Gamma knife surgery (GNS) is one of the many techniques used to treat the idiopathic form of trigeminal neuralgia (TN). The aim of this review is to analyse the effectiveness of treatment with GNS in patients affected by recurrent TN.
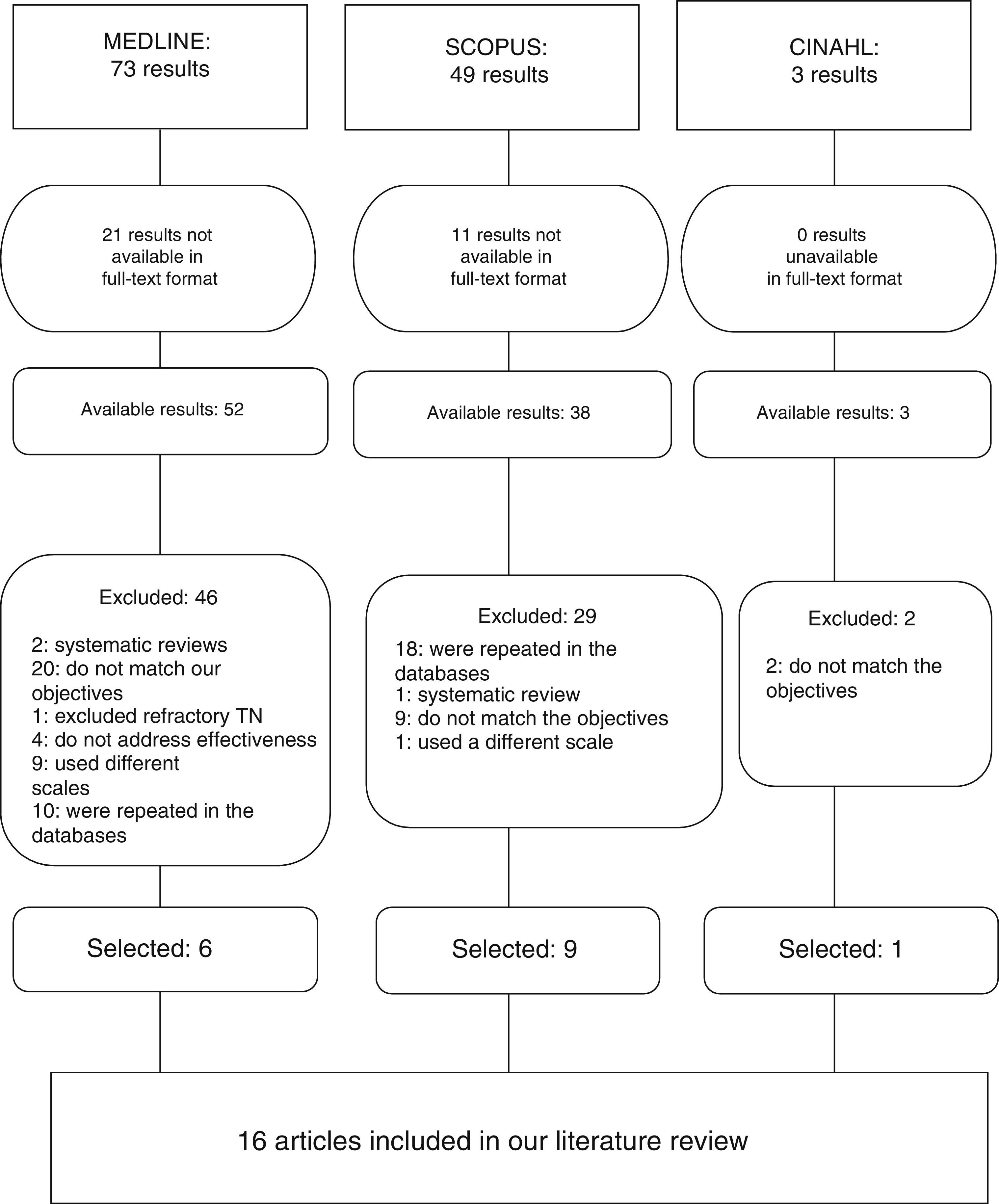
DevelopmentA literature search conducted using MEDLINE, CINAHL, and Scopus in January of 2013 yielded 125 results. After applying the inclusion and exclusion criteria, we selected 16 articles evaluating the effectiveness of GNS for reducing symptoms in patients with recurrent TN. Assessment criteria were degree of pain, time to pain relief, pain maintenance, and disease recurrence after the procedure.
ConclusionsGNS is considered a non-invasive, safe, and effective treatment for patients with idiopathic TN refractory to medication and surgery. It is currently considered the most advanced means of treating this disease.
