Delayed-onset encephalopathy secondary to carbon monoxide poisoning (CO) is a serious although infrequent complication that manifests within the first and the sixth week after poisoning. Its main symptoms are cognitive impairment, parkinsonism, ataxia, and/or behavioural disorder.1–3
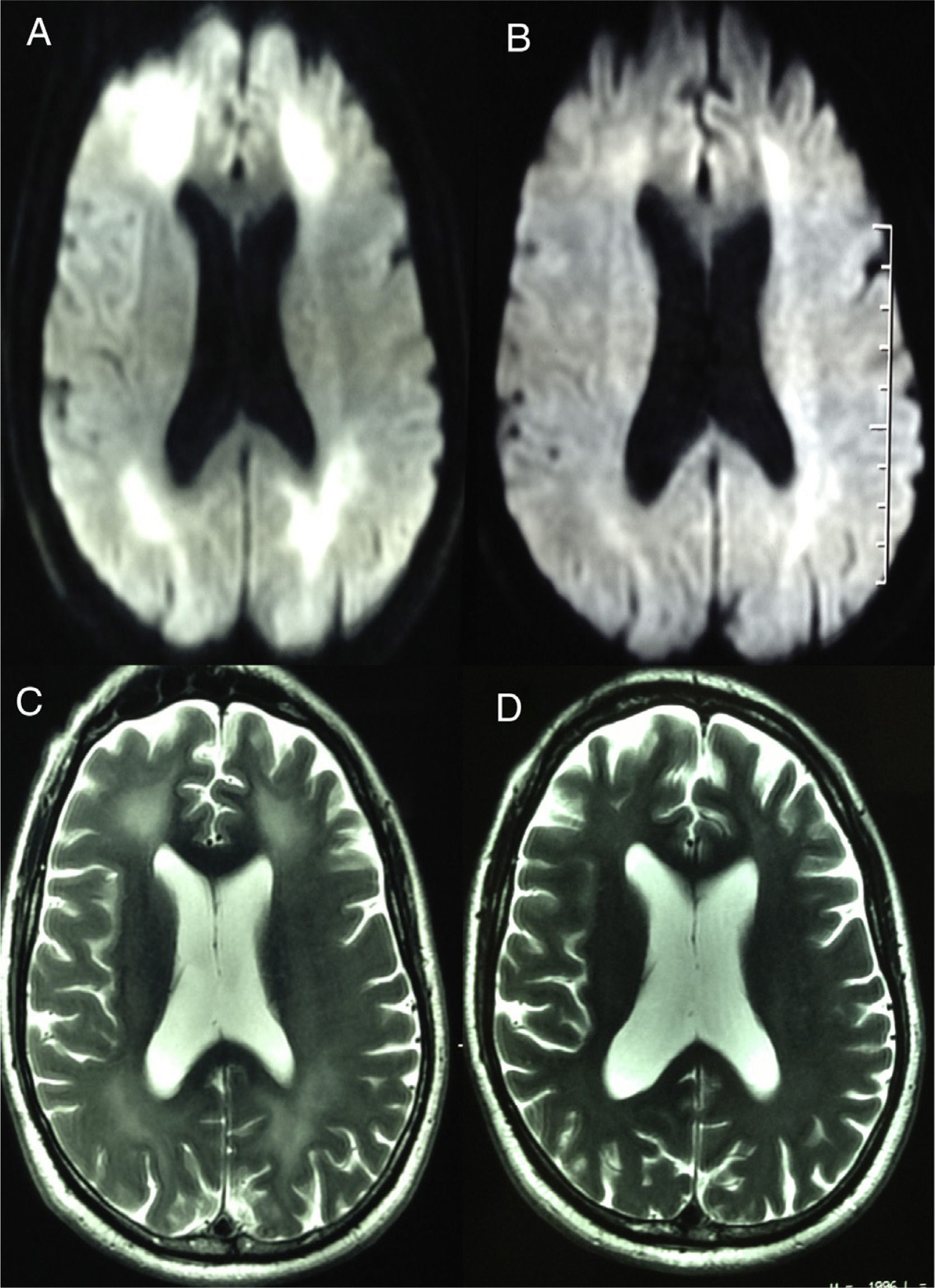
We report the case of a patient who presented this entity, which is characterised by pronounced cognitive impairment. The patient's outcome was favourable. Our patient is a 52-year-old man (a right-handed married freelance worker) with a long history of alcohol and tobacco dependence. On 16 September 2012, after having consumed alcohol, the patient fell asleep near a lit heater and was exposed to carbon monoxide for 14hours. He was admitted to a provincial hospital due to confusional state; after 24hours in observation without hyperbaric oxygen treatment, he was discharged with no neurological disorders. The patient returned to work with no incidents for the following 30 days. After that initial month, his wife noticed changes in his behaviour: he was apathetic, disoriented, confused, and had difficulty completing professional and other daily tasks. He was readmitted to the local hospital, and a brain CT performed at that time yielded normal results. General examinations ruled out infectious or vascular aetiology, and the patient was transferred to our centre to complete the study. At 53 days after symptom onset, the patient was admitted to our hospital awake, showing disorientation, labile attention, and significant impairment of executive functions. He demonstrated altered function when performing the Luria test (fist, edge, and palm) with signs of frontal release and compromised episodic memory, but with preserved long-term memory. Constructional apraxia was confirmed and he scored only 2 points on the clock-drawing test. The patient's score on the Mini-Mental State Examination (MMSE) was 19/30 and his score on Addenbrooke's Cognitive Examination (ACE) was 61/100. The examination detected no focal signs, myoclonias, or movement disorders. All laboratory analyses showed normal results, and the VDRL and HIV tests were both negative. Cytological and chemical studies of cerebrospinal fluid (CSF) yielded normal findings. Electroencephalography (EEG) showed normal alpha rhythm with bilateral, polymorphic, and intermittent theta wave activity. Brain magnetic resonance imaging (MRI) revealed T2-weighted and FLAIR signal intensity, as well as bilaterally symmetric restricted diffusion which was partially confluent in the periventricular white matter. These findings were more noticeable in the frontal and parietal areas even without gadolinium contrast (Fig. 1A–C). The possible diagnosis of dementia-like symptoms due to delayed encephalopathy secondary to CO poisoning was confirmed based on similar images in the literature.3,4 Considering the time elapsed since poisoning and in absence of a specific treatment, doctors began a therapeutic trial with citicoline at 1g/day.5 Sixty days later (in January 2013), the patient underwent another neuropsychological evaluation. His overall improvement was significant; specifically, his score on the MMSE was 27/30, and his score on the ACE had increased to 86/100. EEG showed disappearance of slow wave activity. Brain MRI showed a significantly decreased white matter compromise, especially on the diffusion sequence (Fig. 1B). The patient resumed working normally, and his last assessment at 10 months after acute intoxication (July 2013) showed him to be asymptomatic. His scores on the MMSE and ACE were 29/30 and 91/100, respectively. A routine MRI showed total remission of lesions in the white matter (Fig. 1D). Delayed-onset encephalopathy caused by carbon monoxide poisoning is a condition that progresses unfavourably in approximately half of the cases. Symptoms