MRI). We performed a descriptive analysis of patient characteristics using frequencies and percentages for categorical variables and means and standard deviations (SD) for quantitative variables. We also conducted a bivariate analysis applying hypothesis testing (t test or chi-square test) to detect any differences between the characteristics of patients who did and did not undergo MRI.
We analysed potential inequalities in access to MRI with logistic regression to determine the likelihood of a patient with stroke/TIA undergoing an MRI study as a function of the variables analysed (age, sex, CCI, and whether the patient had previously undergone a CT scan). CCI was calculated using data on secondary diagnoses and risk factors.17 The regression model used the Wald statistic to exclude non-significant variables; we calculated the odds ratio for each variable in the model.
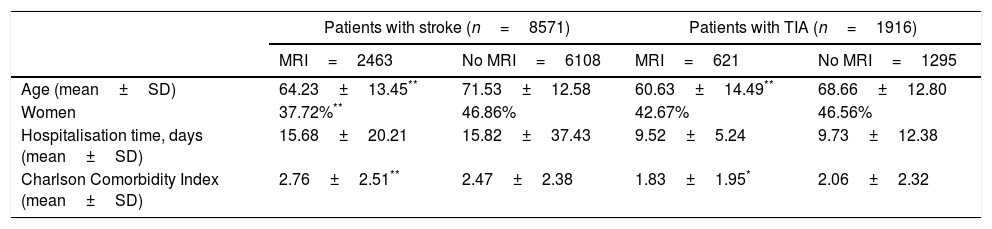
ResultsThe study included 10487 patients older than 18. Table 1 summarises patient characteristics, grouping patients according to whether or not they underwent MRI.
Demographic characteristics and comorbidities of patients with stroke and TIA, grouped according to whether or not they underwent MRI in the reference hospitals of the Canarian Health Service (2005-2010).
| Patients with stroke (n=8571) | Patients with TIA (n=1916) | |||
|---|---|---|---|---|
| MRI=2463 | No MRI=6108 | MRI=621 | No MRI=1295 | |
| Age (mean±SD) | 64.23±13.45** | 71.53±12.58 | 60.63±14.49** | 68.66±12.80 |
| Women | 37.72%** | 46.86% | 42.67% | 46.56% |
| Hospitalisation time, days (mean±SD) | 15.68±20.21 | 15.82±37.43 | 9.52±5.24 | 9.73±12.38 |
| Charlson Comorbidity Index (mean±SD) | 2.76±2.51** | 2.47±2.38 | 1.83±1.95* | 2.06±2.32 |
Overall use of neuroimaging techniques increased progressively over the study period, both among patients with stroke and among those with TIA, due to the increase in the number of admissions due to stroke and TIA. CT scans were performed in 90.4% of patients undergoing MRI. The percentage of stroke patients undergoing CT increased from 89.47% in 2005 to 91.50% in 2010. MRI use increased more markedly than CT use; it should be stressed, however, that MRI was initially used less frequently than CT. In patients with stroke, MRI use increased from 25.41% in 2005 to 36.02% in 2010. Among patients with TIA, CT use increased from 84.64% to 88.04% and MRI use from 32.53% to 39.13% (Fig. 1).