El bisturí de Rayos Gamma (BRG) es una de las múltiples técnicas de tratamiento para la neuralgia del trigémino idiopática (NT). El objetivo de esta revisión es analizar la efectividad del tratamiento con BRG en los pacientes afectados por la NT recurrente.
DesarrolloSe realizó una revisión bibliográfica en las bases de datos MEDLINE, CINAHL y Scopus en enero del 2013. De 125 resultados obtenidos, y tras aplicar los distintos criterios de inclusión y exclusión, se seleccionaron 16 que evalúan la efectividad del BRG en la sintomatología de los pacientes con NT recurrente. Se evalúan el grado del dolor, el tiempo para el alivio del dolor y el mantenimiento del mismo, así como la recurrencia de la enfermedad posterior al procedimiento.
ConclusionesEl BRG se considera una técnica no invasiva, segura y efectiva para el tratamiento de los pacientes afectados de NT Idiopática refractaria a la medicación y cirugías, siendo considerada a día de hoy como la más avanzada para tratar este tipo de afección.
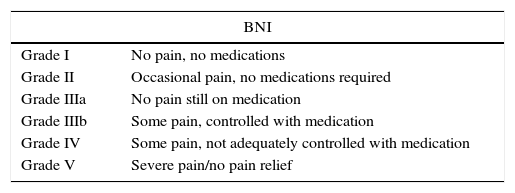
The International Headache Society defines classic trigeminal neuralgia as a unilateral disorder characterised by brief electric shock-like pains, abrupt in onset and termination, limited to the distribution of one or more divisions of the trigeminal nerve. Pain is commonly evoked by trivial stimuli including washing, shaving, smoking, talking and/or brushing the teeth (trigger factors) and frequently occurs spontaneously. Small areas in the nasolabial fold and/or chin may be particularly susceptible to the precipitation of pain (trigger areas). The pain usually remits for variable periods.1 Of the 3 major branches forming the nerve, the mandibular and maxillary nerves are the most frequently affected, whereas the ophthalmic nerve rarely is. While different scales are used to assess pain, the most frequently used is the Barrow Neurological Institute Pain Intensity Scale (BNI) (Table 1).
BNI pain intensity scale.
| BNI | |
|---|---|
| Grade I | No pain, no medications |
| Grade II | Occasional pain, no medications required |
| Grade IIIa | No pain still on medication |
| Grade IIIb | Some pain, controlled with medication |
| Grade IV | Some pain, not adequately controlled with medication |
| Grade V | Severe pain/no pain relief |
BNI: Barrow Neurological Institute.
Estimated worldwide incidence of TN is 15 to 100 cases per 100000 people, and this condition represents a significant percentage of all types of neuralgic facial pain.2,3 TN more commonly affects elderly patients, and the likelihood of presenting this disorder is 2 times higher in women than in men.4
Although its aetiology remains unknown, it is believed to be caused by compression of the nerve root due to vascular malformations or demyelination of the nerve, which causes hypersensitivity of the afferent roots and produces the typical symptoms of the disease.3
Conservative treatment is the first therapeutic approach to manage pain. According to the clinical guidelines drafted by the American Academy of Neurology and the European Federation of Neurological Societies, such drugs as carbamazepine, phenytoin, baclofen, or gabapentin are the most commonly used, although they do no not provide long-term pain relief.5 If pharmacological treatment is not effective enough, surgical treatment may be indicated depending on the patient’ status.
The most frequently used surgical techniques are percutaneous radiofrequency rhizotomy, microvascular decompression, percutaneous retrogasserian glycerol rhizotomy, and the gamma knife (GK). The latter is the most advanced technique and consists of the emission of gamma rays from a cobalt source. We should mention that gamma rays do not cause any damage by passing through the brain. It is only when they all converge on the same point that they demonstrated their therapeutic effect.3
The GK was created by Lars Leksell in 1953, but it was not until recently that imaging techniques provided data sufficient to obtain the best results possible with this treatment.6 The GK focuses beams of gamma radiation on the specific area to be treated. To this end, once the precise target has been pinpointed using imaging-based diagnostic techniques, a stereotactic frame is attached to the scalp of the patient so that the head remains immobile throughout the procedure. The patient is then placed in the machine. Gamma ray beams (or isocentres) then pass through the collimator helmet, which has multiple ports of different diameters, before reaching the target. The procedure makes the technique very precise.
The aim of this review article is to analyse the effectiveness of gamma knife treatment in patients with TN who experience a pain relapse after another treatment (pharmacological or surgical).
