Collet-Sicard syndrome (CSS) is defined as unilateral palsy of lower cranial nerves ix, x, xi, and xii. In 1915, Frederic Collet initially described this syndrome in a soldier who had been shot during World War I,1 and some time later, Jean A. Sicard provided additional descriptions.2 CSS is a very rare condition resulting from lesions at the base of the skull that affect both the jugular foramen and hypoglossal canal. There are a number of causes, including tumours (primary or metastatic), trauma, vascular lesions, inflammatory processes, and iatrogenic complications. Invasive metastatic processes, basilar skull fractures, and carotid artery dissection are the most common aetiologies according to previously published studies, whereas primary intracranial tumours are an extremely rare cause of CSS. We describe a case in which CSS presented as a primary intracranial tumour in the jugular foramen, as well as a review of the aetiology of this syndrome.
Clinical caseWe present the case of an 81-year-old woman with a history of well-controlled arterial hypertension and acoustic neurinoma in the right internal auditory canal. She visited the otorhinolaryngology department for follow-up, and that department referred her to neurology after identifying paresis of the left vocal cord and atrophy of the left side of the tongue.
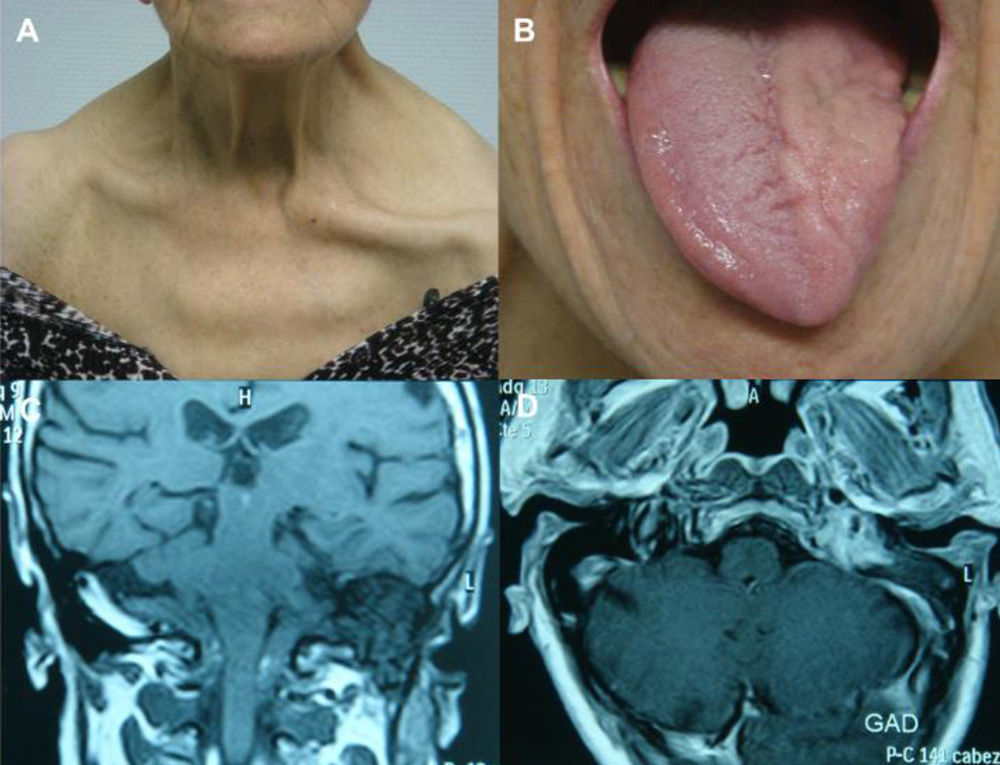
During the year before her neurology consultation, the patient had experienced hypogeusia. After 6 months, she gradually developed dysphagia for both solids and liquids, diminished vocal tone, and weakness in the left shoulder. Symptoms worsened slowly and progressively. Neurological examination showed left-sided drooping of the soft palate, absent gag reflex, whispering speech, and atrophy of the left side of the tongue with no fasciculations. There was also palsy and pronounced atrophy of the left trapezius and sternocleidomastoid muscles, resulting in drooping of the left shoulder and ipsilateral clavicle protrusion (Fig. 1A and B). The neurological examination yielded normal results for all other areas. Cranial magnetic resonance imaging (MRI) revealed a tumour measuring 2.5cm×2cm in the internal jugular foramen, hypointense in T1-weighted and isointense in T2-weighted images, and extending caudally along the path of the internal jugular vein. Tumour intensity increased significantly with gadolinium contrast (Fig. 1C and D). MRI also revealed a lesion occupying the right internal auditory canal, compatible with acoustic neurinoma. The suspected diagnosis was glomus jugulare tumour or jugular foramen neurinoma. We requested a neurosurgical evaluation in order to determine the best treatment approach. Given the patient's advanced age, surgical resection was ruled out. Since we opted for treatment with stereotactic radiosurgery, no anatomical pathology diagnosis of the lesion is available. After 5 years of follow-up, CSS has not yet resolved. Dysphagia has improved slightly, but the rest of the clinical findings remain the same. The follow-up cranial MRI shows a discrete reduction in tumour size (2cm×1.4cm).
Collet-Sicard syndrome: (A) left cranial nerve xi palsy resulting in drooping of the shoulder and clavicle protrusion; (B) left cranial nerve xii palsy leading to atrophy of the left side of the tongue; (C) tumour located in the left internal jugular foramen; and (D) gadolinium-enhancing lesion in MRI.