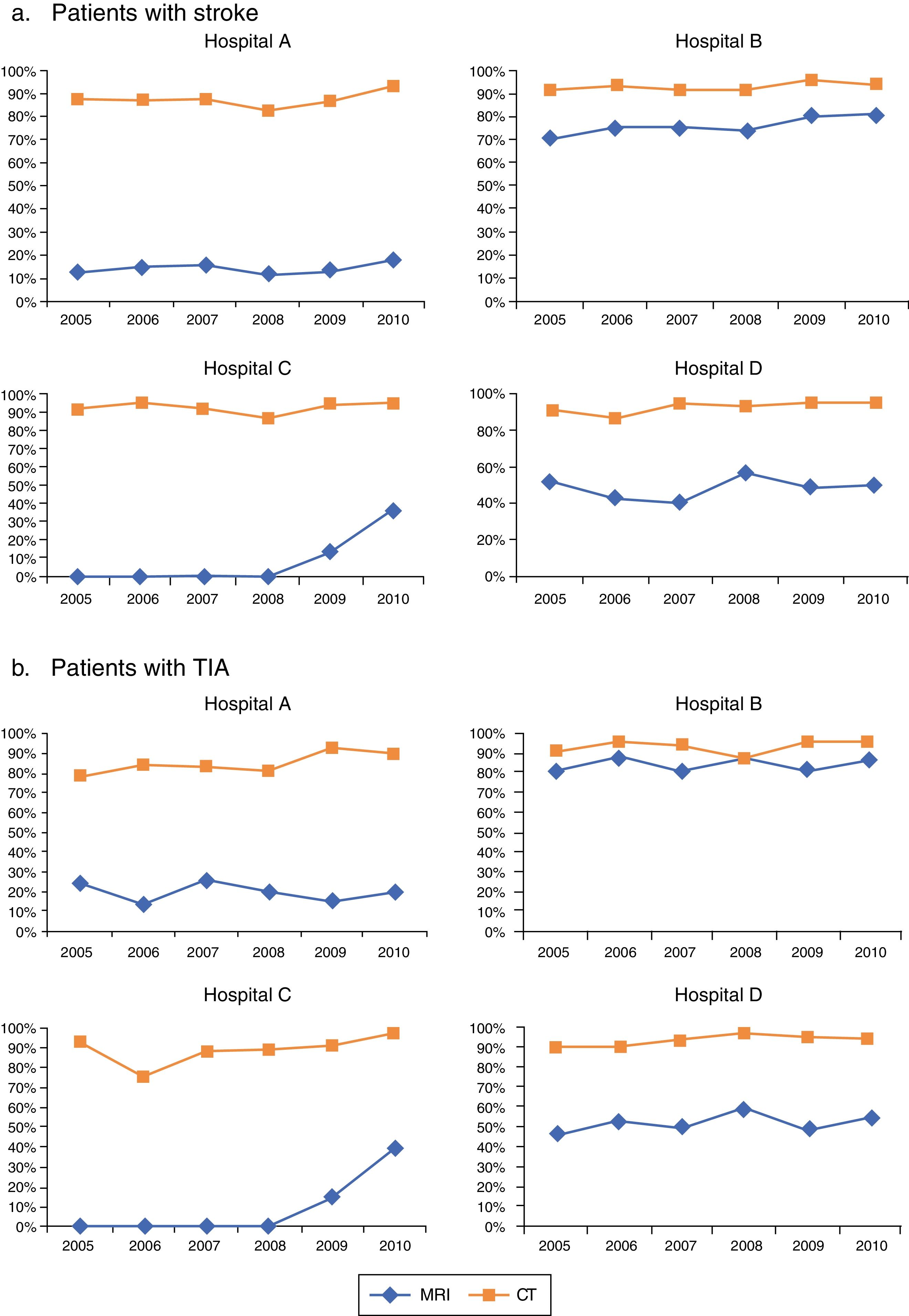
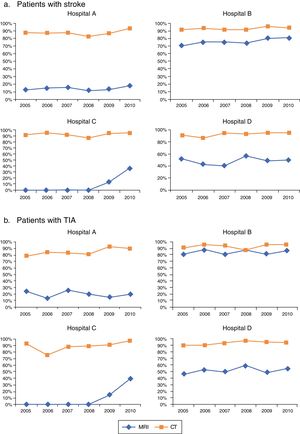
CT use increased in all hospitals, both in patients with stroke and in those with TIA; CT was more frequently used than MRI in all cases. CT was used less frequently for both conditions in hospital A than in the other 3 hospitals. A similar but greater effect was observed for MRI studies: at the end of the study period, the technique was used in 17.38% of stroke patients in hospital A, in 37.11% in hospital C, in 50.37% in hospital D, and in 81.07% in hospital B. The level of MRI use in patients with TIA was similar to that observed for stroke patients for each hospital in 2010: 18.97% in hospital A, 40% in hospital C, 54.39% in hospital D, and 86.49% in hospital B. MRI use follows 4 distinct patterns depending on the hospital: low use, medium use, high use, and a dynamic pattern showing an increase from lack of use to medium use in the last 2 years of the study period (Fig. 2).