DevelopmentWe conducted a literature search in January 2013. Our search strategy was to gather all articles addressing the effectiveness of GK treatment in patients with TN.
We used the MEDLINE, CINAHL, and Scopus databases. For the first 2 databases, we used search terms listed in the Health Sciences Descriptors thesaurus to create the most effective equation possible for locating specific articles. The descriptors selected were ‘treatment outcome’, ‘radiosurgery’, and ‘trigeminal neuralgia’. The Boolean operator used in all 3 databases was ‘AND’.
We used the Medical Subject Headings (MeSH) thesaurus to find the keywords used in the MEDLINE database. The above descriptors were entered as medical subject headings.
We used MeSH terms because they are terms from the medical vocabulary approved by the U.S. National Library of Medicine, which is a controlled list of terminology for articles and science handbooks.
The search of the CINAHL database was conducted following the same steps as on MEDLINE using the MeSH thesaurus, although the terms in this database are called CINAHL Headings. Again, the same descriptors were used.
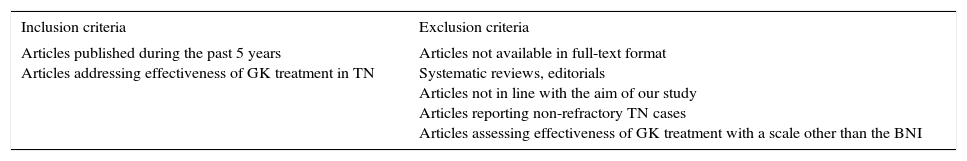
Since the Scopus database has no thesaurus, we used the descriptors ‘treatment outcome’ and ‘trigeminal neuralgia’, and replaced ‘radiosurgery’ with ‘gamma knife surgery’. All terms were searched for in the title, abstract, and keywords fields to make the search algorithms as similar as possible. Table 2 shows the inclusion and exclusion criteria used.
Inclusion and exclusion criteria for our review.
| Inclusion criteria | Exclusion criteria |
|---|---|
| Articles published during the past 5 years Articles addressing effectiveness of GK treatment in TN | Articles not available in full-text format Systematic reviews, editorials Articles not in line with the aim of our study Articles reporting non-refractory TN cases Articles assessing effectiveness of GK treatment with a scale other than the BNI |
Results were as follows:
- –
The search yielded a total of 73 studies in MEDLINE but we excluded 21 because full-access versions were not available. From the remaining 52, we excluded a further 46 articles for different reasons, and included the other 6 in our review (Fig. 1).
- –
The Scopus search yielded 49 studies but we excluded 11 because full-access versions were not available. We excluded 29 from the remaining 38 and selected 9.
- –
We obtained a total of 3 results from the CINAHL database, but excluded 2 (Fig. 1).
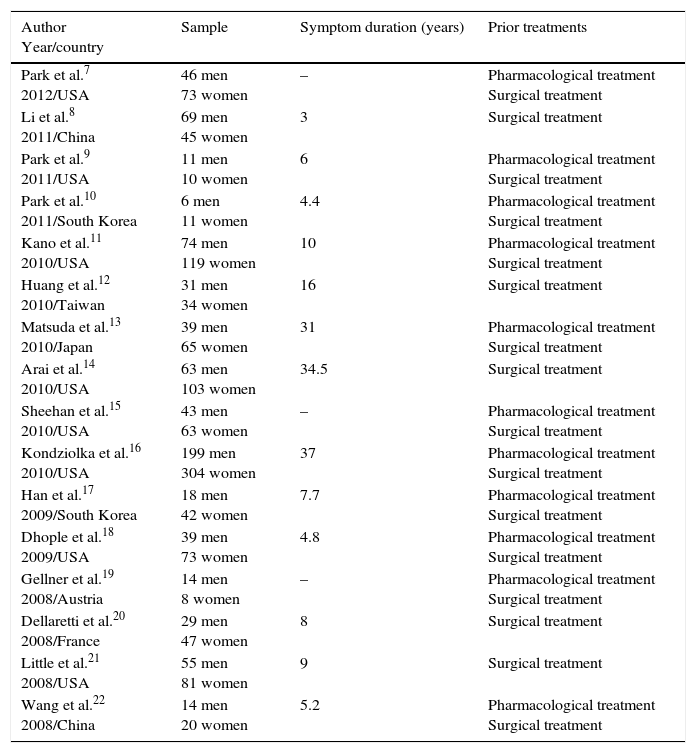
As shown in Tables 3–5, all articles analysed in this review address the effectiveness of GK treatment in patients with TN, in whom previous pharmacological and surgical treatments were unable to prevent a pain relapse. All selected studies have a retrospective design.