include cognitive and behavioural sequelae, and movement disorders.1,2 Prognosis is less favourable in elderly patients or those with shorter lucid intervals (defined as the latency period between acute poisoning and the onset of neuropsychological symptoms).1,2 The main pathophysiological cause is believed to be diffuse demyelination of the subcortical white matter, generally associated with neuronal damage to basal ganglia. MRI studies correspond to the lesions described in the literature, and sequential studies have been helpful in furthering knowledge of this syndrome. A constant feature in MRI is hyperintensity in subcortical white matter and globus pallidus, as seen on diffusion, FLAIR, and T2-weighted sequences.3,4 Diffusion-weighted sequences have shown slow and progressive development of cellular oedema as a result of neuronal death and delayed demyelination.4 Presence of changes in the FLAIR weighted sequence during the lucid interval is the most accurate predictor of delayed-onset encephalopathy caused by CO poisoning.3 According to a follow-up study in 12 patients, lesion remission on MRI is linked to symptom abatement. In most cases, significant recovery of cognitive impairment was associated with a noticeable, although incomplete, disappearance of the lesions in the white matter over the course of one year. Basal ganglia involvement as shown on the MRI study was associated with poorer prognosis, featuring partial or delayed remission of movement disorders.3 Early treatment with hyperbaric oxygen as a means of preventing or reducing symptoms severity has delivered contradictory results.2,6,7 Despite its therapeutic potential, many patients are not given this treatment due to lack of either a diagnosis or resources at the time of acute intoxication. We reviewed the literature and did not find any formal drug trials; there was only one case report of 12/43 patients treated with GM1 ganglioside. The authors of this case report indicated that there were no differences between the 2 groups.2 Furthermore, there are reports of isolated cases of patients with more or less satisfactory clinical responses to drugs with very diverse action mechanisms, such as nimodipine,8 ziprasidone,9 donezepil,10 and citicoline.11 In the latter study, the patient also received levodopa and selegiline which had lessened her cognitive impairment and parkinsonism significantly, although not completely, after 45 days of treatment. None of these patients were followed up with long-term MRI studies. Remission of dementia-like symptoms in our patient was both faster and more complete than was expected, considering his clinical status and lesions on the MRI. In contrast with published cases, our patient was not treated with hyperbaric oxygen. It might therefore be possible for a patient's condition to improve spontaneously in the natural course of the disease. Although citicoline has no confirmed benefits, its action mechanisms suggest that it would exert a neuroprotective effect in situations of hypoxia and ischaemia, and also favour resolution of cerebral oedema.5 While our case is unquestionably anecdotal, the results were no less positive. Considering that there is no known effective treatment for this entity, we decided to publish this letter so that data from more such patients would be available.
MRI. Increased signal intensity in periventricular white matter. (A) Diffusion-weighted sequence at 2 months after exposure. (B) Diffusion-weighted sequence at 4 months after exposure and at 2 months of treatment. (C) T2-weighted sequence at 2 months after exposure. (D) T2-weighted sequence at 10 months after exposure.
Please cite this article as: Lay-Son Rivas L, Trujillo-Godoy O, Alvarado-Pastenes M. Encefalopatía tardía por monóxido de carbono de curso reversible en un paciente tratado con citicolina. Neurología. 2015;30:453–455.