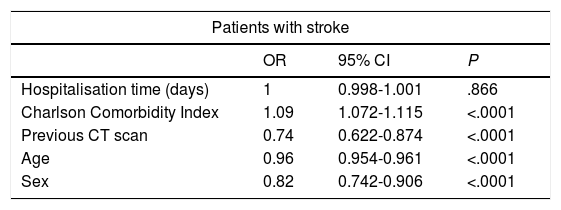
Among patients with stroke, a previous CT scan, age, and sex, but not hospitalisation time (P=.866), have an impact on the likelihood of undergoing MRI, according to the logistic regression analysis (Table 2). Higher CCI increases the likelihood of undergoing MRI by 9% (OR=1.09; P<.0001). The likelihood of undergoing MRI decreases with older age (OR=0.96; P<.0001). Men are 18% less likely to undergo MRI (OR=0.82; P<.0001). Having undergone a previous CT scan during the same hospital stay also reduces the likelihood of undergoing MRI by 26% (OR=0.74; P<.0001).
Multiple logistic regression analysis of the likelihood of patients with stroke or TIA undergoing MRI at hospitals in the Canarian Health Service (2005-2010).
| Patients with stroke | |||
|---|---|---|---|
| OR | 95% CI | P | |
| Hospitalisation time (days) | 1 | 0.998-1.001 | .866 |
| Charlson Comorbidity Index | 1.09 | 1.072-1.115 | <.0001 |
| Previous CT scan | 0.74 | 0.622-0.874 | <.0001 |
| Age | 0.96 | 0.954-0.961 | <.0001 |
| Sex | 0.82 | 0.742-0.906 | <.0001 |
| Patients with TIA | |||
|---|---|---|---|
| OR | 95% CI | P | |
| Hospitalisation time (days) | 1 | 0.998-1.001 | .866 |
| Charlson Comorbidity Index | 1.09 | 1.072-1.115 | <.0001 |
| Previous CT scan | 0.74 | 0.622-0.874 | <.0001 |
| Age | 0.96 | 0.954-0.961 | <.0001 |
| Sex | 0.82 | 0.742-0.906 | <.0001 |
Results are different for patients with TIA: no statistically significant differences were observed for the variables CCI (P=.136), previous CT scan (P=.110), sex (P=.348), or hospitalisation time (P=.843). However, the likelihood of undergoing MRI decreased by 4% with older age (OR=0.956; P<.0001). Table 2 summarises the results of the multiple logistic regression analysis.
DiscussionAlthough clinical practice guidelines5,18–20 recommend immediate neuroimaging assessment for the diagnosis and treatment of stroke, the percentage of patients undergoing neuroimaging studies does not reach 100% either in the Canarian Health Service or in other developed countries.9,21 Lazzarino et al.21 suggest that the increase in the use of neuroimaging techniques may not be real, but rather the result of improvements in the coding of diagnostic tests in the MBDS, which may have contributed to the interhospital differences observed.