Sample, symptom duration, and prior treatment type in each study.
| Author Year/country | Sample | Symptom duration (years) | Prior treatments |
|---|---|---|---|
| Park et al.7 2012/USA | 46 men 73 women | – | Pharmacological treatment Surgical treatment |
| Li et al.8 2011/China | 69 men 45 women | 3 | Surgical treatment |
| Park et al.9 2011/USA | 11 men 10 women | 6 | Pharmacological treatment Surgical treatment |
| Park et al.10 2011/South Korea | 6 men 11 women | 4.4 | Pharmacological treatment Surgical treatment |
| Kano et al.11 2010/USA | 74 men 119 women | 10 | Pharmacological treatment Surgical treatment |
| Huang et al.12 2010/Taiwan | 31 men 34 women | 16 | Surgical treatment |
| Matsuda et al.13 2010/Japan | 39 men 65 women | 31 | Pharmacological treatment Surgical treatment |
| Arai et al.14 2010/USA | 63 men 103 women | 34.5 | Surgical treatment |
| Sheehan et al.15 2010/USA | 43 men 63 women | – | Pharmacological treatment Surgical treatment |
| Kondziolka et al.16 2010/USA | 199 men 304 women | 37 | Pharmacological treatment Surgical treatment |
| Han et al.17 2009/South Korea | 18 men 42 women | 7.7 | Pharmacological treatment Surgical treatment |
| Dhople et al.18 2009/USA | 39 men 73 women | 4.8 | Pharmacological treatment Surgical treatment |
| Gellner et al.19 2008/Austria | 14 men 8 women | – | Pharmacological treatment Surgical treatment |
| Dellaretti et al.20 2008/France | 29 men 47 women | 8 | Surgical treatment |
| Little et al.21 2008/USA | 55 men 81 women | 9 | Surgical treatment |
| Wang et al.22 2008/China | 14 men 20 women | 5.2 | Pharmacological treatment Surgical treatment |
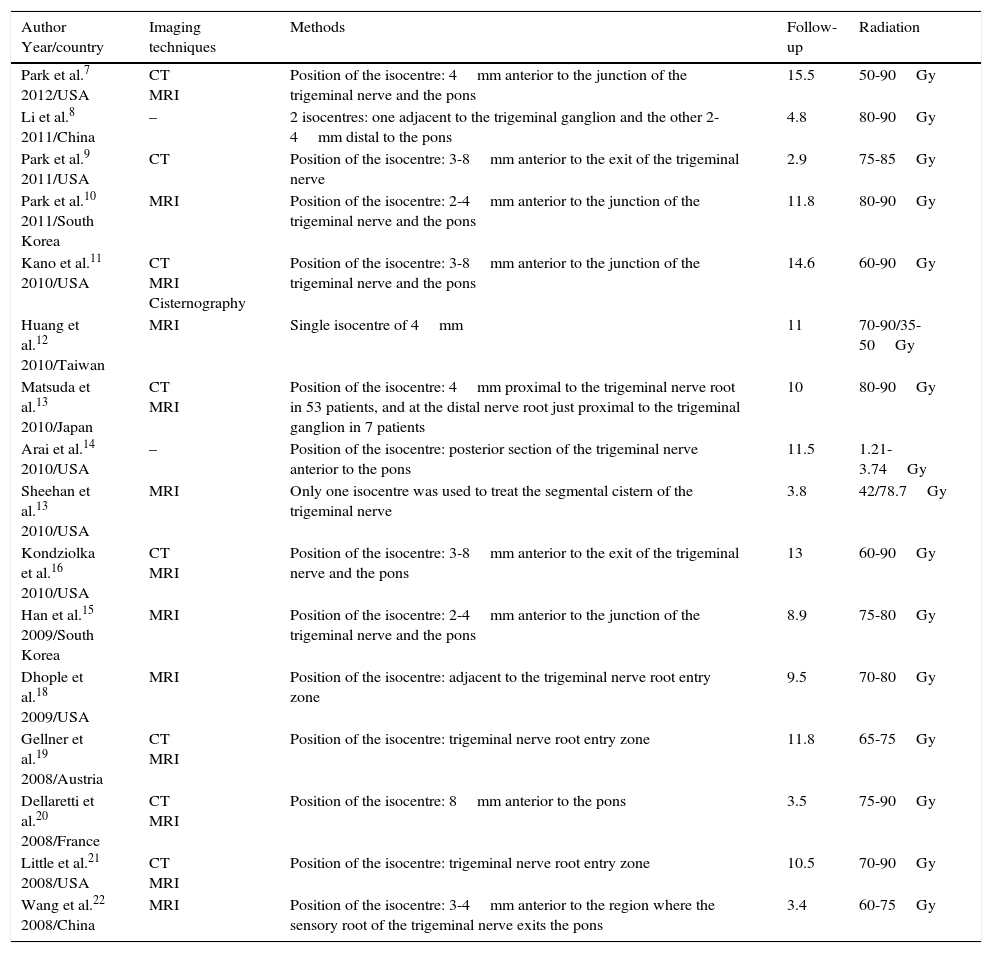
Techniques, methods, follow-up and radiation used in the different studies.
