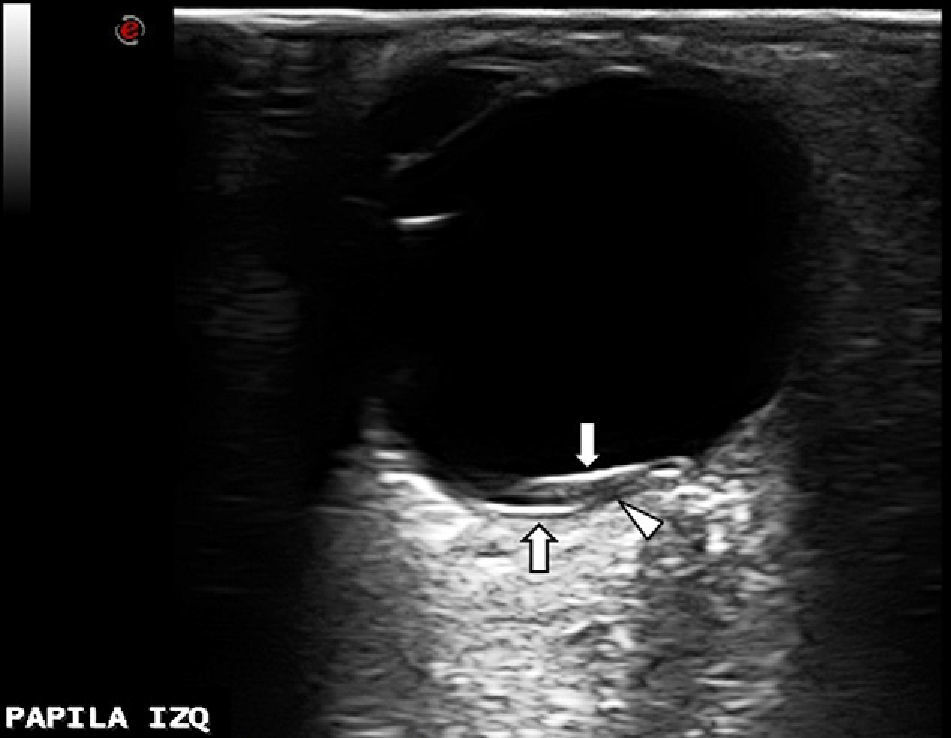
We have read with interest the article by Sánchez Ferreiro et al.1 regarding Terson syndrome (TS) and its potentially important role as a prognostic marker for subarachnoid haemorrhage (SAH). However, we cannot agree with all the points highlighted by the authors. Visible haemorrhages in the fundus of the eye are not a rare occurrence in SAH patients, and while haemorrhages have been suggested as indicators of poor prognosis, not all authors accept this premise.2 Furthermore, the article by Sánchez Ferreiro et al. states that most SAH patients with associated TS present a low level of consciousness. However, our experience contrasts with this statement. As an example, we present the case of a 49-year-old man attended in our hospital on the same day we read the Letter to the Editor. The patient had suffered subarachnoid bleeding during the night while engaging in sexual intercourse. Presence of aneurysm of the anterior communicating artery was observed using CT angiography. His SAH was classified as Fisher grade 3 and Hunt & Hess grade II: stuporous condition was not observed in the patient at any time during the first days of bleeding, and there were no neurological signs except for intense headache and neck rigidity. Twenty-four hours after symptom onset, the patient underwent successful embolisation with platinum coils resulting in total aneurysm occlusion. Five days after embolisation, funduscopic examination revealed several subhyaloid and retinal haemorrhages (a larger one on the superior-nasal quadrant adjoining the optic disk) not affecting the macular area in the left eye. In the right eye, we observed macular and peripapillary retinal haemorrhages. The ocular ultrasound performed that same day revealed the intraretinal origin of the largest haemorrhage, which was located on the superior nasal quadrant of the left eye. On the ultrasound image (Fig. 1), we can observe that the anechogenic area (corresponding to the bleeding and indicated by an arrowhead) divides the retinal lamina (hyperechogenic on the figure, indicated by 2 arrows).
Therefore, in our case, presence of TS in an SAH patient was not associated with stupor or coma, contrary to the rule suggested by Sánchez Ferreiro et al. In fact, we believe that TS in cases of SAH is sufficiently frequent (although underdiagnosed) that it can be clearly associated with any possible outcome.
Although TS as initially described referred only to vitreous haemorrhages in association with SAH, vitreous, subhyaloid, intraretinal, and subretinal haemorrhages are included in this term as it is currently understood.3 However, TS pathophysiology remains unknown, as Sánchez Ferreiro et al. explain in their article. Presence of intraocular haemorrhages might be explained by the pressure exerted by the haematoma on periocular structures, thus favouring the flow of blood through the optic nerve sheath across the subarachnoid space.4,5 Another theory suggests that TS could be associated with increased intracranial pressure (ICP) secondary to SAH. Venous hypertension caused by ICP might cause rupture of retinal veins, thereby giving rise to ocular haematoma.6 If this theory was right, poor prognosis in these patients would have more to do with ICP than with intraocular haemorrhage, and TS would be considered an epiphenomenon.
Lastly, we would like to highlight the utility of orbital Doppler sonography in TS diagnosis,6,7 since this is a simple, fast, and noninvasive technique available to neurologists. This test not only enables diagnosis of TS but also can be used to identify the exact nature of the type of haemorrhage and any potential complications such as retinal detachment, which are therapeutically relevant points.6
Please cite this article as: Monteagudo M, Doménech C, Segura T. Síndrome de Terson y ecografía orbitaria. Neurología. 2015;30:132–3.