Our study provides information on the use of neuroimaging techniques in patients with stroke and TIA. Whereas our rates of CT use in stroke and TIA are similar to those reported for the United Kingdom (83.4%) and the United States (95%), rates of MRI use in the Canarian Health Service do not reach those of the United States for stroke (50%) or Norway for TIA (89%).9,22
In the United States, 95% of stroke patients undergoing MRI also underwent at least one CT scan. In the Canarian Health Service, however, the percentage is lower (90.4%). These findings confirm that MRI has not replaced CT as the main diagnostic tool for stroke/TIA; rather, multiple neuroimaging techniques are being introduced in clinical practice,9 which is increasing healthcare costs15 but providing no clear benefits.21 Pronounced differences in MRI use were observed between hospitals of the Canarian Health Service; rates of MRI use within hospitals were similar for stroke and for TIA. This points to the involvement of factors other than styles of clinical practice, such as the accessibility of MRI technology. In order for a technique to be used, it must be available, accessible, and well established.23,24 Although hospitals in the Canarian Health Service are comparable in terms of assigned population, human resources, and equipment, there are differences in the number of MRI scanners available and the date of purchase. The hospital showing high MRI use was the first to incorporate MRI (in 1997); during the study period, it had the most MRI scanners available. The hospital showing low MRI use had only one MRI scanner, purchased in 1999; in this hospital, MRI studies were performed preferentially in patients selected according to CT results. The hospital showing medium MRI use had also had a single MRI scanner since 2005, but eligibility criteria appear to have been less strict. The dynamic pattern of MRI use observed in the remaining hospital may be explained by the purchase of an MRI scanner in early 2007. Although they do not describe use patterns, Burke et al.9 observe considerable variations in the use of MRI in stroke patients between hospitals in 10 US states from 1999 to 2008 (ranging from 55% in Oregon to 79% in Arizona); however, they provide no explanation for this phenomenon.
Other authors suggest that certain patient characteristics may have an impact on physicians’ decisions about whether to perform a CT/MRI study.21 Our results suggest that female sex, younger age, and presence of comorbidities increase the likelihood of being assessed with MRI. Though limited, the effect of sex is striking: studies on sex-related healthcare inequalities suggest that healthcare resources are more accessible to women than to men, even when need is equal.21,25
The impact of differing clinical practice styles on these variations may be explained by uncertainty regarding the use of CT and MRI for stroke during the period 2005-2010.5,26 Recent clinical practice guidelines for acute ischaemic stroke recommend MRI for stroke assessment,27 whereas the American Academy of Neurology (AAN) limits this recommendation to the first 12hours after symptom onset.28 The AAN recommendations cannot explain our results as they were published before the first year of our study period.
Burke et al.9 note the possibility that requesting both CT and MRI may be due to the physician's preference for MRI in a context where CT is performed faster. In this scenario, it may be possible to improve efficiency in the indication of MRI by optimising patient selection (identifying patients who can wait for an MRI study without a substantial increase in risk) and by improving the dissemination of consensus protocols on the most suitable order for performing the studies.
Our study is not without limitations. The MBDS does not provide information on criteria explaining the indication for specific diagnostic tests, or when each test was indicated and performed; this limits our ability to interpret the results. The study focuses on one region of Spain; caution should therefore be exercised when extrapolating the results to other regions.
Our study has a number of strengths. It supports previous reports of a lack of adherence to clinical practice guidelines, since it describes interhospital differences and inequalities in indicating neuroimaging studies. Our study also demonstrates the usefulness of recording and analysing routine data from clinical practice for detecting clinical changes.
In conclusion, analysis of these data shows that the use of MRI in stroke and TIA management has increased substantially in the hospitals of the Canarian Health Service, although with considerable differences. These results have ethical, clinical, and economic implications; 90.4% of patients admitted due to stroke or TIA and undergoing MRI had previously been evaluated with CT. Assessment with both CT and MRI increases healthcare expenses with no clear clinical benefit.
FundingThis study was conducted as part of the collaboration agreement between the Institute of Health Carlos III and the Canarian Foundation for Healthcare Research in the context of the activities conducted by the Spanish Network of Agencies for Assessing National Health System Technologies and Performance, funded by the Spanish Ministry of Health, Social Services, and Equality.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Valcárcel-Nazco C, Alonso-Modino D, Montón-Álvarez F, Sabatel-Hernández R, Pastor-Santoveña MS, Mesa-Blanco P, et al. Grandes variaciones en la utilización de pruebas por imagen en el diagnóstico y seguimiento de los pacientes con ictus. Neurología. 2019;34:360–366.