| Author Year/country | Imaging techniques | Methods | Follow-up | Radiation |
|---|---|---|---|---|
| Park et al.7 2012/USA | CT MRI | Position of the isocentre: 4mm anterior to the junction of the trigeminal nerve and the pons | 15.5 | 50-90Gy |
| Li et al.8 2011/China | – | 2 isocentres: one adjacent to the trigeminal ganglion and the other 2-4mm distal to the pons | 4.8 | 80-90Gy |
| Park et al.9 2011/USA | CT | Position of the isocentre: 3-8mm anterior to the exit of the trigeminal nerve | 2.9 | 75-85Gy |
| Park et al.10 2011/South Korea | MRI | Position of the isocentre: 2-4mm anterior to the junction of the trigeminal nerve and the pons | 11.8 | 80-90Gy |
| Kano et al.11 2010/USA | CT MRI Cisternography | Position of the isocentre: 3-8mm anterior to the junction of the trigeminal nerve and the pons | 14.6 | 60-90Gy |
| Huang et al.12 2010/Taiwan | MRI | Single isocentre of 4mm | 11 | 70-90/35-50Gy |
| Matsuda et al.13 2010/Japan | CT MRI | Position of the isocentre: 4mm proximal to the trigeminal nerve root in 53 patients, and at the distal nerve root just proximal to the trigeminal ganglion in 7 patients | 10 | 80-90Gy |
| Arai et al.14 2010/USA | – | Position of the isocentre: posterior section of the trigeminal nerve anterior to the pons | 11.5 | 1.21-3.74Gy |
| Sheehan et al.13 2010/USA | MRI | Only one isocentre was used to treat the segmental cistern of the trigeminal nerve | 3.8 | 42/78.7Gy |
| Kondziolka et al.16 2010/USA | CT MRI | Position of the isocentre: 3-8mm anterior to the exit of the trigeminal nerve and the pons | 13 | 60-90Gy |
| Han et al.15 2009/South Korea | MRI | Position of the isocentre: 2-4mm anterior to the junction of the trigeminal nerve and the pons | 8.9 | 75-80Gy |
| Dhople et al.18 2009/USA | MRI | Position of the isocentre: adjacent to the trigeminal nerve root entry zone | 9.5 | 70-80Gy |
| Gellner et al.19 2008/Austria | CT MRI | Position of the isocentre: trigeminal nerve root entry zone | 11.8 | 65-75Gy |
| Dellaretti et al.20 2008/France | CT MRI | Position of the isocentre: 8mm anterior to the pons | 3.5 | 75-90Gy |
| Little et al.21 2008/USA | CT MRI | Position of the isocentre: trigeminal nerve root entry zone | 10.5 | 70-90Gy |
| Wang et al.22 2008/China | MRI | Position of the isocentre: 3-4mm anterior to the region where the sensory root of the trigeminal nerve exits the pons | 3.4 | 60-75Gy |
Gy: grey; CT: computed tomography; MRI: magnetic resonance imaging.