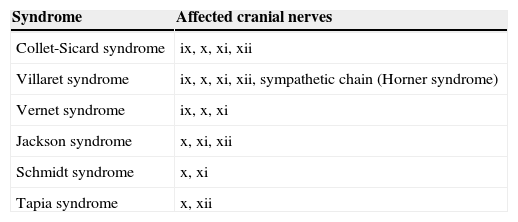
CSS, which was first described by Collet and Sicard working separately, is a rare condition involving combined and unilateral palsy of cranial nerves ix, x, xi, and xii. This syndrome usually develops gradually and its clinical presentation may be complex, which is why late diagnosis is not infrequent. Sometimes it presents in an incomplete form, resulting in other types of syndromes known as jugular foramen syndromes (Table 1). When CSS appears in association with ipsilateral Horner syndrome, this is called Villaret syndrome.
Diagnosis of CSS can be based on clinical history, physical examination, and detailed description of the lesions provided by neuroimaging.3 Occasionally, as in our case, it may be difficult to describe tumours located in the jugular foramen. Gadolinium-enhanced MRI is the technique of choice for determining tumour size and anatomical connections. However, an anatomical pathology study is necessary for a definitive diagnosis.4
CSS can be provoked by a number of conditions, for example, invasive processes at the base of the skull (primary or metastatic tumours), trauma, vascular lesions, inflammatory processes, and iatrogenic complications. Our patient showed clinical findings compatible with CSS secondary to a primary tumour in the jugular foramen, possibly related to the presence of a neurinoma or a glomus jugulare tumour. Neurinomas are slow-growing benign tumours that may rarely undergo malignant transformation. The most frequently affected cranial nerve is cranial nerve viii, followed by cranial nerves v, ix, x, and xi. Purely motor cranial nerves are less frequently affected.5 Glomus tumours, or paragangliomas, are highly vascularised tumours composed of cells that originate from the neural crest during embryonic development. While 90% of the paragangliomas arise in the adrenal glands, only 3% develop in the head and neck.6 These tumours grow close to the jugular foramen and may extend into the intracranial and extracranial spaces. Surgical resection is the treatment of choice for neurinomas and paragangliomas. However, stereotactic radiosurgery is the main treatment alternative for elderly patients, those in poor clinical condition, or patients presenting residual or recurrent lesions after surgery.7,8
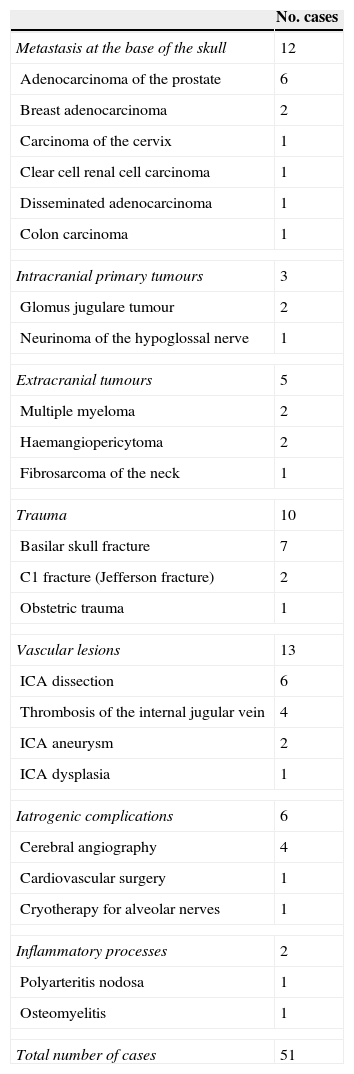
A search for the literature on CSS available in PubMed yielded a total of 51 cases published between 1915 and 2012. Table 2 summarises the different aetiologies of CSS. Out of all tumour-related processes at the base of the skull which can cause this syndrome, metastasis was the most frequent aetiology. We found only three cases of CSS secondary to a primary tumour at the base of the skull: two cases secondary to glomus jugulare tumour,9,10 and one case secondary to a neurinoma of the hypoglossal nerve.11
Aetiologies of Collet-Sicard syndrome
| No. cases | |
|---|---|
| Metastasis at the base of the skull | 12 |
| Adenocarcinoma of the prostate | 6 |
| Breast adenocarcinoma | 2 |
| Carcinoma of the cervix | 1 |
| Clear cell renal cell carcinoma | 1 |
| Disseminated adenocarcinoma | 1 |
| Colon carcinoma | 1 |
| Intracranial primary tumours | 3 |
| Glomus jugulare tumour | 2 |
| Neurinoma of the hypoglossal nerve | 1 |
| Extracranial tumours | 5 |
| Multiple myeloma | 2 |
| Haemangiopericytoma | 2 |
| Fibrosarcoma of the neck | 1 |
| Trauma | 10 |
| Basilar skull fracture | 7 |
| C1 fracture (Jefferson fracture) | 2 |
| Obstetric trauma | 1 |
| Vascular lesions | 13 |
| ICA dissection | 6 |
| Thrombosis of the internal jugular vein | 4 |
| ICA aneurysm | 2 |
| ICA dysplasia | 1 |
| Iatrogenic complications | 6 |
| Cerebral angiography | 4 |
| Cardiovascular surgery | 1 |
| Cryotherapy for alveolar nerves | 1 |
| Inflammatory processes | 2 |
| Polyarteritis nodosa | 1 |
| Osteomyelitis | 1 |
| Total number of cases | 51 |
ICA: internal carotid artery.
In conclusion, although primary tumours at the base of the skull rarely cause CSS, they must be considered in the differential diagnosis of this entity.
Please cite this article as: Gutiérrez Ríos R, Castrillo Sanz A, Gil Polo C, Zamora García MI, Morollón Sánchez-Mateos N, Mendoza Rodríguez A. Síndrome de Collet–Sicard. Neurología. 2015;30:130–2.