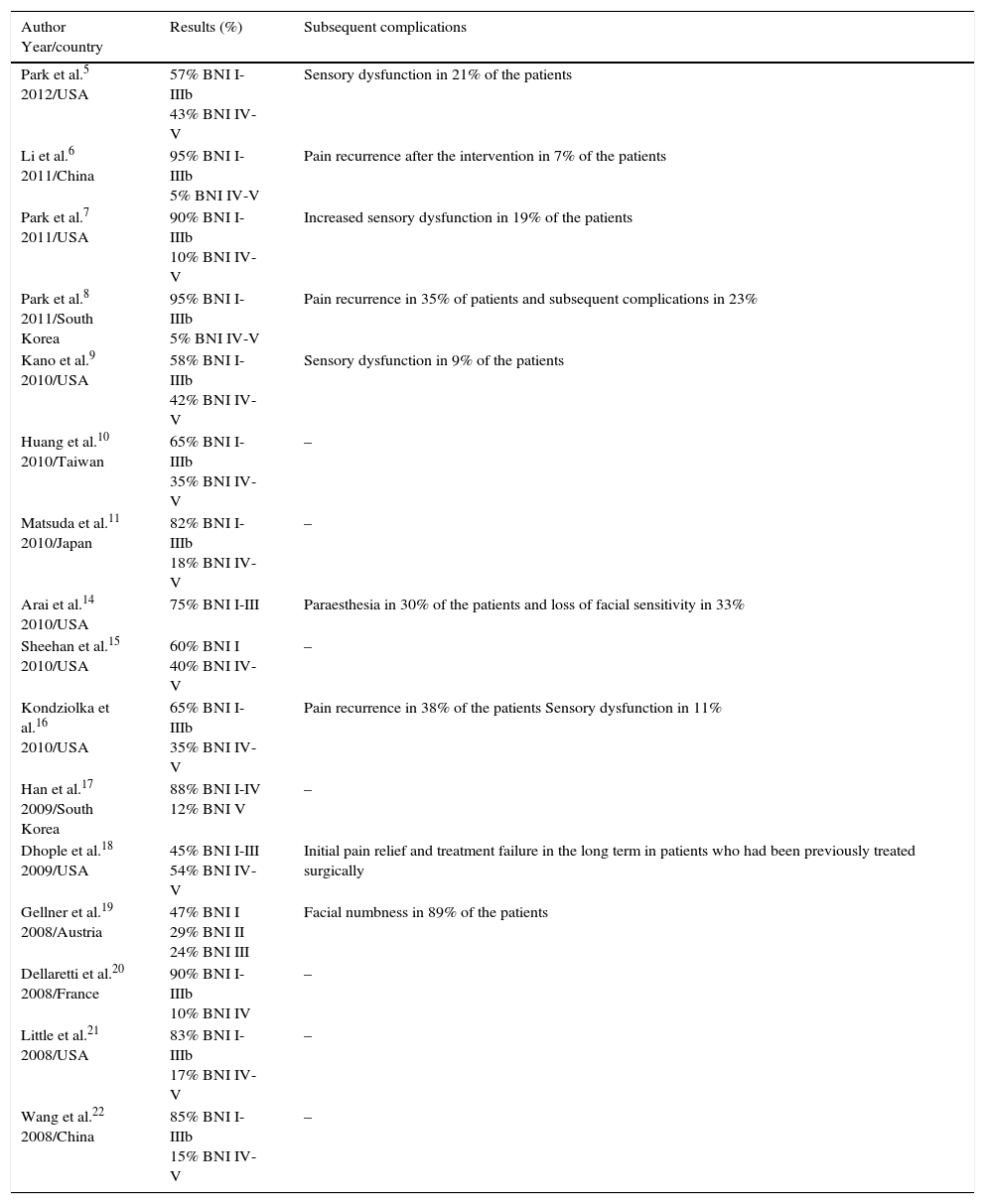
Results and complications observed in the different studies.
| Author Year/country | Results (%) | Subsequent complications |
|---|---|---|
| Park et al.5 2012/USA | 57% BNI I-IIIb 43% BNI IV-V | Sensory dysfunction in 21% of the patients |
| Li et al.6 2011/China | 95% BNI I-IIIb 5% BNI IV-V | Pain recurrence after the intervention in 7% of the patients |
| Park et al.7 2011/USA | 90% BNI I-IIIb 10% BNI IV-V | Increased sensory dysfunction in 19% of the patients |
| Park et al.8 2011/South Korea | 95% BNI I-IIIb 5% BNI IV-V | Pain recurrence in 35% of patients and subsequent complications in 23% |
| Kano et al.9 2010/USA | 58% BNI I-IIIb 42% BNI IV-V | Sensory dysfunction in 9% of the patients |
| Huang et al.10 2010/Taiwan | 65% BNI I-IIIb 35% BNI IV-V | – |
| Matsuda et al.11 2010/Japan | 82% BNI I-IIIb 18% BNI IV-V | – |
| Arai et al.14 2010/USA | 75% BNI I-III | Paraesthesia in 30% of the patients and loss of facial sensitivity in 33% |
| Sheehan et al.15 2010/USA | 60% BNI I 40% BNI IV-V | – |
| Kondziolka et al.16 2010/USA | 65% BNI I-IIIb 35% BNI IV-V | Pain recurrence in 38% of the patients Sensory dysfunction in 11% |
| Han et al.17 2009/South Korea | 88% BNI I-IV 12% BNI V | – |
| Dhople et al.18 2009/USA | 45% BNI I-III 54% BNI IV-V | Initial pain relief and treatment failure in the long term in patients who had been previously treated surgically |
| Gellner et al.19 2008/Austria | 47% BNI I 29% BNI II 24% BNI III | Facial numbness in 89% of the patients |
| Dellaretti et al.20 2008/France | 90% BNI I-IIIb 10% BNI IV | – |
| Little et al.21 2008/USA | 83% BNI I-IIIb 17% BNI IV-V | – |
| Wang et al.22 2008/China | 85% BNI I-IIIb 15% BNI IV-V | – |
BNI: Barrow Neurological Institute Pain Intensity Scale.
Pain relapse may occur because medication did not have the desired effect,9,10,13,15,16,18 previous surgical procedures failed,12,14,19–21 or both, according to Park et al.,7 Li et al.,8 Kano et al.,11 Han et al.,17 and Wang et al.22
All articles in this review reported on patients aged between 60 and 75 years, which confirms that TN affects elderly patients and its incidence increases with age. Although TN has a higher incidence in women than in men, we should highlight that the samples studied by Li et al.,8 Park et al.9 and Gellner et al.19 included more men than women.
Symptom durations ranged from 3 to 37 years, but the results observed after the intervention were similar in all cases, even in the patients with the longest histories of TN.
MRI and CT studies were performed so that the trigeminal nerve could be properly targeted for treatment.7,11,12,16,18–22 However, Park et al.9 used CT and a cisternography, since MRI was contraindicated in one patient due to the presence of metal devices. In addition, Sheehan et al.15 used MRI only to detect vascular impingement in patients treated with GK. Park et al.9 reported that both imaging techniques offer a good anatomical view of the nerve that enables very precise treatment.
Another factor observed was that patients did not have to be admitted for the intervention, therefore avoiding exposure to nosocomial risks. The only exception was the study by Wang et al.,22 who reported that patients were discharged 24hours after radiosurgery.
The number of isocentres used in the radiosurgical procedure and the prescribed dose are factors that varied between studies. The number of isocentres is related to the length of the trigeminal nerve root entry zone for reducing the influencing region,22 and it depends on the precise target to be treated. This number is selected depending on the area to receive radiation, in order to cause the least harm to the patient rather than to improve results.
All authors, except Li et al.,8 used only one isocentre, but they targeted different areas: 2-4mm7,10,17,22 or 3-8mm9,11,16,20 anterior to the junction of the trigeminal nerve and the pons; the trigeminal nerve root entry site immediately adjacent to the pons12,18,19,21; the midposterior portion of the trigeminal nerve, anterior to the pons,14 and the cisternal segment of the trigeminal nerve, located inside the pontocerebellar cistern.15
Higher rates of pain relief were obtained when isocentres were positioned 2-4mm anterior to the junction of the trigeminal nerve and the pons.7,10,17,22 Authors who positioned the isocentre 3-8mm anterior to the junction9,11,16,20 and those who positioned the isocentre on the junction12,18,19,21 reported average pain relief scores. Only the study by Sheehan et al.15 reported a pain relief score below the mean; only 58% of the patients achieved a BNI score of 1.
Unlike the other authors using only one target, Matsuda et al.13 irradiated targets at both the proximal and distal portions in 2 different patient groups. A significant percentage of their patients reported pain reduction, but many also presented facial numbness. The benefits of irradiating this area are therefore questionable.
Furthermore, some of the authors who used 2 isocentres had small patient samples.8,11,16,22 Kano et al.,11 Kondziolka et al.,16 and Wang et al.22 used 2 isocentres of 4mm focused on targets positioned 3-8mm anterior to the junction of the trigeminal nerve and the pons; Li et al.8 used an isocentre focused on the trigeminal ganglion and another at 2-4mm distal to the pons.
We have observed that although the number of isocentres is different between studies, this factor does not influence the results obtained, since differences between percentages were not significant and results remained within the same range. However, we have observed that results can be positive or negative depending on the irradiated area.
Regarding dose, our review shows that authors using a narrower spectrum of high-energy radiation8–10,13,17,18,22 achieved greater success, as reflected by their patients’ high scores on the BNI. On the contrary, the authors who used doses of radiation with a broader spectrum, including lower values, obtained poorer results for pain relief.7,11,12,15,16,19–21 None of the articles provided an explanation of why one dose or another should be used.
Dosing is very important: the higher the treatment dose delivered, the better the pain relief achieved.22 Still, setting the dose at the highest photon energy of the spectrum is recommended, since patients exposed to broader spectra of radiation present a higher risk of complications secondary to the intervention, the most frequent of which are facial numbness and sensory dysfunction.
We should highlight that Park et al.,7,9,10 Kondziolka et al.,16 Dhople et al.,18 Little et al.,21 and Wang et al.22 consider that treatment is successful when a score of BNI I-IIIb is obtained, and fails when scores are BNI IV-V. In contrast, Arai et al.14 and Dellaretti et al.20 define success as BNI I-IIIa and failure as BNI IIIb-V. Lastly, Sheehan et al.15 considered that treatment is successful only when the score is BNI I. These authors’ heterogeneous criteria for defining success or failure on the same BNI scale makes our review's purpose, comparative analysis, quite difficult.
We have observed that only Wang et al.22 differentiate the concepts of relapsing and refractory, unlike the rest of the authors who made no such distinction.
We have also observed, in almost all of the articles, that patients report significant pain relief right after radiosurgery, but the percentage of patients experiencing relief decreases over time.7,9,13,16,18,20 The opposite occurs in the study by Kano et al.11 in which the number of patients experiencing complete pain relief was higher at the end of the follow-up period. We should highlight that although the procedure performed by Kano et al.11 is similar to the one followed in other studies, no reasons have been found as to why their long-term results are better.
Some articles report that long after radiosurgery, patients experience pain recurrence and express dissatisfaction with the results.8–11,13,16 Park et al.9 reported that the variables age, sex, symptom duration, previous surgery, and doses are not associated with pain recurrence after GK treatment.
One important finding in this review is the sensory dysfunction secondary to radiosurgery. In some studies, sensory dysfunction manifested 2 years after the intervention, without causing additional disturbances or motor deficit in the cranial nerves.7,9,11,14,16 However, Kondziolka et al.16 underscore that patients’ quality of life improved since sensory dysfunction decreased pain perception.
Furthermore, Kondziolka et al.16 and Kano et al.11 observed that there were no differences in the maximum dose or the number of isocentres used between patients who developed facial sensory dysfunction and those with no dysfunction after GK treatment. This contrasts with the results published by Huang et al.12 and Park et al.7 who found a significant association between developing trigeminal sensory dysfunction and maximum radiation: the higher the dose, the greater the likelihood of developing sensory dysfunction. Most authors considered this technique to be safe and effective.8,10,16,17,19,20 Dhople et al.18 and Dellaretti et al.20 reported poorer outcomes in patients with prior surgery or previous invasive procedures, and that duration of complete pain relief was statistically higher in patients who had not undergone invasive surgery than in those who had undergone surgery. However, Kano et al.11 mentioned that using a GK after failure of prior surgery achieved pain relief in most patients. Huang et al.,12 Matsuda et al.,13 and Gellner et al.19 observed that, although pain control was satisfactory, the rate of facial numbness (the most frequent complication of this technique) was high after surgery.
Park et al.,7 Huang et al.,12 and Wang et al.22 observed that repeating GK treatment achieved better and longer-lasting pain relief in patients, even when the first intervention obtained positive results.
ConclusionsGamma knife is the surgical technique of choice when previous treatments have failed. The best candidates are elderly patients experiencing a pain relapse despite having undergone prior surgical procedures. They opt for this procedure as a last resort to relieve pain.
We confirm that the factors determining the success of treatment are the dose selection and the radiation area. The most effective radiation dose and radiation area are 70-90Gy and at 2-4mm anterior to the junction of the trigeminal nerve and the pons. The number of isocentres used does not affect the results.
GK treatment lessens pain in most patients with recurrent classic TN, but in some it has been necessary to repeat the procedure or even perform additional surgical interventions, since pain relapse is frequent and relief decreases over time. The reason for this reduction in pain relief is unknown.
We have observed that after the radiosurgical procedure, subsequent complications may emerge, with facial numbness and sensory dysfunction being the most frequent. The risk of presenting this type of complication is very high if the dose used is not appropriate for the patient or if the radiation area is not correct, as these factors determine treatment success.
Despite using the same scale, each study established different score ranges for treatment success and failure, which suggests that even using the same scale does not always allow for reliable comparisons.
GK treatment is painless, performed on an outpatient basis, without general anaesthesia and with the patient awake. The patient therefore recovers immediately and can be discharged right after the procedure.
Finally, we can state that GK treatment is a non-invasive, safe, and effective technique for treating classic TN that is refractory to medication and surgery. Today, GK treatment is considered the newest therapeutic alternative for this disease. Nevertheless, our literature review is based exclusively on retrospective studies; it would be interesting to conduct further randomised trials to confirm the effectiveness of this technique.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Amutio Gutiérrez S, Soto-González M. Efectividad del tratamiento con bisturí de rayos gamma en pacientes afectados por la neuralgia del trigémino idiopática recurrente. Neurología. 2016;31:482–490.